Percutaneous transhepatic cholangiography vs endoscopic ultrasound-guided biliary drainage: A systematic review
2022-08-11ZeinabHassanEyadGadour
Zeinab Hassan, Eyad Gadour
Abstract BACKGROUND Percutaneous transhepatic cholangiography is a diagnostic and therapeutic procedure that involves inserting a needle into the biliary tree, followed by the immediate insertion of a catheter. Endoscopic ultrasound-guided biliary drainage(EUS-BD) is a novel technique that allows BD by echoendoscopy and fluoroscopy using a stent from the biliary tree to the gastrointestinal tract.AIM To compare the technical aspects and outcomes of percutaneous transhepatic BD(PTBD) and EUS-BD.METHODS Different databases, including PubMed, Embase, clinicaltrials.gov, the Cochrane library, Scopus, and Google Scholar, were searched according to the guidelines for Preferred Reporting Items for Systematic reviews and Meta-Analyses to obtain studies comparing PTBD and EUS-BD.RESULTS Among the six studies that fulfilled the inclusion criteria, PTBD patients underwent significantly more reinterventions (4.9 vs 1.3), experienced more postprocedural pain (4.1 vs 1.9), and experienced more late adverse events (53.8%vs 6.6%) than EUS-BD patients. There was a significant reduction in the total bilirubin levels in both the groups (16.4-3.3 μmol/L and 17.2-3.8 μmol/L for EUSBD and PTBD, respectively; P = 0.002) at the 7-d follow-up. There were no significant differences observed in the complication rates between PTBD and EUSBD (3.3 vs 3.8). PTBD was associated with a higher adverse event rate than EUSBD in all the procedures, including reinterventions (80.4% vs 15.7%, respectively)and a higher index procedure (39.2% vs 18.2%, respectively).CONCLUSION The findings of this systematic review revealed that EUS-BD is linked with a higher rate of effective BD and a more manageable procedure-related adverse event profile than PTBD. These findings highlight the evidence for successful EUS-BD implementation.
Key Words: Percutaneous transhepatic cholangiography; Endoscopic ultrasound; Biliary drainage;Obstructive cholangiopathy
INTRODUCTION
Endoscopic transpapillary biliary drainage (BD) is the preferred approach for biliary decompression in patients with unresectable pancreatic cancer and obstructive jaundice[1]. Percutaneous transhepatic cholangiography (PTC) is a diagnostic and therapeutic procedure that involves inserting a needle into the biliary tree, followed by immediately inserting a catheter to achieve percutaneous BD. During the procedure, contrast is injected into one or more bile ducts (cholangiography) and sometimes into the duodenum. PTC can be performed using fluoroscopic guidance alone or using both fluoroscopic and ultrasound guidance[2,3].
In cases of suspected malignant biliary stricture, imaging alone may not be sufficient to provide a precise diagnosis. PTC was first introduced several decades ago to visualize biliary obstructions, treat malignant obstructive jaundice palliatively, and access BD[4]. Fine needle aspiration (FNA), brush cytology, and forceps biopsy have been performed using percutaneous biliary catheterization during PTC since the 1980s[5]. For biliary stenosis, endoscopic retrograde cholangiopancreatography (ERCP)has recently been recognized as a reliable diagnostic and therapeutic procedure.
Endoscopic retrograde BD (ERBD) is the most commonly used method of biliary decompression in patients with blockage of the distal central bile duct. This technique has a success rate of 90%-95% in the United States[6]. Altered anatomy, presenting pathology (tumor infiltration, impacted stone, and duodenal compression by a pancreatic pseudocyst), previous surgery, or variations in normal anatomy(periampullary diverticula and tortuous ducts) can contribute to the failure of ERBD. The failure rate of ERBD is 6%-7% in cases with obstructive jaundice caused by a blockage or altered anatomy[7].Percutaneous transhepatic BD (PTBD) has a lower risk of complications than surgical decompression,but it is associated with complications such as fistula formation, repeat intervention, recurrent infection,and the requirement for long-term external catheter drainage, which contribute to a low quality of life[8]. Although PTBD is associated with severe morbidity and mortality, the only relative contraindication of PTBD is perihepatic ascites[6-9]. Furthermore, PTBD usually requires separate surgery after the failure of ERCP BD, thereby increasing the morbidity associated with biliary stasis.
Endoscopic ultrasound-guided BD (EUS-BD) has become more widely used as an alternative to PTBD in patients with anatomical abnormalities, which make endoscopic transpapillary insertion of a biliary stent difficult[10]. It offers advantages of being compatible with anatomic internal drainage, being more comfortable, and resulting in a recovery associated with fewer complications and reduced expenditure[11].
EUS is an extremely useful imaging method for examining the gastrointestinal luminal wall and surrounding tissues. The proximity of the EUS probe to the area of interest enables high-resolution imaging and EUS-guided FNA tissue collection in real time. EUS has become a crucial diagnostic technique due to its high-quality imaging and FNA capacity and is also used as a treatment tool.However, until recently, its use was limited to the introduction of various drugs[12,13]. The therapeutic uses of EUS have been expanded due to larger channel echoendoscopes, which combine the benefits of real-time ultrasound and fluoroscopy imaging with the use of ERCP-based devices and procedures,such as EUS-BD. In 1996, Wiersemaet al[14] first reported EUS-guided diagnostic cholangiography and in 2001, Giovanniniet al[10] first reported EUS-BD in a patient with pancreatic cancer, establishing a choledochoduodenal fistula with a needle knife followed by transduodenal stenting.
These early reports were followed by modified techniques and expanded indications, such as EUSguided hepatic gastrostomy with stent placement[15], transduodenal EUS-rendezvous (EUS-RV) biliary access[16], and EUS-guided choledocholithiasis therapy with the creation of a neo papilla[17]. Since then, several studies have reported modifications to these techniques, including the use of a covered metal stent as a conduit for interventional endoscopic procedures in the bile duct[18,19]. Few studies have compared EUS-BD and PTBD in failed ERCP cases in terms of success rate and adverse event profile[20]; therefore, we performed a systematic review of the relevant literature to investigate the combined efficacy and adverse effects of EUS-BD and PTBD.
MATERIALS AND METHODS
Literature search
This systematic review was conducted using an electronic search of different databases, including PubMed, Embase, clinicaltrials.gov, the Cochrane library, Scopus, and Google Scholar using the guidelines for Preferred Reporting Items for Systematic reviews and Meta-Analyses[21]. Two investigators independently searched for the following key terms: all field “failed EUS”, all field“Percutaneous biliary drainage”, and all field “EUS-guided biliary drainage”. All the three search headings were connected using the Boolean operator “AND”. Studies published in English comparing PTBD with EUS-BD were chronologically limited to those published from their inception to October 2021. After completing the literature search, the references were imported to Endnote citation manager(Endnote X9) for removing any duplicates, following which the abstracts were screened for potential relevance by two independent investigators. This study included intervention studies, retrospective or prospective observational studies, case reports, randomized controlled trials, and published abstracts that reported at least some adverse events. And this study also cited high-quality articles in Reference Citation Analysis (https://www.referencecitationanalysis.com).
Letters, comments, seminar proceedings, and animal studies were excluded from our analysis.Moreover, only human studies were included and limited to the English language. Publications judged to be potentially relevant underwent a full text assessment by two independent investigators to determine their inclusion. Disagreements regarding study eligibility were resolved by consensus or adjudication between the investigators.
Data extraction
The baseline study details, including study identifiers, such as first author, publication year, title, and country, and study-specific methodological data, such as sample size, study design, single-centervsmulticenter study types, and healthcare setting, are presented in Table 1. Technical and clinical success rates, including the total number of patients enrolled, number of patients in each arm, mean age, sex ratio, comorbidity index, mean preprocedural bilirubin, mean diameter of the bile duct, etiology of biliary obstruction, and reasons for EUS failure are shown in Table 2.
Risk of bias evaluation
The GRADE checklist was used to evaluate the risk of bias in the included studies[22]. Table 3 shows a summary of the methodological qualities of studies reporting the prevalence data. Questions were answered as “yes”, “no”, “unclear”, or “not applicable”.
RESULTS
Our literature search yielded 315 manuscripts, of which 132 studies remained after excluding duplicate studies. After reviewing the title and abstract, only nine articles were left for the thorough screening of data by reviewing the full text. Further, two studies were eliminated after reading the manuscripts because they included primary EUS-BD cases wherein EUS was not attempted as the primary procedure. The third study was excluded, as it did not contain full text. A total of six studies met the abovementioned inclusion criteria of the study[23-28] (Figure 1).

Table 1 Baseline characteristics of the studies
DISCUSSION
The most common method for gaining access to the biliary tree is ERCP. In patients with unmodified upper gastrointestinal anatomy, the success rate of bile duct cannulation using ERCP is > 90%[25].Affected or variant anatomy, ampullary pathology (stones, stenosis, and tumor infiltration), periampullary diverticulum, gastric outlet obstruction, indwelling duodenal stent, and previous gastric bypass surgery are the prevalent causes of failed cannulation[29]. The rate of adverse outcomes associated with PTBD and surgery is extremely high, although these approaches are traditionally used to treat these clinical conditions[30]. The most prevalent issues related to long-term PTBD therapy are drain blockage,dislocation, and cholangitis, which require multiple interventions and longer hospital stays[31].Moreover, patients are left with a permanent external drain, resulting in poor quality of life[32]. EUS-BD has emerged as a viable, extremely safe, effective, and minimally invasive approach[33]. Using echoendoscopy and fluoroscopy, the biliary tree is accessed from the gastrointestinal lumen, a fistulous tract is created, and a stent is deployed in a single step, eliminating the need for an external drain[34].However, the rates of success and adverse events associated with EUS-BD remain unclear. The use of EUS-BD was first reported by Giovanniniet al[10] in 2001. Subsequently, several studies reported theefficacy of EUS-BD as an alternative BD method after a failed ERCP. The EUS-BD procedures are divided into three techniques: (1) EUS-RV; (2) EUS-guided antegrade (EUS-AG); and (3) EUS-guided transluminal BD, including EUS-guided choledochoduodenostomy (EUS-CDS) and EUS-guided hepaticogastrostomy (EUS-HGS)[6]. In EUS-RV, the biliary duct is accessed using fluoroscopy and EUS,forming a temporary fistula, followed by guidewire placement into the duodenumviathe biliary duct and ampulla. After guidewire placement, ERCP is performed using the EUS-placed guidewire, which is removed once biliary cannulation is obtained. Thus, EUS-RV should be performed in patients with an endoscopically accessible ampulla after unsuccessful biliary cannulation using conventional ERCP.
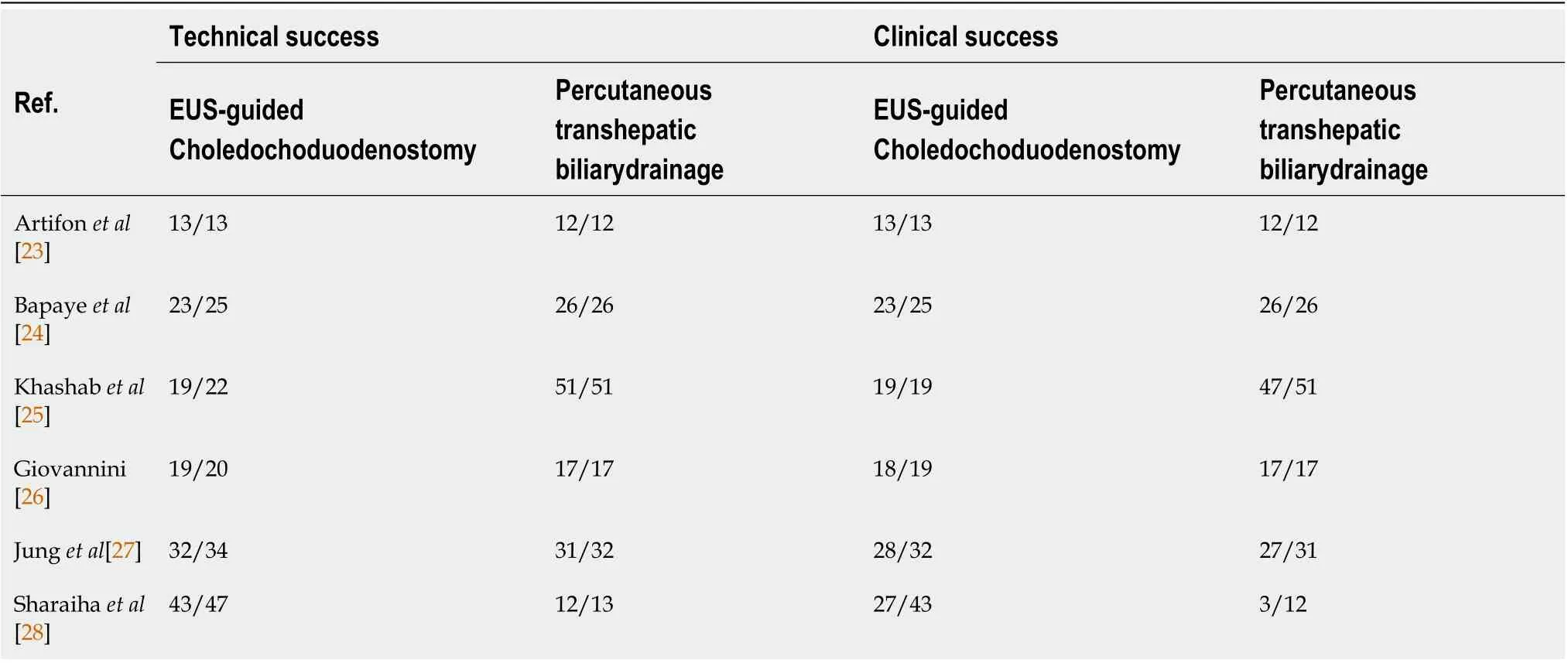
Table 2 Rates of clinical and technical success in the included studies

Table 3 Quality of identified studies
In EUS-AG, the intrahepatic biliary duct is accessed by creating a temporary fistula between the intestine and intrahepatic biliary duct from the upper intestine. Stent placement or balloon dilation is performed after the dilation of the fistula to achieve biliary obstruction through the fistula without reaching the ampulla using the endoscope. This technique is appropriate when reaching the biliary orifice using endoscopy is impossible or unmanageable, such as in biliary obstruction in patients with surgically altered anatomy or upper intestinal obstruction.
In EUS-guided transluminal BD, including EUS-CDS and EUS-HGS, the biliary duct is accessed followed by guidewire placement and fistula dilation under EUS guidance. For BD, a permanent fistula is created by inserting the stent between the biliary duct and the intestine. This procedure can be performed in cases where reaching the biliary orifice using endoscopy is possible or accessible;however, in patients with unresectable malignant biliary obstruction, its indication should be limited given the features of permanent fistula creation.
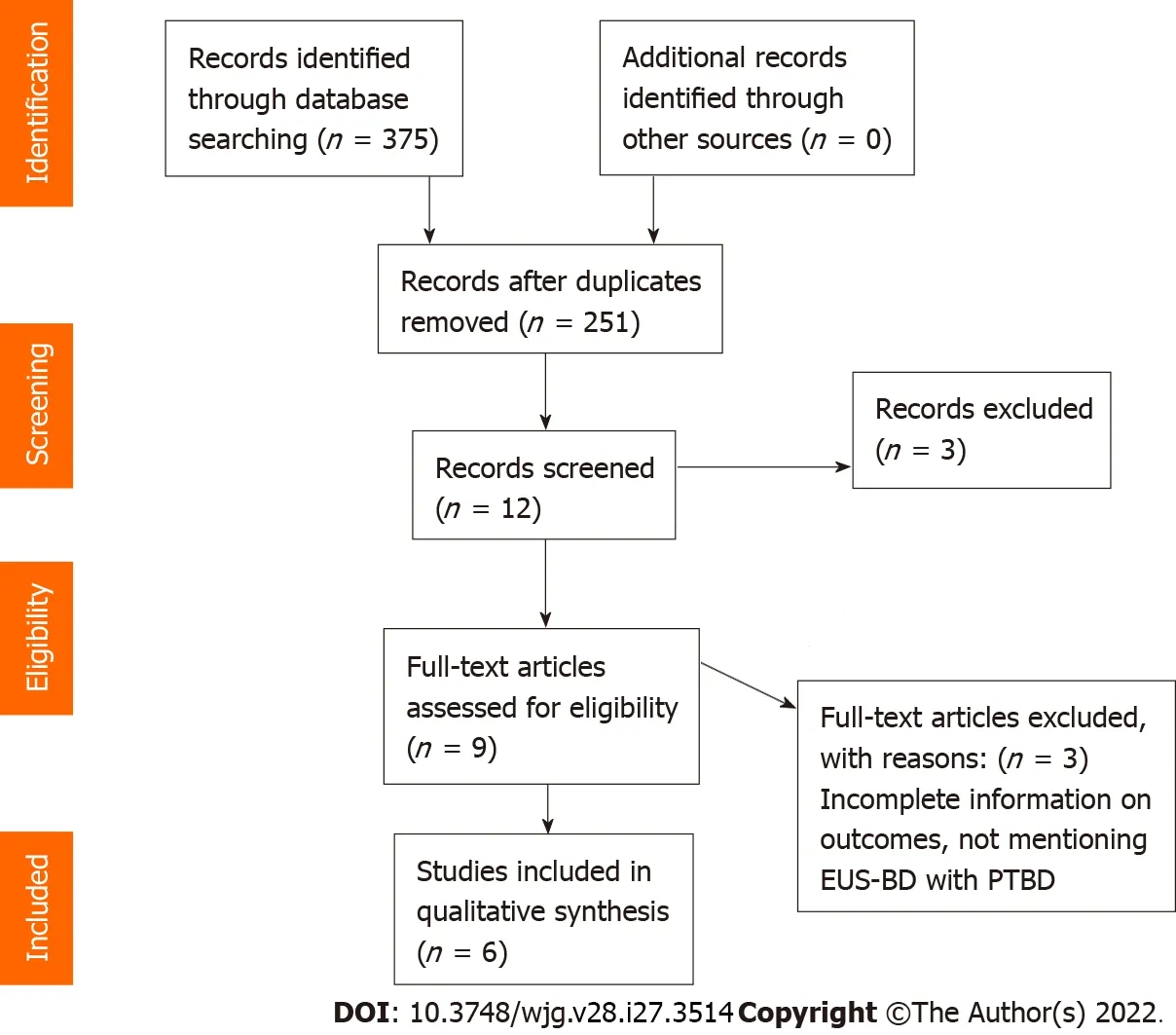
Figure 1 PRISMA Flow Diagram. EUS-BD: Endoscopic ultrasound-guided biliary drainage; PTBD: Percutaneous transhepatic biliary drainage.
Recent studies have demonstrated that EUS-BD could be an alternative to PTBD in patients with inoperable malignant biliary blockage and failed ERCP. However, individual study outcomes show inconsistent results. We performed a systemic analysis to aggregate information from individual trials and examine the overall outcomes of EUS-BD compared with PTBD. EUS-BD was associated with a lower rate of adverse events compared with PTBD. The healthcare cost of PTBD was twice that of EUSBD due to the high reintervention rate in the PTBD group. A retrospective study by Sharaihaet al[28]reported that the technical success rate was comparable between PTBD and EUS-BD in patients with inoperable malignant biliary obstruction and inaccessible papilla. In a retrospective study examining patients with incurable malignant biliary obstruction with failed ERCP due to an inaccessible papilla,Bapayeet al[24] found that the EUS-BD group had a higher success rate of BD (92%vs46%, respectively,P> 0.05) and a lower rate of adverse events than the PTBD group (20%vs46%, respectively,P= 0.05)[24]. These results were partially due to the use of EUS-BD in high-volume centers by experienced endoscopists. The rates of success and the complications of EUS-BD are expected to improve with technical advances.
In the present systematic review, the only randomized controlled study comparing EUS-BD and PTBD in patients with inoperable malignant biliary blockage was conducted by Artifonet al[8]. The study, which included 13 patients in the EUS-BD group and 12 patients in the PTBD group, reported that EUS-BD and PTBD were comparable in terms of cost, adverse events, and clinically meaningful improvements in bilirubin levels. The bilirubin levels in the EUS-BD group declined from 16.4 μmol/L to 3.3 μmol/L, whereas the bilirubin levels in the PTBD group declined from 17.2 μmol/L to 3.3 μmol/L[8]. The postprocedural follow-up period was 7 d in both the groups. Choiet al[32] reported a higher technical success rate in the PTBD group than in the EUS-BD group, although the functional success rate was comparable between the two groups[35].
In most facilities, PTBD is used as an alternative technique in cases of failed ERCP. In high-volume clinics, endoscopic ultrasound-guided gallbladder drainage has begun replacing PTBD, which was developed only a decade ago as the fourth approach for biliary decompression after surgical drainage,percutaneous transhepatic drainage, and endoscopic transpapillary drainage[36]. Although the type of BD approach used in cases of failed ERCP is currently determined by local competence, EUS-BD is a less intrusive and more physiologic technique. This approach improves nutrition absorption, prevents electrolyte loss, reduces reinterventions, and eliminates the stress of external drainage[37]. EUS-BD can also be performed in a single setting before ERCP if the patient agrees.
However, EUS-BD is associated with several specific issues. Only a small number of centers have the operational skills to perform EUS-BD, whereas most centers have extensive experience and skills to perform PTBD, and interventional radiologists are well-trained and equipped to perform PTBD[25]. The inherent risk of advanced endoscopy necessitates specialized training. Therefore, EUS-BD can only be performed in high-volume treatment institutions with adequate interventional radiology and surgical backup to prevent complications such as bile leak, pneumoperitoneum, hemorrhage, and stent migration[38,39].
The invasion of the sterile biliary tree by transmural puncture from the luminal side of the gastrointestinal tract poses a modest theoretical risk of infection in EUS-BD[40]. However, such negative events should improve with the further evolution of this technique. Despite its classification as a rescue treatment for failed ERCP, primary EUS-BD is currently compared with ERCP, and a recent study indicated similar short-term outcomes between EUS-BD and ERCP[41]. In addition, unlike ERCP, there is no risk of pancreatitis following EUS-BD. Furthermore, the clinical success rates and complications do not differ between EUS-BD and ERCP if performed by skilled endoscopists. The current systematic review revealed that EUS-BD was safe and effective when performed by skilled individuals, with a lower risk of adverse events and similar technical and clinical success rates.
Our analyses also indicated that: In patients with inoperable biliary blockage after a failed ERCP,EUS-BD was associated with a higher chance of successful BD and a lower risk of procedure-related adverse effects and infectious complications compared with PTBD. Furthermore, the number of patients with bile leaks was lower in the EUS-BD group than in the PTBD group.
CONCLUSION
Several case reports, series, and retrospective investigations regarding EUS-BD have been published to date. However, no prospective studies or comparisons of the various BD systems have been published;therefore, the technical success, functional success, adverse events, and stent patency of EUS-BD with long-term follow-up remain unknown. Prospective, randomized controlled studies are required to clarify these issues. However, it is clear that EUS-BD is clinically useful as a BD option. EUS-BD could become a first-line BD treatment instead of ERCP if the outcomes of clinical studies are positive and technologies are simplified.
ARTICLE HIGHLIGHTS
Research background
Percutaneous transhepatic cholangiography is a diagnostic and therapeutic procedure. Endoscopic ultrasound-guided biliary drainage (EUS-BD) is a novel technique that allows BD whose technicality,success rate, and outcomes are not negligible.
Research motivation
We aimed to compare the technical details and outcomes of 132 studies concerning interventional BD procedures in patients with obstructive cholangiopathy. We conducted a systematic review of six studies that met the inclusion criteria.
Research objectives
To assess the suitability and appropriability of different clinical biliary interventions in achieving optimal BD for obstructive cholangiopathy.
Research methods
An extensive systematic review was independently conducted by two investigators using an electronic search of different databases, including PubMed, Embase, clinicaltrials.gov, the Cochrane library,Scopus, and Google Scholar, using the guidelines for Preferred Reporting Items for Systematic reviews and Meta-Analyses to identify studies comparing percutaneous transhepatic BD (PTBD) and EUS-BD.
Research results
PTBD patients underwent significantly more reinterventions (4.9vs1.3), experienced more postprocedural pain (4.1vs1.9), and experienced more late adverse events (53.8%vs6.6%) than EUS-BD patients. There was a significant reduction in the total bilirubin levels in both the groups (16.4-3.3 μmol/L and 17.2-3.8 μmol/L in the EUS-BD and PTBD groups, respectively;P= 0.002) at the postprocedural 7-d follow-up. There were no significant differences in the complication rates between the PTBD and EUS-BD groups (3.3vs3.8). PTBD was associated with a higher adverse event rate than EUS-BD in all the procedures, including reinterventions (80.4%vs15.7%, respectively) and a higher rate of index procedure (39.2%vs18.2%, respectively).
Research conclusions
EUS-BD might be considered as a first-line BD treatment instead of PTBD if the outcomes of clinical studies are favorable and the technical approach is simplified.
Research perspectives
EUS-BD following failed ERCP was superior to PTBD in patients with obstructive cholangiopathy.
FOOTNOTES
Author contributions:Hassan Z contributed in study selection, data analysis, and writing of the manuscript; Gadour E contributed in study conception, analysis and interpretation of the data, and drafting of the manuscript; and all authors have approved the final manuscript.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
PRISMA 2009 Checklist statement:The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:United Kingdom
ORCID number:Zeinab Hassan 0000-0003-0703-6500; Eyad Gadour 0000-0001-5087-1611.
Corresponding Author's Membership in Professional Societies:British Society of Gastroenterology, BSG64346.
S-Editor:Wang JJ
L-Editor:A
P-Editor:Wang JJ
杂志排行
World Journal of Gastroenterology的其它文章
- Crosstalk between dietary patterns, obesity and nonalcoholic fatty liver disease
- Regulatory T cells and their associated factors in hepatocellular carcinoma development and therapy
- Associations of gut microbiota with dyslipidemia based on sex differences in subjects from Northwestern China
- Prognostic significance of hemoglobin, albumin, lymphocyte,platelet in gastrointestinal stromal tumors: A propensity matched retrospective cohort study
- Contrast-enhanced ultrasound Liver Imaging Reporting and Data System: Lights and shadows in hepatocellular carcinoma and cholangiocellular carcinoma diagnosis
- Isolated gastric variceal bleeding related to non-cirrhotic portal hypertension following oxaliplatin-based chemotherapy: A case report
