Effects of acupuncture on nutritional status in patients in a persistent vegetative state:a prospective randomized controlled study
2022-08-16SHIHanfeng石含峰
SHI Hanfeng (石含峰)
Wuhan Hospital of Traditional Chinese and Western Medicine, Hubei 430000, China
Abstract
Keywords: Acupuncture Therapy; Persistent Vegetative State; Nutritional Status; Hemoglobins; Gastrointestinal Microbiome;Fatty Acids, Volatile
A persistent vegetative state (PVS) refers to a condition in which patients remain unconscious and only maintain the sleep-wake cycle, primordial postural reflexes, and eye movements after a period of brain injury[1]. After severe brain injuries, the sympatheticoadrenomedullary system is activated, the body is in a state of high catabolism, and energy consumption is significantly increased. And due to the “gut-brain interaction”, brain injuries are often combined with gastrointestinal mucosal ischemia-hypoxic damages,gastrointestinal motility disorders, and decreased intestinal mucosal absorption function, causing PVS patients to be prone to malnutrition[2]. Malnutrition can lead to decreased body resistance, affect the repair and functional compensation of the central nervous system,increase the risk of complications such as pulmonary infection and bedsores, prolong the hospitalization time,and increase hospitalization costs and mortality[3].Therefore, paying attention to the nutritional status of patients in PVS and actively providing nutritional support is of great significance for promoting the recovery of patient’s neurological function and improving the prognosis.
Enteral nutrition is the preferred nutrition therapy for patients in PVS, which is beneficial to maintaining the normal secretory function and integrity of the intestinal mucosa, but it cannot inhibit protein catabolism or correct the hypercatabolic state[4-5]. In recent years,acupuncture therapy has been widely used in the clinical treatment of vegetative states, as it can promote the recovery of patients’ brain function and limb movement and improve the level of consciousness[6-8].However, there are few clinical studies on acupuncture improving the nutritional status of patients in a vegetative state. In this study, a prospective randomized controlled trial design was used to study PVS treated with additional Tiao Shen Jian Pi acupuncture therapy(acupuncture for spirit-regulating and spleeninvigorating) on the basis of enteral nutrition support,and the effect on the nutritional status of the patients was observed.
1 Clinical Materials
1.1 Diagnostic criteria for PVS[9]
Unconscious, unable to understand or express language; maintained spontaneous breathing and blood pressure; had the sleep-wake cycle, could open eyes automatically or after stimulation, and could have aimless eye tracking movements; the vegetative state lasted for more than a month.
1.2 Inclusion criteria
Those who met the above diagnostic criteria for PVS;with clear etiology and a stable condition after treatment; aged 20 to 70 years old; patients’ families agreed to participate in this clinical trial and signed informed consent.
1.3 Exclusion criteria
Patients in a coma or with locked-in syndrome; those with a medical history of Parkinson disease, Alzheimer disease, or epileptic seizure confirmed by the past medical records or the patient’s family members; those in PVS for more than one year; patients with craniocerebral trauma and did not undergo cranioplasty after decompressive craniectomy; those who had severe injuries of other organs or tissues such as thoracoabdominal injuries and spinal fractures; those had severe diseases of heart, liver, or kidney.
1.4 Elimination and shedding criteria
Dropped out during the trial due to those family members’ requirements; those presenting with severe adverse reactions or got worse in the disease condition during the study; with incomplete clinical materials.
1.5 Statistical methods
All data were statistically analyzed by the SPSS version 22.0 statistical software. The counting data were expressed as case numbers and analyzed by the Chi-square test. Measurement data in normal distribution and having homogeneous variance were expressed as mean ± standard deviation (±s) and analyzed byt-test. Measurement data in non- normal distribution or without homogeneous variance were analyzed by non-parametric test.P<0.05 indicated a statistically significant difference.
1.6 General data
A total of 66 patients in PVS were collected from our hospital between January 2016 and November 2020. All patients were randomly divided into a control group and an observation group by the random number table method, with 33 cases in each group. In this trial, three patients in the control group and two patients in the observation group dropped out due to aggravation of the condition. A total of 61 patients finished the study,with 30 cases in the control group and 31 in the observation group. There were no statistical differences in gender, age, duration of vegetative state, or cause of PVS between the two groups (P>0.05), indicating that they were comparable (Table 1).
2 Treatment Methods
2.1 Control group
The patients in the control group received conventional treatments such as improving cerebral metabolism and microcirculation, nourishing nerves,consciousness-promoting drugs, and anti-epileptics,combined with enteral nutrition support at the same time. The treatments lasted for 8 weeks.
2.2 Observation group
The observation group was treated with additional Tiao Shen Jian Pi acupuncture therapy based on the same interventions in the control group.
Points: Baihui (GV20), Yintang (GV29), bilateral Tianshu (ST25), Zusanli (ST36), Shangjuxu (ST37) and Sanyinjiao (SP6)[10].
Methods: The patient took a supine position with points exposed. After routine disinfection, acupuncture needles of 0.25 mm in diameter and 40 mm in length were inserted, avoiding the injured site of the skull.Baihui (GV20) was subcutaneously punctured by 0.8 Cun in depth. Yintang (GV29) was subcutaneously punctured by 0.5 Cun in depth with the skinpinching-up insertion method. Tianshu (ST25) was perpendicularly punctured by 1.0 Cun in depth with the skin-stretching needle insertion method. The rest of the points were all perpendicularly punctured by 1.0 Cun in depth with the finger-pressing needle insertion method.After the arrival of Qi (Deqi), even reinforcing-reducing manipulation was applied. The needles were retained for 30 min. The treatment was performed once a day,5 times a week, for 8 weeks in total.

Table 1. Comparison of the general data between the two groups
3 Therapeutic Efficacy Observation
3.1 Observation items
3.1.1 Nutrition-related blood indicators
Before and after treatment, fasting venous blood was collected in the morning to determine the levels of total protein (TP), prealbumin (PA), albumin (Alb), and hemoglobin (Hb).
3.1.2 Upper arm circumference and skinfold thickness of the triceps brachii
Before and after treatment, the arm circumference was measured at the thickest part of the patient’s biceps brachii. The physician used the index finger and thumb to lift up the skin and subcutaneous fat to form a fold at the midpoint of the line connecting the ulna olecranon and the posterior acromion of the upper arm.The index finger and thumb were 3 cm apart, and the thickness of the pinched skinfold was measured.
3.1.3 Intestinal flora contents
Before and after treatment, 3 g of fresh wet feces of the patients were collected, diluted, and droppingseeded for bacterial culture. The contents ofBifidobacterium,Lactobacillus, andEnterococcuswere determined by the live bacteria plate counting method.
3.1.4 Fecal short-chain fatty acids contents
Before and after treatment, 3 g of fresh wet feces of patients were collected, and the total content of short-chain fatty acids, and the contents of acetic acid and butyric acid in feces were determined by gas chromatography-mass spectrometry.
3.2 Results
3.2.1 Comparison of the nutrition-related blood indicators
Before treatment, there were no statistical differences in the levels of TP, PA, Alb, or Hb between the two groups (P>0.05). After treatment, the levels of TP, PA, Alb, and Hb in the control group were decreased(P<0.05), while the levels of TP, PA, Alb, and Hb in the observation group were not statistically different from those before treatment (P>0.05) and were all higher than those in the control group (P<0.05). It is shown in Table 2.
Table 2. Comparison of nutrition-related blood indicators between the two groups ( ±s)

Table 2. Comparison of nutrition-related blood indicators between the two groups ( ±s)
Note: TP=Total protein; PA=Prealbumin; Alb=Abumin; Hb=Hemoglobin; compared with the same group before treatment, 1) P<0.05;compared with the control group after treatment, 2) P<0.05
Group n Time TP (g/L) PA (mg/L) Alb (g/L) Hb (g/L)Observation 31 Before treatment 65.33±7.62 149.14±33.98 38.31±5.64 128.95±19.30 After treatment 62.65±7.982) 145.48±31.522) 36.00±5.472) 122.57±15.612)Control 30 Before treatment 67.93±7.40 153.24±30.65 40.48±6.16 129.25±19.57 After treatment 55.81±9.261) 120.15±23.111) 31.03±4.081) 100.77±13.521)
3.2.2 Comparison of the upper arm circumference and skinfold thickness of triceps brachii
Before treatment, there were no statistical differences in the upper arm circumference or skinfold thickness of triceps brachii between the two groups(P>0.05). After treatment, the upper arm circumference and skinfold thickness of triceps brachii in both groups decreased (P<0.05) and were higher in the observation group than in the control group (P<0.05). It is shown in Table 3.
3.2.3 Comparison of the intestinal flora contents
Before treatment, there were no statistical differences in the contents ofBifidobacterium,Lactobacillus,orEnterococcusin feces between the two groups (P>0.05). After treatment, the contents ofBifidobacteriumandLactobacillusin the control group decreased (P<0.05), and the content ofEnterococcusincreased (P<0.05). In the observation group, the contents ofBifidobacteriumandLactobacillusin feces increased (P<0.05), and the content ofEnterococcusdecreased (P<0.05). In addition, the contents ofBifidobacteriumandLactobacillusin the observation group were higher than those in the control group(P<0.05), and the content ofEnterococcuswas lower than that in the control group (P<0.05). It is shown in Table 4.
3.2.4 Comparison of the fecal short-chain fatty acids contents
Before treatment, there were no statistical differences in the total content of fecal short-chain fatty acids or the contents of acetic acid and butyric acid in feces between the two groups (P>0.05). After treatment,the total content of fecal short-chain fatty acids and the contents of acetic acid and butyric acid in the control group decreased (P<0.05). In the observation group, the total content of fecal short-chain fatty acids and the contents of acetic acid and butyric acid in feces increased (P<0.05), and all contents were higher than those in the control group (P<0.05). It is shown in Table 5.
Table 3. Comparison of the upper arm circumference and skinfold thickness of triceps brachii between the two groups ( ±s)
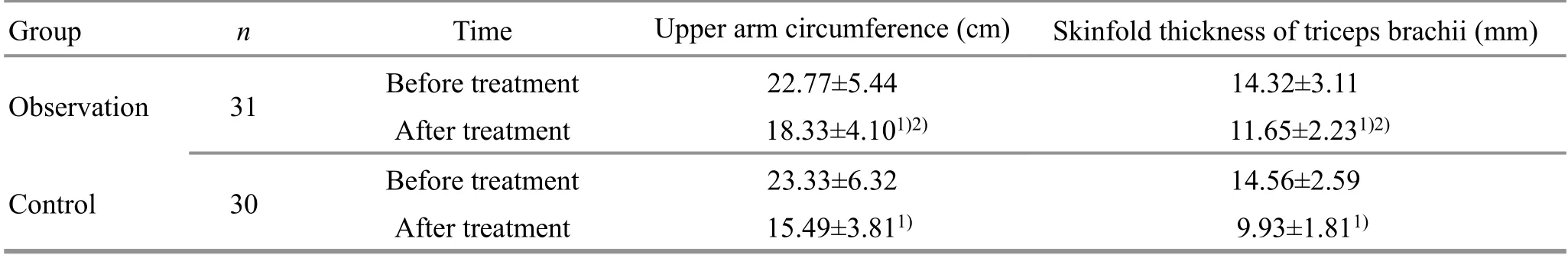
Table 3. Comparison of the upper arm circumference and skinfold thickness of triceps brachii between the two groups ( ±s)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Time Upper arm circumference (cm) Skinfold thickness of triceps brachii (mm)Observation 31 Before treatment 22.77±5.44 14.32±3.11 After treatment 18.33±4.101)2) 11.65±2.231)2)Control 30 Before treatment 23.33±6.32 14.56±2.59 After treatment 15.49±3.811) 9.93±1.811)
Table 4. Comparison of the intestinal flora contents between the two groups ( ±s logCFU/g)
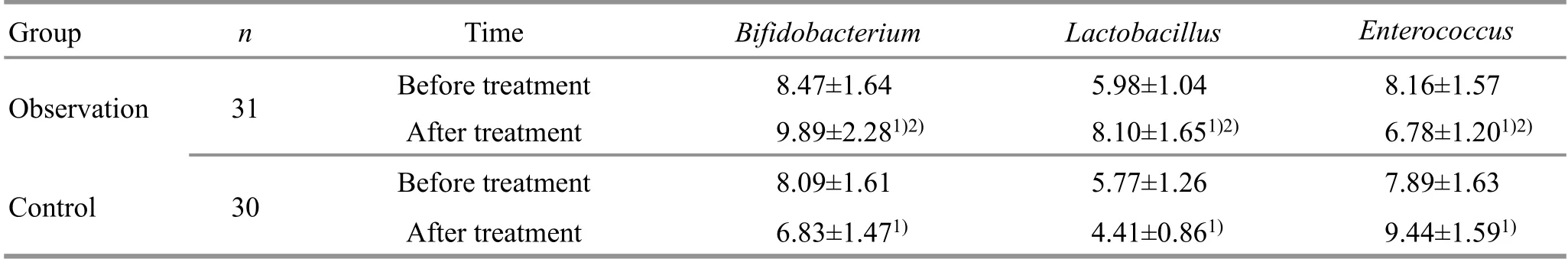
Table 4. Comparison of the intestinal flora contents between the two groups ( ±s logCFU/g)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Time Bifidobacterium Lactobacillus Enterococcus Observation 31 Before treatment 8.47±1.64 5.98±1.04 8.16±1.57 After treatment 9.89±2.281)2) 8.10±1.651)2) 6.78±1.201)2)Control 30 Before treatment 8.09±1.61 5.77±1.26 7.89±1.63 After treatment 6.83±1.471) 4.41±0.861) 9.44±1.591)
Table 5. Comparison of the fecal short-chain fatty acids contents between the two groups ( ±s μg/g)
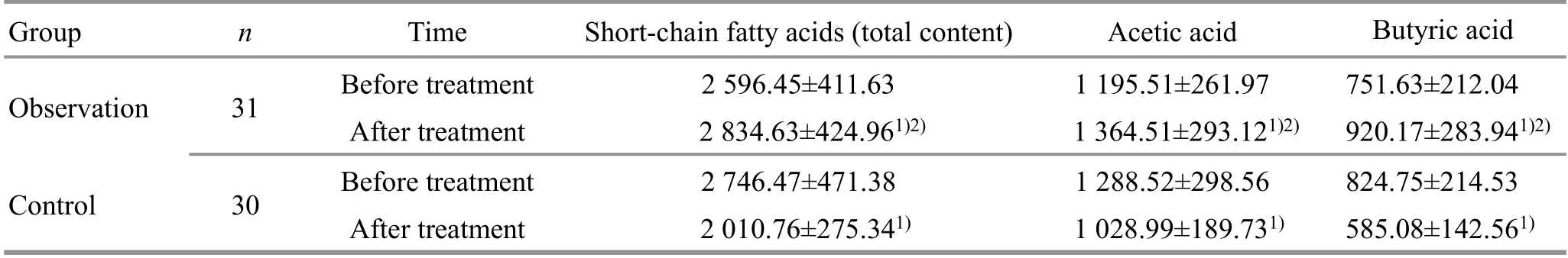
Table 5. Comparison of the fecal short-chain fatty acids contents between the two groups ( ±s μg/g)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Time Short-chain fatty acids (total content) Acetic acid Butyric acid Observation 31 Before treatment 2 596.45±411.63 1 195.51±261.97 751.63±212.04 After treatment 2 834.63±424.961)2) 1 364.51±293.121)2) 920.17±283.941)2)Control 30 Before treatment 2 746.47±471.38 1 288.52±298.56 824.75±214.53 After treatment 2 010.76±275.341) 1 028.99±189.731) 585.08±142.561)
4 Discussion
Chinese medicine believes that PVS belongs to the category of coma and unconsciousness. It is mostly caused by craniocerebral trauma or aging and physical infirmity, which result in blood stasis blocking collaterals,phlegm-turbidity clouding the orifices, deficiency of Qi and blood, and insufficient nourishment of essential Qi and spirit[11]. The location of PVS is in the brain,involving the spleen, heart, and kidney. The insufficiency of spleen and kidney and the deficiency of Qi and blood are the core, while phlegm and static blood blocking collaterals are the superficial[12]. Patients in PVS are bedridden for a long time, which impairs Qi.Besides, they are unable to eat and swallow, which inevitably affects the transportation and transformation function of the spleen and its function to ascend the clear. The deficiency of spleen and stomach will cause the lack of supply for Qi and blood generation and transformation, resulting in insufficient nourishment of the sea of marrow and spirit, muscle dystrophy, and body emaciation. Therefore, in clinical practice, PVS is more common in the syndrome of Qi and blood deficiency, and the treatment should pay equal attention to regulating the spirit and refreshing the brain, benefiting Qi and replenishing blood[13].
Tiao Shen Jian Pi acupuncture therapy is an acupuncture method that pays equal attention to the treatment of the spirit and the spleen proposed by Professor SUN Jianhua based on his years of clinical experience. It is mainly used for the treatment of psychosomatic diseases such as irritable bowel syndrome, functional dyspepsia, and gastroesophageal reflux[14]. Research has confirmed that Tiao Shen Jian Pi acupuncture therapy can improve the mental state and intestinal function of patients by regulating the functions of limbic system-neocortex-related brain regions and hypothalamic-pituitary-adrenal axis, so as to achieve the effect of “treating spirit and physical body simultaneously”[15].
Patients in PVS due to the long-term bedridden state,usually demonstrate spiritual and physical deficiency.Therefore, we used Tiao Shen Jian Pi acupuncture therapy in this study to observe its effect on patients’nutritional status. In the point prescription, Baihui(GV20) and Yintang (GV29) are located on the head and face, closely related to the brain, and are the key points for invigorating the brain and benefiting the spirit[16].Tianshu (ST25) is the Front-Mu Point of the large intestine. And Shangjuxu (ST37) is the Lower He-Sea Point of the large intestine. Both points can unblock and regulate the intestine and Qi-flow for dispelling stagnation, thus considered the key points for the treatment of gastrointestinal diseases. Zusanli (ST36) is the He-Sea Point of the Stomach Meridian and the Lower He-Sea Point of the stomach, with the effect of invigorating spleen-stomach and tranquillization and nourishing blood[17-18]. Sanyinjiao (SP6) is the crossing point of the Spleen Meridian, Liver Meridian, and Kidney Meridian. It can invigorate the spleen, regulate the liver, benefit the kidney, and nourish blood for tranquillization. The combination of the above points produces the effect of regulating spirit and strengthening the brain, invigorating the spleen, and harmonizing the stomach, benefiting Qi and nourishing blood. The results of this study showed that after treatment, the nutrition-related blood indicators in the control group decreased, while there were no significant changes in the observation group, which was statistically different from the control group. The upper arm circumference and skinfold thickness of triceps brachii in both groups decreased, and the values of these two items in the observation group were higher than those in the control group. It is suggested that Tiao Shen Jian Pi acupuncture therapy can stabilize the nutrition-related blood indicators in patients in PVS, and delay the reduction of upper arm circumference and skinfold thickness of the triceps brachii.
Intestinal flora can directly affect intestinal absorption function and regulate brain function through the brain-gut axis. Intestinal flora forms a natural barrier in the intestinal mucosa, increasing the absorption area of the intestinal mucosa and improving intestinal absorption function[19]. If the flora related to food digestion and absorption is reduced, even if food intake is sufficient, malnutrition may be caused due to insufficient digestion and absorption. If the flora with the effect of inhibiting inflammation is reduced, it will lead to chronic intestinal inflammation, aggravating the intestinal epithelial injury, causing chronic diarrhea and affecting the absorption of nutrients[20-22]. Intestinal flora is also a key component of the brain-gut axis. Its metabolites (lipopolysaccharide, etc.) can penetrate the blood-brain barrier and have a direct impact on the brain[23]. It can also communicate with the brain through the hypothalamic-pituitary-adrenal axis,immune-modulation, tryptophan metabolism, and production of neuroactive compounds[24]. This indicates that the regulation of intestinal flora may be the target of improving the intestinal absorption function,regulating the excitability of the sympathoadrenal system, and correcting the hypercatabolism state of patients in PVS.
Short-chain fatty acids are the metabolites of intestinal flora, which can provide energy for the intestinal mucosa and intestinal flora, protect the intestinal mucosal barrier, reduce the level of intestinal inflammation, improve the structure of intestinal flora,and enhance gastrointestinal digestion, absorption, and motor function. Short-chain fatty acids mainly include acetic acid and butyric acid. Among them, acetic acid is the main substrate for cholesterol synthesis and lipogenesis and is metabolized by the liver as the energy source for surrounding tissues[25]. Butyric acid can be absorbed and utilized by colonic epithelial cells and is the preferred source of energy for the colon and cecum.It participates in gluconeogenesis, ketone body generation, and triacylglycerol synthesis, affecting saccharometabolism and lipid metabolism. Besides, it has a positive effect on maintaining the stability of the intestinal environment and preventing intestinal inflammation[26-27].
In this study, the intestinal flora and fecal short-chain fatty acids contents of patients in the two groups were analyzed before and after treatment. The results showed that after treatment, the contents ofBifidobacteriumandLactobacillusin the control group decreased, and the content ofEnterococcusincreased.Results in the observation group were the opposite, and the content of flora was more beneficial than that of the control group. In the control group, the total content of fecal short-chain fatty acids and the contents of acetic acid and butyric acid in feces decreased.Results in the observation group were the opposite, and the contents were all higher than those in the control group. It is suggested that Tiao Shen Jian Pi acupuncture therapy can up-regulate the contents ofBifidobacteriumandLactobacillusand short-chain fatty acids in the intestinal tract and reduce the content ofEnterococcus. The mechanism of Tiao Shen Jian Pi acupuncture therapy in improving the nutritional status of patients in PVS may be related to this.
In summary, acupuncture can improve nutritionrelated blood indicators in patients in PVS and delay the decrease of upper arm circumference and skinfold thickness of the triceps brachii, which may be related to its regulation of intestinal flora and fecal short-chain fatty acids contents.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
There was no project fund supporting this study.
Statement of Informed Consent
Informed consent was obtained from the family members of all individual participants.
Received: 27 May 2021/Accepted: 18 August 2021
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Research on clinical application of manual therapy to tumor-related adverse reactions
- Observation on efficacy of thumbtack needle combined with pediatric Tuina for constipation in children caused by liver depression and Qi stagnation
- Clinical study on Tuina plus physical agents for lateral collateral ligament injury of ankle in gymnasts
- Efficacy of knee-balancing manipulation plus heat-sensitive moxibustion for knee osteoarthritis and its influence on CTX-Ⅰ, TRACP-5b,ADAMTS-4, and MMP-3
- Clinical observation of warm needling moxibustion plus lumbar traction for lumbar disc herniation
- Clinical observation of acupuncture plus acupoint sticking therapy for insomnia and its influence on subjective and objective sleep indicators
