Impact of COVID-19 pandemic on clinicopathological features of transplant recipients with hepatocellular carcinoma: A case-control study
2022-06-22SamiAkbulutTevfikTolgaSahinVolkanInceSezaiYilmaz
INTRODUCTION
On December 11, 2019, an atypical pneumonia leading to acute respiratory distress syndrome in individuals was reported for the first time in Wuhan city of Hubei Province of China. The etiology was identified to be a new form of coronavirus. Later taxonomic studies defined it to be a new member of the beta-coronavirus family, and was renamed as severe acute respiratory syndrome coronavirus-2. The disease was named as the coronavirus disease 2019 (COVID-19)[1,2]. In Turkey, the first confirmed case of COVID-19 was declared on March 11, 2020. On January 30, 2020, the World Health Organization declared COVID-19 as a public health emergency of international concern, which was a declaration that the situation had become a pandemic and necessary precautions should be taken immediately[3].COVID-19 soon spread all around the world, and currently there are 255324963 confirmed cases of COVID-19, and 5127696 cumulative deaths are related with COVID-19 and its complications[4]. Since then, there have been 8503220 confirmed cases of COVID-19 in Turkey, and in total 74428 patients died due to COVID-19 and related complications[4].
COVID-19 has overwhelmed the health-care services all around the world. The organization of healthcare facilities was changed, and treatment of many diseases such as heart disease, liver disease and various cancers have been postponed until the pandemic was under control. Also, the COVID-19 pandemic had a significant impact on the emergency procedures. The organization, surveillance strategy and prioritization of the patients should all be reorganized during these periods[5]. Vulnerable populations such as patients with cancer should be determined. As necessary precautions are taken, all nosocomial infections including COVID-19 can be prevented and all emergency procedures can be performed safely[5]. Another point that should be considered is the overwhelming stress and burnout of the health care professionals. As the health care personnel become psychologically burned out, the management of vital diseases such as cancers are disrupted[5,6].
In Turkey, soon after the first confirmed case of COVID-19, the state hospitals were reorganized as the pandemic hospital, and elective surgeries, treatments and daily based procedures such as endoscopies were all cancelled to prevent transmission of COVID-19 between individuals[7]. Liver diseases and transplantation received the hardest blow due to the spread of COVID-19 cases. The use of hospital resources for patients with COVID-19, fear of hospital visits due to risk of disease transmission and economic consequences of the devastating pandemic have crippled the liver transplantation (LT)efforts[8]. In the beginning of the pandemic before the development of vaccination strategies, various societies in the field recommended reduction in the frequency of hospital visits and transplantation procedures in patients with stable disease[9-11]. This strategy has reduced deceased donor liver procurement and transplantation by nearly 80%[12-16]. Soin[8] reported that living donor LT(LDLT) has dropped by 60% since the beginning of the pandemic in India. Similarly, Bhatti[17]stated that the LDLTs were on average 70% lower than the pre-COVID-19 period. However, they found that waiting list mortality did not change during the pandemic and pre-pandemic periods, and early mortality rate was found to be even lower than the pre-pandemic period[17].
Toward the end of that year, the kids on my bus gave me a small trophy7(,) inscribed8 “To the Best Bus Driver Ever”. I propped9 it up on the dashboard() . On top I hung a small tin heart that a little girl had given me. In red paint she had written, “I love Polly and Polly loves me.”
Hepatocellular carcinoma (HCC) is a very important disease that needs close follow-up for recurrence after treatment or progression following downstaging procedures[18]. However, the risk should be balanced in terms of risk of contracting the disease in a high-risk environment for COVID-19 transmissionthe risk of progression or recurrence of HCC in the patients. The patients with HCC have an increased risk of contracting a severe form of COVID-19 for two reasons: (1) They are immunosuppressed because of the cancer treatment; and (2) They are typically of older age and have associated comorbidities that increase the risk of developing severe COVID-19[19,20].
There are many observational studies that have been published in the era of COVID-19 that show that in general cancer patients have a higher mortality risk during COVID-19 infection[21-24]. Specifically,Deng[21] created a population-based study and showed that the mortality risk increased by 3-fold in cancer patients when they were infected with severe acute respiratory syndrome coronavirus-2. These results have also been confirmed by the study performed by Mehta[22] stating that the mortality rate of COVID-19 infection among cancer patients were twice the mortality rate in patients without COVID-19.
There are various limitations in our study. The major one is the retrospective design of the study. We considered patients who were transplanted for HCC. However, other bridging therapies as well as systemic therapies were not considered. Since our study was not designed as an intention to treat analysis, we cannot draw definitive conclusions regarding the impact of COVID-19 on treatment of patients with HCC. Furthermore, the follow-up period of the patients transplanted during the pandemic is very short. As our survival data accumulates, we can provide better data regarding the significance of increased lymphovascular invasion on the prognosis of the patients. Lastly, the number of patients is low, and results such as increased rate of lymphovascular invasion during the pandemic should be evaluated with a level of skepticism.
Gandhi[29] analyzed 27 centers in the Asian-Pacific region where the incidence of HCC was highest. Fourteen of the centers replied to the online questionnaire. Their results showed that there was a nearly 27% drop in the diagnosis of the participating centers; also, there was 50% delay in the diagnosis of HCC. Furthermore, there was a change towards administering oral molecularly targeted systemic therapy in patients with HCC[29]. Similarly, a multicenter study conducted by Muñoz-Martí nez[30] showed dramatic results showing a 40% change in diagnostic procedures, an 87% change in surveillance protocols and a 42% change in the liver transplant program. According to these results,currently more advanced HCC with high drop-out risk were to receive curative treatment such as LT or resection. In our opinion, this would be reflected on the clinicopathologic characteristics of the patients evaluated in transplant centers. However, despite changes in the management and follow-up protocols of patients with HCC, the definitive impact of these changes in patients who received definitive treatment during the pandemic is not clear.
We have also changed our priorities and made changes in the management of patients with end-stage liver disease including HCC. We have previously published our preventive measures and guidelines for handling the infected patients and/or health-care personnel in our institute, which has the highest volume of LDLT in Europe[31]. Therefore, in the present study, our aim was to compare the demographic, clinical and histopathologic characteristics of the patients with HCC during the COVID-19 pandemic with the patients in the pre-pandemic period. We aimed to define any change in the tumor behavior or any change in the management of these patients during the COVID-19 pandemic.
MATERIALS AND METHODS
The World Health Organization declared COVID-19 as a public health emergency of international concern on January 30, 2020. The first confirmed case of COVID-19 was declared by the Ministry of Health of Turkey on March 11, 2020. The patients that have been transplanted for HCC in our institute between March 11, 2020 and June 21, 2021 were included in the study. The data of the patients were prospectively collected and retrospectively analyzed. These patients that received operations during the pandemic period were included in the pandemic group. Our aim was to evaluate the impact of COVID-19 on demographic and clinicopathologic characteristics of the patients with HCC; for this reason we included 61 patients who were transplanted for HCC in our institute between November 12, 2018 and March 10, 2020 (before the pandemic) in our study. They were included in the pre-pandemic group.Therefore, we obtained the opportunity to compare the patients with HCC transplanted during the 15 mo peroid after the confirmation of the pandemic in Turkey to the patients with HCC who were transplanted during the 16 mo period before the pandemic. First, the required official administrative permission from the Directorate of the Liver Transplant Institute was granted (Approval date:04.10.2021 and Number: 93889). Then, ethical approval was obtained from the Inonu University Institutional Review Board (IRB) for non-interventional studies (Approval date: 05.10.2021 and Number: 2538).
The study parameters included age (years), sex (female, male), body mass index, graft weight (gram),MELD score, alpha fetoprotein (AFP), tumor number, total diameter of the tumors (TTD; cm), liver index score, Agg index, white blood cell, hemoglobin, platelets, neutrophil, lymphocyte, neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, International normalized ratio, creatinine, albumin, total bilirubin, direct bilirubin, alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase(ALP), gamma-glutamyl transpeptidase (GGT), lactate dehydrogenase, C-reactive protein, type of LT[LDLT, deceased donor LT (DDLT)], Child score (A, B, C), Milan criteria (single tumor ≤ 5 cm or ≤ 3 tumor with the largest ≤ 3 cm), UCSF criteria (single tumor ≤ 6.5 cm or ≤ 3 tumors with the largest tumor≤ 4.5 cm and total tumor diameter ≤ 8 cm), BCLC criteria (single tumor ≤ 7 cm, three tumor ≤ 5 cm, five tumor ≤ 3 cm, maintained response within Milan criteria during 6 mo after downstaging), Tokyo 5-5 rule (5 tumor with a maximum tumor size ≤ 5 cm), Onaca criteria (single tumor ≤ 6 cm or 2-4 tumors with the largest tumor ≤ 5 cm), CUN Navara criteria (single tumor ≤ 6 cm or ≤ 3 tumors with the largest≤ 5 cm), Up-to-7 criteria (total tm diameter ≤ 7 cm and total number of tm ≤ 7), AFP model criteria{[largest tumor size: ≤ 3 cm (0 point), 3–6 cm (1 point), > 6 cm (4 point)] [total number of tumor: 1–3 tumor (0 point), ≥ 4 tumor (2 point) [AFP level: ≤ 100 (0 point), 100–1000 (2 point), > 1000 (3 point)]},AFP-TTD criteria (AFP ≤ 400 ng/mL and total tumor diameter ≤ 8 cm), expanded Malatya criteria(maximum tumor diameter ≤ 10 cm and AFP ≤ 200 ng/mL and GGT ≤ 104 U/L and within Milan criteria), 5-5-500 rule (nodule size ≤ 5 cm in diameter, nodule number ≤ 5, and AFP ≤ 500 ng/mL),Samsung criteria (≤ 7 tumors, diameter ≤ 6 cm, AFP ≤ 1000 ng/mL), macrovascular invasion (present,absent), tumor differentiation (well, moderate, poor), lymphovascular invasion (present, absent),perineural invasion (present, absent), capsular invasion (present, absent), tumor necrosis (present,absent), locoregional therapy (transarterial radioembolization, transarterial chemoembolization,radiofrequency ablation, microwave ablation, resection,), ascites (no, moderate, massive), outcome(alive, dead) and recurrence (yes, no).
But when she looked up once in her grief there stood a woman beside her who asked, Little Two-eyes, what are you crying for? Little Two-eyes answered, Have I not reason to cry? Because I have two eyes like other people, my sisters and my mother cannot bear me; they push me out of one corner into another, and give me nothing to eat except what they leave
Evaluation of patients with HCC who were candidates for LT before the COVID-19 pandemic
Various diseases such as cancer need special attention due to their progressive nature, which is especially valid if appropriate treatment is not applied and it may even lead to mortality[37]. On the other hand, the patients with a high risk for mortality due to a severe course of COVID-19 are patients with chronic diseases such as chronic obstructive pulmonary disease, cardiac disease and patients with cancer. In the initial stages of the pandemic, changes were made in the management protocol of every disease including cancer[37,38]. The European Society for Medical Oncology consensus statement stated that treatment of any cancer patients should not be postponed or cancelled without proper risk stratification[39]. HCC is an aggressive tumor with variable tumor biology that has a high tendency to relapse. The recurrence rates following LT and resection are 30% and 70%, respectively[40]. In the initial stages of the pandemic, Gori[41] published their altered protocol for management of patients with end-stage liver disease including HCC. They prioritized LT for HCC patients with a high risk of progression and drop out. Microwave and radiofrequency ablation were explicitly performed in patients for whom resection was planned; furthermore, locoregional transarterial procedures have been performed as planned but postponed in patients older than 80 years[41]. Iavarone[38] published the results of this altered protocol in a brief communication. They showed that there was a delay of months or longer in the treatment of 26% of the patients[38]. This delay may have serious consequences for a disease such as HCC.
Evaluation of patients with HCC that were candidates for LT during the COVID-19 pandemic
After the confirmation of the first case with COVID-19 in Turkey, the Ministry of Heath released new regulations limiting all elective procedures including elective LTs and advised the liver transplant centers to perform a risk stratification. In addition, emergency LTs, such as those performed for acute liver failure, recipients with a MELD score > 19, patients who were to be transplanted for cancer and patients who were decompensated (intractable ascites, jaundice, encephalopathy and variceal bleeding),during the follow-up period could be performed provided that necessary precautions were taken at the operating room and the patient ward[31]. We have previously published our COVID-19 surveillance strategy in LDLT[31]. In the initial stages of the pandemic, patients with HCC within Milan criteria and with tumors greater than 2 cm were transplanted.
However, various vaccines have been developed, and normalization efforts have started in countries who have vaccinated more than 70% of its population. The organization of the health care centers started to revert to the pre-pandemic state, and elective surgical procedures resumed provided that necessary precautions were taken, as well as COVID-19 surveillance is performed. Therefore, LT for HCC has also returned to its pre-pandemic state. Nevertheless, we are still performing a strict COVID-19 surveillance for our patients and donors (deceased or alive) who will undergo LT.
Our follow-up protocol after LT
Our immunosuppressive treatment protocol following LT for HCC is as follows: Corticosteroids are initiated starting from the completion of hepatic artery anastomosis and continues to the postoperative period. The dose is tapered gradually and discontinued on the postoperative third to sixth month.Tacrolimus is initiated on the postoperative third day, and the dose is tapered to obtain trough levels of 6-10 ng/mL. Similarly, mycophenolate mofetil is started on the postoperative third day and is discontinued after the first month in patients who are transplanted for HCC. In the postoperative first month,everolimus is started to achieve trough levels of 8-10 ng/mL, and the tacrolimus dose is tapered to achieve trough levels between 5-7 ng/mL. After the third month following LT, tacrolimus-everolimus combination is continued.
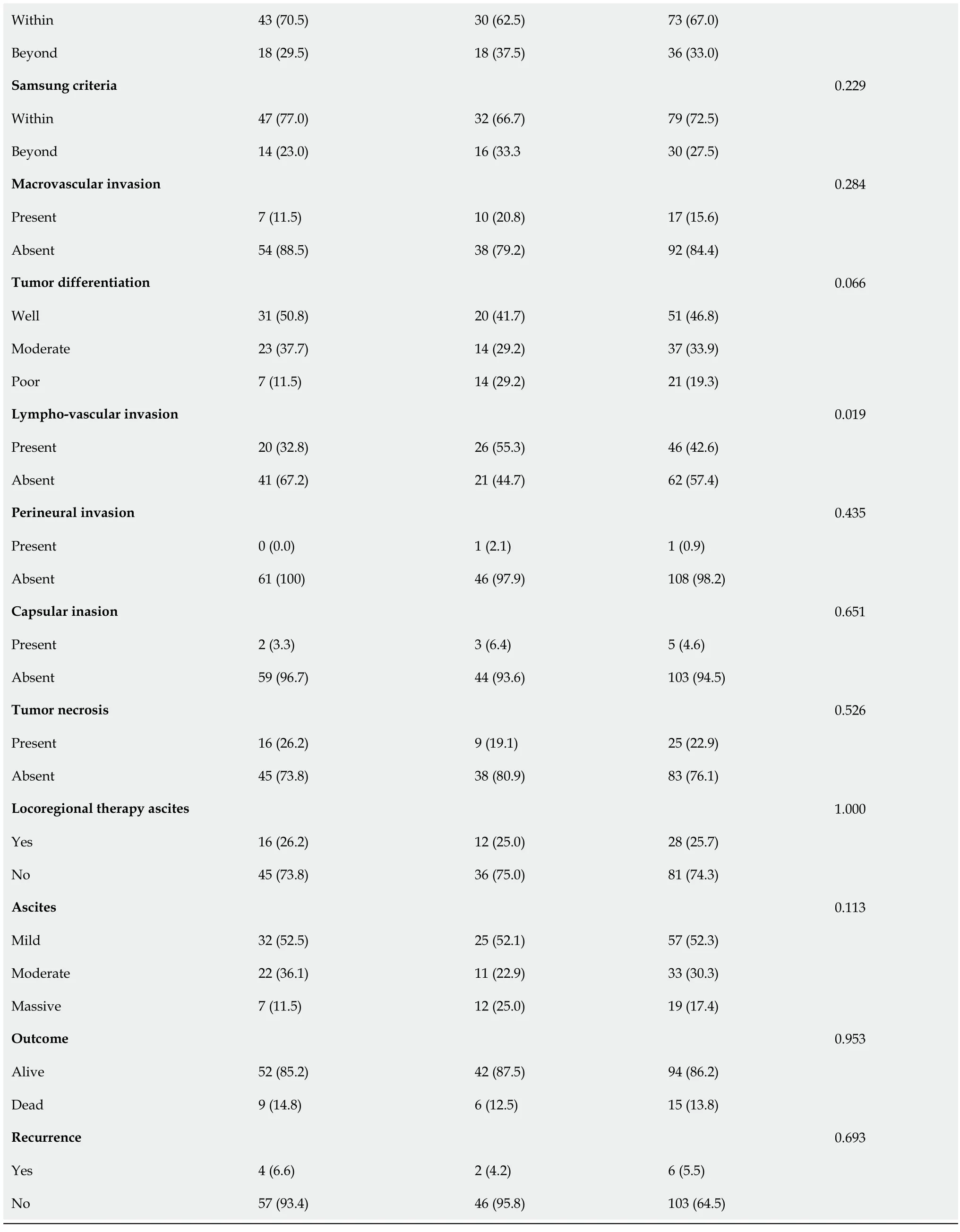
In the initial stages of the pandemic, we transplanted patients with HCC with tumors greater than 2 cm. However, we developed a strict surveillance program and started to transplant patients according to our conventional protocol. Our results show that using our surveillance protocol there was no difference between the pandemic and pre-pandemic period in terms of the stages of tumors at the time of LT. For this reason, our protocol seems feasible in the management of patients with HCC. However,we found that the rate of lymphovascular invasion was higher in patients transplanted during the COVID-19 period. We believe this may be related to the observational difference between the two time periods because the staging of the tumors (performed by different classification methods) was similar between the two groups, and we have summarized these results in Table 1. Microscopic vascular invasion is an especially major determinant of early recurrence following treatment as well as a major risk factor for metastatic disease[42]. The patients receiving an operation during the pandemic do not have sufficient follow-up period to determine any recurrences. However, similar stages of the disease between the two-time intervals suggests that we may not observe a major difference in the recurrence or the outcome of the patients.
Coronavirus disease 2019 (COVID-19) has overwhelmed the healthcare services all around the world.The organization of healthcare facilities were changed and treatment of many diseases such as heart disease, liver disease and various cancers have been postponed until the pandemic was under control.Hepatocellular carcinoma (HCC) is an aggressive disease that shows progression without any intervention. Therefore, the impact of COVID-19 in the management of progressive diseases such as HCC needs to be investigated.
There he left them, and there they were found by the man and woman who had met him at home beside the sea, and had helped him to start on his journeyWhen this had been done the boy and his bride set forth for home, and landed at the harbour of his native land
Statistical analysis
The statistical analyses were performed using IBM SPSS Statistics v25.0 (Statistical Package for the Social Sciences, Inc, Chicago, IL, United States). The quantitative variables were expressed as median and interquartile range. The qualitative variables were reported as number and percent (%). Kolmogorov–Smirnov were used to assess normality of quantitative variable distribution. Nonparametric Mann Whitneytest was used to compare quantitative variables. Pearson’s χtest was used to compare qualitative variables.≤ 0.05 was considered a statistically significant value.
RESULTS
General characteristics of the patients
In total, 109 patients were included for analysis in the study, and the median age of the patients in the study was 56 (interquartile range = 15). Ninety-seven patients (89%) were male and 12 were female(11%). The common etiologies of liver disease were hepatitis B virus (= 52), cryptogenic (= 26),hepatitis C virus (= 8), hepatitis B virus + hepatitis D virus (= 8) and miscellaneous (= 15). Eightone patients (74.3%) underwent LT as the primary therapeutic modality, and 28 patients (25.7%)received LT after various modalities of locoregional therapy. One hundred and two patients received LDLT (93.6%), and 7 patients (6.4%) received DDLT. Fifty-nine patients had tumors within the Milan criteria (54.1%), 69 patients (63.3%) were within the UCSF criteria 78 patients (71.6%) were within BCLC criteria, 76 patients were within the 5-5 rule (69.7%), 75 patients (68.8%) were within the Onaca criteria,69 patients (63.3%) were within the CUN Navara criteria, 75 patients (68.8%) were within the up-toseven criteria, 74 patients (67.9%) were within AFP model, 78 patients 71.6%) were within AFP-TTD criteria, 73 patients (67%) were within the 5-5-500, 79 patients (72.5%) were within the Samsung criteria,and 75 patients (68.8%) were within the expanded Malatya criteria. Seventeen patients (15.6%) had microvascular invasion, 21 patients (19.3%) had poor differentiation, 46 patients (42.6%) had lymphovascular invasion, 1 patient (0.9%) had perineural invasion, 5 patients (4.6%) showed capsular invasion, and 25 patients (22.9%) had tumor necrosis confirmed by pathologic analysis. The median follow-up period was 571 d (interquartile range = 457; min-max = 17-1051 d). Fifteen patients (13.8%)died during the median follow-up period, and six of the mortalities were within the postoperative first 90 d, which was regarded as early mortality.
Pre-pandemic vs pandemic era
Based on March 11, 2020 as the turning point towards the global catastrophe, 61 patients in the prepandemic period and 48 patients in the pandemic period underwent LT for HCC. According to our results, there was a 21.3% drop in the number of patients transplanted for HCC. We found no statistical significant difference between groups in terms of age (= 0.685), sex (= 0.629), body mass index (=0.352), graft weight (= 0.925), MELD score (= 0.413), Child score (= 0.353), pre-LT AFP level (=0.643), tumor number (= 0256), TTD (= 0.712), liver index score (0.417), Agg index (= 0.183), white blood cell (= 0.298), hemoglobin (= 0.079), platelets (= 0.363), neutrophil (= 0.394), lymphocyte (= 0.498), neutrophil to lymphocyte ratio (= 0.819), platelet to lymphocyte ratio (= 0.634), International normalized ratio (= 0.112), creatinine (= 0.955), albumin (= 0.888), total bilirubin (= 0.138),direct bilirubin (= 0.306), aspartate aminotransferase (= 0.157), alanine aminotransferase (= 0.944),GGT (= 0.213), lactate dehydrogenase (= 0.325), C-reactive protein (= 0.533), Milan criteria (=0.337), UCSF criteria (= 0.450), BCLC (= 0.429), Tokyo (= 0.684), Onaca (= 0.293), CUN Navara (= 0.450), Up-to-7 (= 0.142), AFP model (= 0.202), AFP-TTD (= 0.223), 5-5-500 rule (= 0.449),Samsung (= 0.229), Malatya (= 0.723) and Extended Malatya (= 0.826).
However, statistically significant differences were found between pre-pandemic and pandemic groups in terms of serum ALP levels (= 0.029), lymphovascular invasion (= 0.019) and type of the liver graft that was transplanted (= 0.017). In patients who were transplanted for HCC in the COVID-19 period, the use of grafts from the living donors was 13.3 times more frequent than the COVID-19 period [odds ratio = 13.3; 95% confidence interval (CI) = 0.74-240]. The rate of lympho-vascular invasion in the explant pathologies of patients was found to be 2.54 times more frequent in patients who received operations during the COVID-19 period (odds ratio = 2.54; 95%CI = 1.15-5.56). Categorical and continuous variables of the groups and results of the statistical analyses are summarized in Tables 1 and 2.
"Back in those days, we had a very different approach, where first you designed your features, and a lot of thought and design process went into that," said Saenko, an associate professor at the Department of Computer Science at Boston University.
DISCUSSION
HCC is the most common primary liver tumor and the fourth to fifth leading cause of cancer-related deaths[33]. HCC usually develops in patients with chronic liver disease and viral hepatitis such as hepatitis B virus and hepatitis C virus play an important etiologic role in its development. The incidenceis also rising in developed countries[34]. It meets the criteria of a particular disease that necessitates screening: (1) It is common in individuals of certain subpopulations; (2) Populations at highest risk of developing HCC is defined in detail; (3) Screening tests are non-invasive or minimally invasive; (4)Population at risk usually has underlying chronic liver disease and is subject to regular out-patient follow-up; and (5) Early diagnosis provides advantages in terms of survival and cure of the disease[34,35]. For these reasons, patients with HCC need special attention regarding the course of the disease[35,36]. Any deviation from the standard of care adapted for these patients may have devastating results. In the present study, we evaluated the pre-pandemic and COVID-19 era in terms of clinicopathologic characteristics in patients who were transplanted for HCC. This is one of the first studies evaluating the consequences of the pandemic era on critical diseases such as HCC using the clinicopathologic characteristics.
COVID-19 has overwhelmed the everyday healthcare services. Treatment of many cancers such as liver cancer have been postponed until the COVID-19 pandemic was under control. A delay in the treatment of HCC has serious consequences that would reflect the clinical and tumor characteristics of the patients.
In our institution prior to defining the expanded Malatya criteria[32], patients were considered eligible for LDLT only if the disease was confined to the liver and without any macrovascular invasion. Since 2016, the indication for LT was discussed in multidisciplinary liver tumor board that was constituted by transplant surgeons, medical oncologist, radiologist, nuclear medicine specialist, pathologist and hepatologist. The law commissioned by the Turkish Ministry of Health on organ procurement and allocation allow DDLT in patients with HCC that are within the Milan criteria. However, this does not apply to the recipients of the living liver donors. Therefore, patients with tumors beyond the Milan criteria can only receive LDLT. Our preoperative evaluation includes liver function tests, complete blood counts, coagulation parameters, AFP levels, multi-slice computed tomography scans and magnetic resonance imaging. Recently, we also added positron emission tomography/computerized tomography scan to our work-up scheme.
But I m not sure that he understands the part he played in that transition6. The words I heard growing up pierced7 my soul, yet his words pierced even deeper.

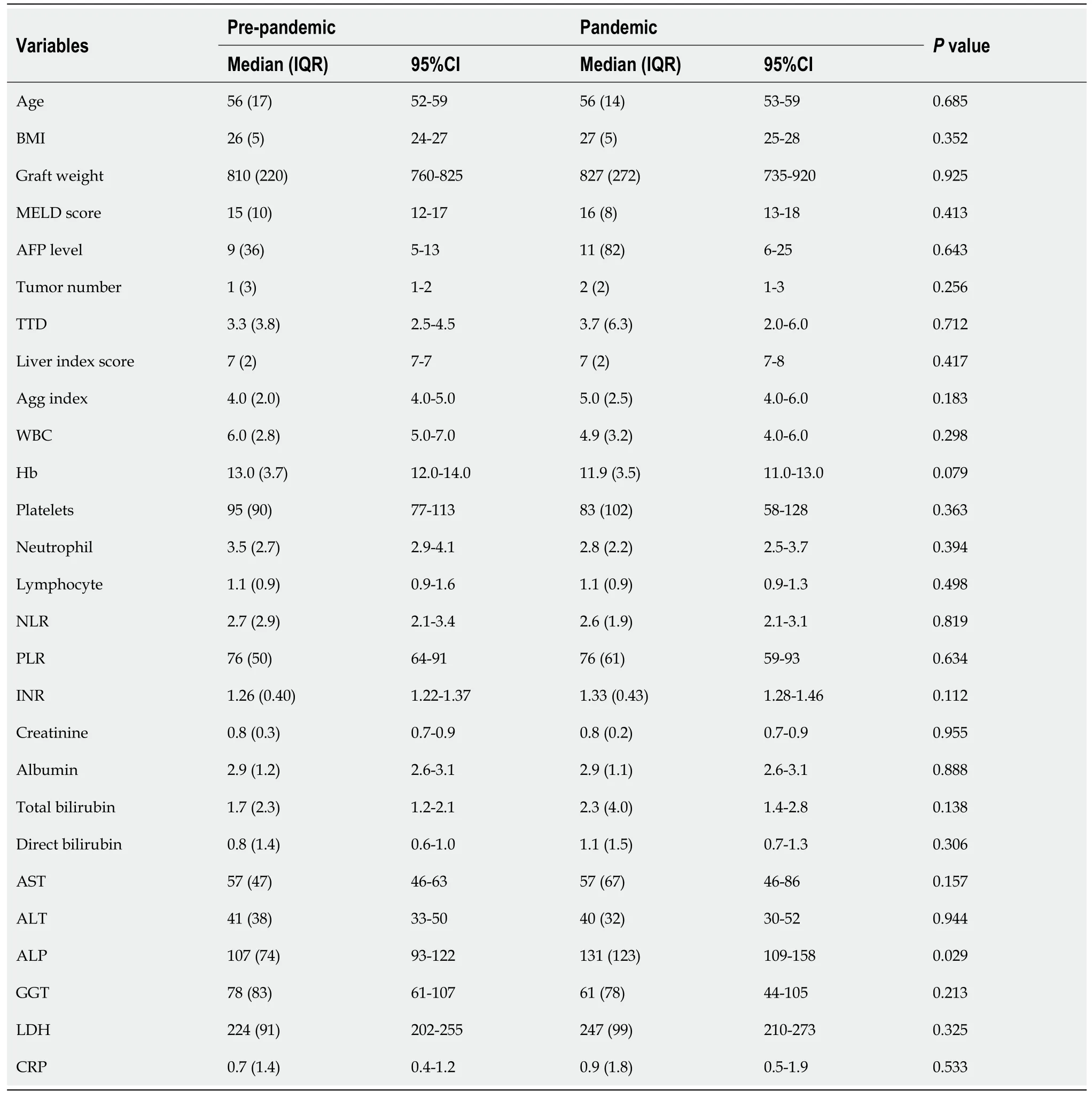
Wu[43] showed that ALP and GGT were prognostic indictors in patients with HCC undergoing liver resection. Their cohort included 469 pathologically confirmed HCC. They found that high ALP levels (≥ 136.5 IU/mL) were associated with larger tumors (> 5 cm), vascular invasion and advanced BCLC stages[43]. Also, they found that ALP was an independent prognostic factor determining overall survival but not disease-free survival[43]. Both Wu[43] and other researchers[43-46] have stated that GGT can be a marker for tumor stem cells, microvascular invasion, tumor proliferation and nuclear cell cycle control in the tumors. The results of our study showed that ALP levels were significantly higher in the patients transplanted during the pandemic period. However, there was no significant difference in the GGT levels between the two groups. Therefore, we believe that this is an observational difference and will not have an impact on the survival or recurrence of the patients. However, HCC is a very heterogenous disease in terms of antigenic content, which also reflects upon the biologic behavior. This mosaicism determines the aggressive nature of the tumors[47]. In the present study, only increased microvascular invasion that is a subjective parameter does not determine the absolute outcome of the tumors of the patients. We have also evaluated multiple parameters that show that stages of the tumor did not change when compared to the pre-pandemic period.
On the next evening Tsarevitch Vasilii went into the garden to watch, and he, too, fell asleep at midnight, and next morning when his father summoned him, he, like his brother, being ashamed to tell the truth, answered: Gracious Sir, I watched throughout the night but the Fire Bird that steals the golden apples did not enter thy garden.
During the pandemic, the transplant activities around the world decreased significantly[15,45-48].Furthermore, the patients with lower scores who were stable were postponed[49-53]. The deceased organ donation significantly decreased even in areas with low COVID-19 incidence[54,55]. Aubert[56] performed a multi-institutional study and showed that there was a dramatic decrease in both DDLT and LDLT activities[56]. Furthermore, in countries such as Japan where the number of COVID-19 cases as well as COVID-19-related deaths were low and due to strict preventive measures taken, there was a nearly 70% decrease in solid organ transplantation[56]. However, in countries such as the United States,the number of COVID-19 cases as well as the number of deaths were higher, but there was only a 4%decrease in solid organ transplantation[56]. In our institute, the DDLT rates decreased. However, we managed to preserve a relatively high rate of LDLT, which is very unique when considering the study performed by Aubert[56]. This is the reason we observed a change in the type of the liver graft used in the present study, which was a decrease in the deceased donor organ grafts and an increase in the LDLT in the COVID-19 pandemic. In Turkey, LDLT are generally the mainstay of the liver grafts. Since the relatives are determined to donate their organs for their relatives, the LDLT was sustained in a relatively stable course during the COVID-19 pandemic.
Furthermore, the care of the patients with HCC has also been interrupted by the overwhelming number of patients with COVID-19[18]. Therefore, patients cannot reach hepatology units for proper care, and diagnostic procedures such as imaging studies, endoscopies and biopsies are delayed. All these factors have detrimental effects on the diagnosis of new HCC tumors and surveillance of the patients that were already receiving medical care[25]. Increased mortality and morbidity in patients with HCC during the pandemic era are due to chronic liver disease. Although chronic liver disease does not specifically increase the susceptibility to COVID-19, specific liver diseases such as fatty liver disease(as a part of the metabolic syndrome) increases the risk of mortality due to severe COVID-19 infection[26,27]. Also, in patients with autoimmune liver disease, immunosuppressive medication used during the treatment of the disease may increase the risk of severe COVID-19 infection[28].
CONCLUSION
In conclusion, our results show that there was only a modest change in the tumor biology during the COVID-19 pandemic. This shows the efficacy of our surveillance program, which enables transplanting patients with HCC according to conventional management protocols. We believe that the increased lymphovascular invasion rate in the present study is an observational variation because there is no change in the stages of the diseases between the two intervals. The DDLT rate in Turkey is already low,and it further decreased during the pandemic. However, we managed to preserve a high rate of LDLT.Therefore, it is important to develop a surveillance strategy for liver transplant centers. The LT for HCC is justified and safe provided that strict surveillance protocols are applied.
ARTICLE HIGHLIGHTS
Research background
Our postoperative surveillance program is very intense. In the postoperative first 2 years, the AFP levels are analyzed every month. Multi-slice computed tomography is obtained every 3 mo for the first postoperative 2 years. After the second year following the LT, cross-sectional imaging techniques are performed annually. If there is a suspicion of recurrence on laboratory and multi-slice computed tomography, contrast enhanced magnetic resonance imaging and positron emission tomography/computed tomography are performed to confirm the diagnosis. In patients with hepatic recurrence, we perform multimodality treatment including resection, locoregional therapeutic options(transarterial therapies, radiofrequency or microwave ablations) and systemic chemotherapy including sorafenib.
Research motivation
When Roger died of lymphatic cancer in December 1985, I attended the funeral in Fargo, North Dakota. After the ceremony, I went to Pat and told her how sorry I felt. She hugged me, and then turned to her six children. I want to introduce someone really special. Kids, this is Andy Strasberg. And Roger Maris Jr. said, You re Dad s number-one fan.
Research objectives
The main objective was to compare the demographic, clinical and histopathologic characteristics of the patients with HCC who have undergone liver transplantation during the COVID-19 pandemic with the patients in the pre-pandemic period. We aimed to define any change in the tumor behavior or any change in the management of these patients during the COVID-19 pandemic.
Research methods
Demographic, clinicopathological variables of patients with HCC who have undergone liver transplantation between March 2020 and June 2021 (Pandemic group, n = 48) were retrospectively compared with that of the patients with HCC transplanted between November 2018 and March 2020(Pre-pandemic group, n = 61).
Research results
Ninety-seven patients (89%) were male, and 12 were female (11%). The most common etiology of liver disease was hepatitis B virus (n = 52, 47.7%). Statistically significant differences were found between groups in terms of blood alkaline phosphatase levels (P = 0.029), lymphovascular invasion (P = 0.019)and type of the liver graft that was transplanted (P = 0.017). In patients who were transplanted for HCC in the COVID-19 period, the use of grafts from the living donors was 13.3 times more frequent than the pre-COVID-19 period [odds ratio = 13.3; 95% confidence interval (CI): 0.74-240]. The rate of lymphovascular invasion in the explant pathologies of patients was found to be 2.54 times more frequent in patients who received operations during the COVID-19 period (odds ratio = 2.54; 95%CI:1.15-5.56).
At this the witch became so furious that she danced about and knocked everything to pieces that she could lay her hands upon, so that the splinters flew about the ears of the prince and princess, who now stood there in her own beautiful shape
Research conclusions
This study showed that there was only a modest change in the tumor biology during the COVID-19 pandemic. This shows the efficacy of our surveillance program that enabled transplanting patients with HCC according to conventional management protocols.
Oh. There s nothing wrong with it. It s brand new. We re closing the store is all. It s on clearance12 like everything else. I think that includes lifejackets, paddles and a bunch of fishing gear, too. I ll go check.
Research perspectives
We believe that the increased lymphovascular invasion rate in the present study was an observational variation because there is no change in the stages of the diseases between the two intervals. The DDLT rate in Turkey was already low, and it further decreased during the pandemic. However, we managed to preserve a high rate of LDLT. Therefore, it is important to develop a surveillance strategy for liver transplant centers. The liver transplantation for HCC is justified and safe provided that strict surveillance protocols are applied.
ACKNOWLEDGEMENTS
We would like to commend all health care professionals who were always in the frontline. They took the courage and responsibility of treating all patients during these hard times and despite risking their own lives. In addition, we would like to thank Brian I Carr, Ramazan Kutlu, Burak Isik, Nese Karadag,Murat Harputluoglu, Nuru Bayramov, Mustafa Dikilitas, Oztun Temelli, Muge Otlu, Ayse Nur Akatlı,Sinan Karatoprak, and Vedat Subasi, who participated in our online meetings as multidisciplinary liver tumor board member during this process, for their contributions.
And when the young man stood before the king, the king spoke6 to him and said, By your tricks and the pranks7 that you have played on other people, you have, in the eye of the law, forfeited8 your life
FOOTNOTES
Akbulut S and Ince V collected the data; Akbulut S performed the statistical analysis; Akbulut S and Sahin TT wrote the manuscript; Akbulut S, Sahin TT and Yilmaz S developed the study and reviewed the final version.
This study was reviewed and approved by the Inonu University institutional review board for non-interventional studies, No. 2021/2538.
Verbal and written consents were obtained from all HCC patients before the liver transplantation procedure.
The authors declare that they have no conflicts of interest regarding this study.
There are no additional data available for this study.
The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Turkey
Sami Akbulut 0000-0002-6864-7711; Tevfik Tolga Sahin 0000-0002-9132-6115; Volkan Ince 0000-0002-0714-490X; Sezai Yilmaz 0000-0002-8044-0297.
Fan JR
Filipodia
Some time after her mistress said to Catherine, I am obliged to go out for a long while, and must lock the house door, so that no thieves shall get in
Fan JR
杂志排行
World Journal of Clinical Cases的其它文章
- Diet and intestinal bacterial overgrowth: Is there evidence?
- Spontaneous liver rupture following SARS-CoV-2 infection in late pregnancy: A case report
- Metastasis of liver cancer to the thyroid after surgery: A case report
- Solitary primary pulmonary synovial sarcoma: A case report
- Knot impingement after arthroscopic rotator cuff repair mimicking infection: A case report
- Clear aligner treatment for a four-year-old patient with anterior crossbite and facial asymmetry: A case report
