Triple rule-out computed tomography angiography: Evaluation of acute chest pain in COVID-19 patients in the emergency department
2022-09-01SuzanBahadirSonayAydMecitKantarciEdhemUnverErdalKaravaszgCanenbil
INTRODUCTION
Acute chest pain is one of the major complaints among the admissions to the emergency department (ED)[1,2]. In some patients, diagnoses can be made by electrocardiographic (ECG) changes, elevated cardiac laboratory biomarkers, and typical symptoms. However, a normal ECG or cardiac biomarkers do not rule out acute cardiovascular disease and symptoms might be atypical[3]. Moreover, after the novel coronavirus disease 2019 (COVID-19) pandemic, it has been more complicated to make a differential diagnosis list of acute chest pain in the ED. To date, many studies have presented that COVID-19 causes hypercoagulability[4]. Hypercoagulability is attributed to endothelial cell dysfunction, hypoxiainduced pathways, and increased blood viscosity[5]. Therefore, to make a rapid and accurate diagnosis in COVID-19 patients presenting with acute chest pain is of utmost importance.
Triple rule-out computed tomography angiography (TRO CTA) covers all thoracic vascular systems and has advantages in the detection of coronary artery disease, pulmonary thromboembolism (PTE), or acute aortic syndromes[6]. TRO CTA has ability to rule out pathology in all three vascular systems, particularly in COVID-19 patients who have already increased risk of thrombosis and myocardial injury[7].
The aim of this study was to define clinical evidence supporting that TRO CTA is a comprehensive and feasible diagnostic tool in patients with COVID-19 who were admitted to the ED for acute chest pain. Optimizing diagnostic imaging strategies in COVID-19 related thromboembolic events, will help for rapid and noninvasive diagnoses and results will be effective for patients and healthcare systems in all aspects.
“I don’t like to see you fret,” said the little robber-girl; “you ought to look quite happy now; and here are two loaves and a ham, so that you need not starve.” These were fastened on the reindeer, and then the little robber-maiden opened the door, coaxed23 in all the great dogs, and then cut the string with which the reindeer was fastened, with her sharp knife, and said, “Now run, but mind you take good care of the little girl.” And then Gerda stretched out her hand, with the great mitten21 on it, towards the little robber-girl, and said, “Farewell,” and away flew the reindeer, over stumps and stones, through the great forest, over marshes24 and plains, as quickly as he could. The wolves howled, and the ravens screamed; while up in the sky quivered red lights like flames of fire. “There are my old northern lights,” said the reindeer; “see how they flash.” And he ran on day and night still faster and faster, but the loaves and the ham were all eaten by the time they reached Lapland.
THERE was once upon a time a king who was so much beloved by his subjects that he thought himself the happiest monarch1 in the whole world, and he had everything his heart could desire. His palace was filled with the rarest of curiosities, and his gardens with the sweetest flowers, while in the marble stalls of his stables stood a row of milk-white Arabs, with big brown eyes.
MATERIALS AND METHODS
This study was approved by our Institutional Review Board and as it was a retrospective study, written informed consent was waived. No author has any conflict of interest to declare in this study. Our radiology archiving system was searched for patients who applied to the ED for acute chest pain and underwent TRO CTA between September 2020 and January 2021. Patients older than 18 years, who had COVID-19 pneumonia and applied to the emergency department for acute chest pain, and underwent TRO CTA for further evaluation were included in this study. The exclusion criteria were as follows: Unreachable clinical or laboratory data and incomplete documentation of imaging data or inadequate imaging quality. Six of the patients were excluded from the study and the remaining 47 patients fulfilled the inclusion criteria. Medical records were used for the collection of demographics and clinical and laboratory findings. TRO CTA images were evaluated for the presence of the coronary artery disease, PTE, or acute aortic syndromes.
In our center, TRO CTA examination is performed according to the eligibility criteria in the article of Eltabbakh AR
[8].
TRO-CTA protocol
All TRO CTA scans were acquired using a third-generation dual-source CT scanner (Somatom Force, Siemens Healthineers). The protocol begins with a noncontrast prospectively ECG-triggered acquisition between the levels of the carina and the base of the diaphragm for coronary artery calcium scoring. After this, CTA was acquired from the lung apices to the diaphragm after the administration of intravenous contrast. According to patients’ condition, prospectively ECG-triggered, retrospectively ECG-gated, or prospectively ECG-triggered high pitch spiral acquisition was used. An intravenous iodinated contrast material of 60 to 90 mL was administered at an injection rate of 4 to 6 mL/s, followed by a saline chaser of 50 mL. Nitroglycerin or beta-blocker administration was not used. Primarily, the coronary arteries were opacified during image acquisition, while homogeneous enhancement of the pulmonary arteries happened. For the evaluation of the maximum intensity projection of the aorta, coronary and pulmonary arteries, curved planar and volume-rendered reconstructions were obtained; findings were then confirmed on the axial CT source images.
Statistical analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS) for Windows 20 software (IBM SPSS Inc., Chicago, IL, United States). Normal distribution of the data was evaluated using the Kolmogorov-Smirnov test. Numerical variables with a normal distribution are shown as minimummaximum values. Categorical variables are shown as percentages. Differences in normally distributed variables between groups were evaluated using Student’s
-test. Categorical variables were evaluated by the chi-square test between groups.
A two tailed
-value
0.05 was considered statistically significant.
RESULTS
The following day she was dressed from head to foot in silk and velvet16, and they invited her to stay at the palace for a few days, and enjoy herself, but she only begged for a pair of boots, and a little carriage, and a horse to draw it, so that she might go into the wide world to seek for Kay
So he procured16 some bears skins, and covered himself and his horse with them, so that not a particle of gold could be seen, and then rode bravely on into the heart of the forest
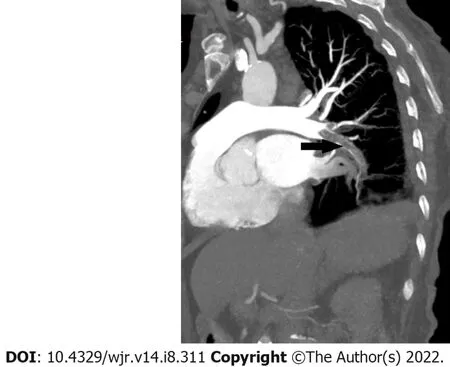
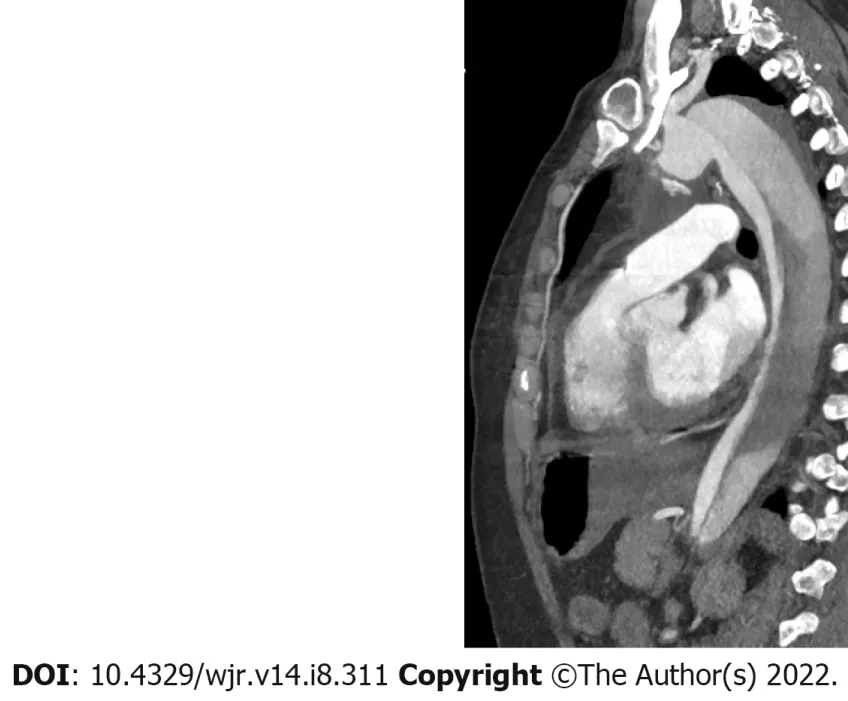
In 31 patients (65.9%), there was not any pathology except for parenchymal findings of COVID-19 pneumonia. PTE was diagnosed in 11 patients (Figure 1), significant stenosis in the coronary arteries diagnosed in 4 (Figures 2 and 3), and dissection in the descending aorta diagnosed in 1 (Figure 4). All coronary artery stenoses were observed in the left anterior descending artery and its branches. The patient with thoracic aortic dissection had a history of previous abdominal aortic dissection.


Forty-one (41/47, 87.2%) of the patients included in this study had a history of hypertension. All patients with hypertension were using antihypertensive drugs and blood pressures were under control. There was no significant relationship between the rates of pathology on CTA and history of hypertension. When patients with findings on CTA and those without findings other than COVID-19 pneumonia on CTA were compared, HT rates were similar (normal group 14/16, 87.5%
pathologic group 27/31, 87%,
= 0.09).
Fourteen patients had a history of diabetes mellitus (DM) (14/47, 29.7%). Eight of these 14 patients were in the group with no imaging findings other than pneumonia, 5 of them were in the PTE group, and 1 was in the acute coronary syndrome group. When compared with those without any imaging findings other than pneumonia on CTA, the DM rate was much higher in the acute coronary syndrome group, particularly in the PTE group (8/31 = 25.8%
6/16 = 37.5%,
= 0.001).
Panguite is an especially exciting discovery since it is not only a new mineral, but also a material previously unknown to science, says Chi Ma, a senior scientist and director of the Geological and Planetary Sciences division s Analytical Facility at Caltech and corresponding author on the paper.
Dyslipidemia was detected in the blood test taken just before (1-3 d) the CTA examination in 22 (22/47, 46.8%) patients. Nine of these patients also had a history of DM. Fourteen of these patients were previously aware of the history of hypercholesterolemia and were using statin derivatives.
The mean total cholesterol level of these patients was 243.9 ± 71.2 mg/dL, and the low-density lipoprotein cholesterol level was 171.5 ± 42.6 mg/dL. All of the patients with significant findings on TRO CTA had a total cholesterol level above 240 mg/dL and low-density lipoprotein cholesterol level above 175 mg/dL. Twelve of these 22 patients were in the group without imaging findings other than pneumonia, 7 were in the PTE detected group, 2 were in the acute coronary syndrome group, and 1 was in the group with aortic dissection. The rate of dyslipidemia was significantly higher in the group with pathology on CTA while compared to those without pathology apart from imaging findings of the pneumonia group (10/16 = 62.5%
12/31 = 38.7%,
0.001).
Nine of the patients included in this study (9/47, 19.1%) had a smoking history. There was not any significant relationship between smoking history and the rate of pathology detected using TRO CTA. Smoking history rates were similar in the group who had pathology on CTA, compared to those without pathology apart from imaging findings of the pneumonia group (3/16 = 18.7%, 6/31 = 19.3%,
0.08).
Two patients (2/47, 4.2%) had a history of cancer (breast cancer and lymphoma). There was not any pathology except for imaging findings of pneumonia detected on CTA in these patients.
The mean PLT value of the whole population was 231.99 ± 64.15 (x 10
/L), the D-dimer value was 854.75 ± 347.65 µg/L , the fibrinogen value was 333.05 ± 66.3 mg/dL, the C-reactive protein (CRP) value was 37.31 ± 2.01 mg/dL, and the erythrocyte sedimentation rate (ESR) value was 55.9 ± 8.2 mm/h (Table 1).
DISCUSSION
Our study revealed that TRO CTA is an effective and non-invasive diagnostic method in COVID-19 patients who were admitted to the ED with acute chest pain. Acute chest pain might be due to pneumonia itself or accompanying vascular events which are related to an increased risk of thrombosis, endothelial dysfunction, and myocardial injury in COVID-19 cases[5,7,8].
In this study, 53 patients who were previously diagnosed with laboratory-proven (real-time PCR) COVID-19 pneumonia and underwent triple rule-out computed tomography angiography due to sudden chest pain between September 2020-January 2021, were retrospectively searched. Six of these patients were excluded from the study because of insufficient quality of the images or because the necessary laboratory and/or clinical data could not be reached. The study population consisted of 47 patients. The creatinine values of 47 patients included in the study were within the physiological range.
To decrease the morbidity and mortality rates in patients.
"The reason deep learning is so successful is because there's very little design that goes into neural networks," said Saenko. "We just let the machine discover the most useful pattern from raw data. We're not going to tell it what to look for. We're not going to tell it any high-level features. We let it search through all of its training data and find those patterns that lead to the highest accuracy in solving the problem."
To the best of our knowledge, there is no research to date that has examined the TRO CTA findings in COVID-19 cases and related them to the clinical features. By examining the TRO CTA findings, performed in the emergency setting of COVID-19 cases, the current study might increase the awareness about the diagnostic utility and effectiveness of the technique, and increase its use.
Performing TRO CTA in every patient with acute chest pain might be challenging and it will not be a cost-effective method. According to our results, accompanying pathologies were mostly seen in COVID-19 patients with DM and dyslipidemia. These data can help the clinicians to select the more eligible patients for TRO CTA examinations. In addition to clinical properties, laboratory parameters can also help to define suitable patients. We showed that PLT, D-dimer, fibrinogen, CRP, and ESR values were higher in COVID-19 cases with additional pathologies other than pneumonia. The relationship between D-dimer and fibrinogen levels with thromboembolic events, and the relationship between CRP/ESR levels with severity of inflammation and the course of disease were previously studied for COVID-19 cases[14]. Hence, it would be a wise choice to prefer TRO CTA examinations in cases with severe inflammation and who are prone to thromboembolic events.
But the wind caught him up, and whirled him through the air so quickly that Medio Pollito could scarcely breathe, and his heart beat against his side till he thought it would break

It has been previously emphasized that COVID-19 increases the risk for pulmonary thromboembolic events, so the thromboprophylaxis is suggested to prevent PTE[12]. Being a common cause of acute chest pain, coronary vascular pathologies can be encountered as a potential differential diagnosis for COVID-19. In addition to being an alternative diagnosis, coronary vascular pathologies can also increase the mortality of COVID-19 cases[13]. The results of the current study demonstrated that pathologies that can be easily diagnosed
the TRO CTA method, such as PTE and coronary vascular pathologies, were also frequently encountered in COVID-19 cases. Therefore, easy, accurate, and rapid diagnosis of accompanying pathologies can help guide treatment and reduce mortality/morbidity rates. Moreover, the effective use of TRO CTA in the ED can enable clinicians to both detect comorbidities and eliminate the mimickers of COVID-19 pneumonia.
The limitations of this study are that it is a retrospective single-center study with a small sample size. Although our center is a third-level university hospital and has a wide variety of facilities, future studies in larger populations are required to support the use of TRO CTA in COVID-19 patients with acute chest pain. Subsequently in times to come, our findings should be confirmed in well-powered clinical studies in multicenter hospitals. Since our study was retrospective, ECG data of some patients could not be accessed.
CONCLUSION
She was delighted with the beautiful deer, and cried to her nurse: Catch it! if you will I will give you this necklace, every pearl of which is worth a kingdom
Twenty-nine (61.7%) of 47 patients were men and 18 (38.3%) of them were women. Mean age was 61.7 ± 13.6 years and median age was 59 years (min-max: 47-84 years).
ARTICLE HIGHLIGHTS
Research background
The aim of this study was to define c linical evidence supporting that triple rule-out computed tomography angiography (TRO CTA) is a comprehensive and feasible diagnostic tool in patients with novel coronavirus disease 2019 (COVID-19) who were admitted to the emergency department for acute chest pain. Optimizing diagnostic imaging strategies in COVID-19 related thromboembolic events, will help for rapid and noninvasive diagnoses and results will be effective for patients and healthcare systems in all aspects.
Research motivation
Acute chest pain in COVID 19 patients becomes more difficult due to increasing differential diagnosis.TRO CTA helps diagnosis by excluding pulmonary thromboembolism (PTE), coronary artery disease,and acute aortic syndrome at the same time.
But what was still more curious, whoever held his finger in the smoke of thekitchen-pot, immediately smelt all the dishes that were cooking on everyhearth in the city--this, you see, was something quite different from therose.
Research objectives
TRO CTA accelerates the precise diagnosis and utilizes the evaluation of the aorta, coronary arteries, and pulmonary vascular systems with a single examination for safe and rapid decisions[9]. However, it requires a larger amount of contrast medium and higher radiation dose, and might not be easily reachable in all centers[10]. But still instead of separate examinations, it is plausible to choose TRO CTA not only for acute thoracic vascular emergencies but for parenchymal pathologies in COVID-19 patients. Because the correct diagnosis of PTE, acute coronary syndrome, and aortic dissection, influences early treatment and thus, it is life-saving[11].
Research methods
Our study is a retrospective study.
Research results
No pathology was detected in 31 of 57 patients included in the study. PTE was detected in 11 patients.The diabetes mellitus rate was much higher in the acute coronary syndrome group, particularly in the PTE group. The rate of dyslipidemia was significantly higher in the group with pathology on CTA while compared to those without pathology apart from imaging findings of the pneumonia group
Our study has shown that TRO CTA is an imaging method that evaluates all thoracic vascular systems at once and gives accurate results in the COVID-19 patient group with acute chest pain, which has been proven to be susceptible to thrombotic events.
Research conclusions
TRO CTA can be a useful method in the differential diagnosis of COVID-19 patients who present to the emergency department with chest pain.
Research perspectives
The use of TRO CTA will reduce mortality and morbidity as it will accelerate the diagnosis and treatment process in the future. Studies will proceed in this direction.
FOOTNOTES
Aydın S, Bahadır S, Kantarcı M, and Karavas E designed the research study; Bahadır S, Ünver E, Şenbil DC, and Karavas E performed the research; Aydın S and Bahadır S contributed new reagents and analytic tools; Aydın S, Karavas E, and Şenbil DC analyzed the data and wrote the manuscript; all authors have read and approved the final manuscript.
This study was approved by our Institutional Review Board (Erzincan Binali Yıldrım University Faculty of Medicine protocol number kaek-ebyu-2020/03/14) and as it was a retrospective study, written informed consent was waived.
If one didn t know it, one would never think that it was you we got from the red cow; will you come home with me now? No, said the merchant, I can t find time just now
Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
No author has any conflict of interest to declare in this study.
No additional data are available.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Turkey
Suzan Bahadir 0000-0002-0019-5851; Sonay Aydın 0000-0002-3812-6333; Mecit Kantarci 0000-0002-1043-6719; Edhem Unver 0000-0002-0322-8102; Erdal Karavas 0000-0001-6649-3256; Düzgün Can Şenbil 0000-0003-0233-7371.
Then he counted again. He needed 20 cents more. Could there be any sacks left any where in town? He had to find four and sell them before the day ended.
Wang LL
Wang TQ
Wang LL
1 Backus BE, Six AJ, Kelder JH, Gibler WB, Moll FL, Doevendans PA. Risk scores for patients with chest pain: evaluation in the emergency department.
2011; 7: 2-8 [PMID: 22294968 DOI: 10.2174/157340311795677662]
2 Lee TH, Goldman L. Evaluation of the patient with acute chest pain.
2000; 342: 1187-1195 [PMID: 10770985 DOI: 10.1056/NEJM200004203421607]
3 Pope JH, Aufderheide TP, Ruthazer R, Woolard RH, Feldman JA, Beshansky JR, Griffith JL, Selker HP. Missed diagnoses of acute cardiac ischemia in the emergency department.
2000; 342: 1163-1170 [PMID: 10770981 DOI: 10.1056/NEJM200004203421603]
4 Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia.
2020; 18: 844-847 [PMID: 32073213 DOI: 10.1111/jth.14768]
5 Gupta N, Zhao YY, Evans CE. The stimulation of thrombosis by hypoxia.
2019; 181: 77-83 [PMID: 31376606 DOI: 10.1016/j.thromres.2019.07.013]
6 Lee HY, Yoo SM, White CS. Coronary CT angiography in emergency department patients with acute chest pain: triple rule-out protocol
dedicated coronary CT angiography.
2009; 25: 319-326 [PMID: 18853277 DOI: 10.1007/s10554-008-9375-4]
7 Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study.
2020; 395: 1054-1062 [PMID: 32171076 DOI: 10.1016/S0140-6736]
8 Eltabbakh AR, Dawoud MA, Langer M, Moharm MA, Hamdy EA, Hamisa MF. ‘Triple-rule-out’CT angiography for clinical decision making and early triage of acute chest pain patients: use of 320-multislice CT angiography.
2019; 50: 1-10 [DOI: 10.1186/s43055-019-0003-1]
9 Chae MK, Kim EK, Jung KY, Shin TG, Sim MS, Jo IJ, Song KJ, Chang SA, Song YB, Hahn JY, Choi SH, Gwon HC, Lee SH, Kim SM, Eo H, Choe YH, Choi JH. Triple rule-out computed tomography for risk stratification of patients with acute chest pain.
2016; 10: 291-300 [PMID: 27375202 DOI: 10.1016/j.jcct.2016.06.002]
10 Yoon YE, Wann S. Evaluation of acute chest pain in the emergency department: "triple rule-out" computed tomography angiography.
2011; 19: 115-121 [PMID: 21464639 DOI: 10.1097/CRD.0b013e31820f1501]
11 Takx RAP, Wichmann JL, Otani K, De Cecco CN, Tesche C, Baumann S, Mastrodicasa D, Litwin SE, Bayer RR 2nd, Nance JW, Suranyi P, Jacobs BE, Duguay TM, Vogl TJ, Carr CM, Schoepf UJ. In-Hospital Cost Comparison of Triple-Rule-Out Computed Tomography Angiography Versus Standard of Care in Patients With Acute Chest Pain.
2020; 35: 198-203 [PMID: 32032251 DOI: 10.1097/RTI.0000000000000474]
12 Sakr Y, Giovini M, Leone M, Pizzilli G, Kortgen A, Bauer M, Tonetti T, Duclos G, Zieleskiewicz L, Buschbeck S, Ranieri VM, Antonucci E. Pulmonary embolism in patients with coronavirus disease-2019 (COVID-19) pneumonia: a narrative review.
2020; 10: 124 [PMID: 32953201 DOI: 10.1186/s13613-020-00741-0]
13 Dan S, Pant M, Upadhyay SK. The Case Fatality Rate in COVID-19 Patients With Cardiovascular Disease: Global Health Challenge and Paradigm in the Current Pandemic.
2020; 1-10 [PMID: 32953401 DOI: 10.1007/s40495-020-00239-0]
14 Eljilany I, Elzouki AN. D-Dimer, Fibrinogen, and IL-6 in COVID-19 Patients with Suspected Venous Thromboembolism: A Narrative Review.
2020; 16: 455-462 [PMID: 33223833 DOI: 10.2147/VHRM.S280962]
杂志排行
World Journal of Radiology的其它文章
- Imaging volumes during COVID-19: A Victorian health service experience
- Progress in interventional radiology treatment of pulmonary embolism: A brief review
- Amebic liver abscess: Clinico-radiological findings and interventional management
- Advanced magnetic resonance imaging findings in salivary gland tumors
- Augmenting prostate magnetic resonance imaging reporting to incorporate diagnostic recommendations based upon clinical risk calculators