lncluding video and novel parameter-height of penetration of external anal sphincter-in magnetic resonance imaging reporting of anal fistula
2022-06-08PankajGargBaljitKaurVipulYagnikSushilDawka
Pankaj Garg, Baljit Kaur, Vipul D Yagnik, Sushil Dawka
Pankaj Garg, Department of Colorectal Surgery, Garg Fistula Research Institute, Panchkula 134113, Haryana, India
Pankaj Garg, Department of Colorectal Surgery, Indus International Hospital, Mohali 140507,Punjab, India
Baljit Kaur, Department of Radiology, SSRD Magnetic Resonance Imaging Institute,Chandigarh 160011, Chandigarh, India
Vipul D Yagnik, Department of Surgical Gastroenterology, Nishtha Surgical Hospital and Research Center, Patan 384265, Gujarat, India
Sushil Dawka, Department of Surgery, SSR Medical College, Belle Rive 744101, Belle Rive,Mauritius
Abstract The main purpose of a radiologist’s expertise in evaluation of anal fistula magnetic resonance imaging (MRI) is to benefit patients by decreasing the incontinence rate and increasing the healing rate. Any loss of vital information during the transfer of this data from the radiologist to the operating surgeon is unwarranted and is best prevented. In this regard, two methods are suggested.First, a short video to be attached with the standardized written report highlighting the vital parameters of the fistula. This would ensure minimum loss of information when it is conveyed from the radiologist to the operating surgeon.Second, inclusion of a new parameter, the amount of external sphincter involvement by the anal fistula. This parameter is usually not included in the MRI report. This can be evaluated as the height of penetration of the external anal sphincter (HOPE) by the fistula. The external anal sphincter plays a pivotal role in maintaining continence. This parameter (HOPE) is distinct from the ‘height of internal opening’ and assumes immense importance as its knowledge is paramount to prevent damage to the external anal sphincter by the surgeon during surgery.
Key Words: Magnetic resonance imaging; Anal fistula; External anal sphincter; Video reporting;Incontinence
lNTRODUCTlON
Anal fistulas are associated with a high rate of recurrence and risk to the anal continence mechanism.The operating surgeons need to understand the exact position of the anal fistula and its relation to the anatomical structures in order to achieve high cure rate especially in complex anal fistulas. Magnetic resonance imaging (MRI) is the gold standard investigation used for anal fistulas. Usually, the MRI is interpreted by the radiologists who then send a written report to the operating surgeon and the surgeon performs the surgery after reading the radiologist’s report. Formats have been suggested for reporting the MRI in fistulas[1,2]. However, utility of MRI to the operating surgeon can be improved immensely if the two features discussed below (inclusion of an MRI video and addition of HOPE parameter) are added to MRI report (Table 1).
First, when only a written report is sent by the radiologist who has analyzed the MRI scans, then a lot of important information is lost. This happens because the three-dimensional picture created in the radiologist’s mind by the detailed visual analysis of the MRI scans cannot be replicated in the surgeon’s mind just by reading the text in the radiologist’s report. This loss of three-dimensional visual data can be prevented by sending a small video highlighting all relevant parameters along with the written report. Second, as discussed, the two main concerns in anal fistulas are recurrence and incontinence[3].It is a known fact that the recurrence risk of fistula is directly related to surgeon’s knowledge about the precise location of fistula tract’s internal opening (where the fistula opens into the anal canal)[4,5].On the other hand, the accurate assessment of the amount of external anal sphincter (EAS) involvement is key to prevent sphincter damage (incontinence)[6]. The importance of reporting the location of the internal opening has now been established[7], but the other equally important parameter, HOPE (height of penetration of external anal sphincter by the fistula) parameter is not reported by the radiologists(Figure 1). The EAS is mainly responsible for anal continence. HOPE parameter conveys the extent of involvement of the EAS to the operating surgeon and is thus pivotal to avoid damaging the EAS. The studies have demonstrated that when the surgeon performing the surgery is unsure of the accurate extent of EAS involvement, then the fistulotomy procedure is generally avoided and remains largely underutilized, even in simple anal fistulas, due to fear of incontinence in the mind of surgeons[8].Fistulotomy is the simplest procedure for low anal fistulas and is associated with the maximum cure rate (93%-99%) and no other procedure has been shown to have success rate comparable to fistulotomy[6,8]. Therefore, lack of knowledge of HOPE (EAS involvement) leads to a lower healing rate which can be prevented by proper MRI reporting.

Figure 1 Height of penetration of external sphincter parameter. Demonstration of height of penetration of external anal sphincter by the fistula tract in the patient included in accompanying video (Video 1). Approximately 2/3 of the external sphincter is involved by the fistula tract. The yellow arrow demonstrates the point of penetration of external anal sphincter by the fistula tract.
As the origin of most fistulas is at the level of the dentate line, the location of the internal opening in most of them is at that level only. The location of the internal opening does not accurately correspond to the amount of involvement of the EAS as penetration of the EAS by the fistula is often at a different level(Figure 1 and Video 1). Therefore, HOPE is the parameter which should be reported separately for helping the operating surgeon to precisely assess the amount of involvement of the EAS.
The level of understanding of fistula anatomy is greatly enhanced in the surgeon’s mind when a small video of MRI scan showing the fistula characteristics is send along with the written report (Video 1). The key points regarding the fistula characteristics can be highlighted by using a pointer in the video(Video 1). The fistula parameters which should be mentioned and highlighted in the video have been listed in Table 2. The MRI report should also be standardized as shown in Table 1. An example of a final written report (of the fistula shown in Video 1 has been included at the bottom of Table 1 to clarify the format).
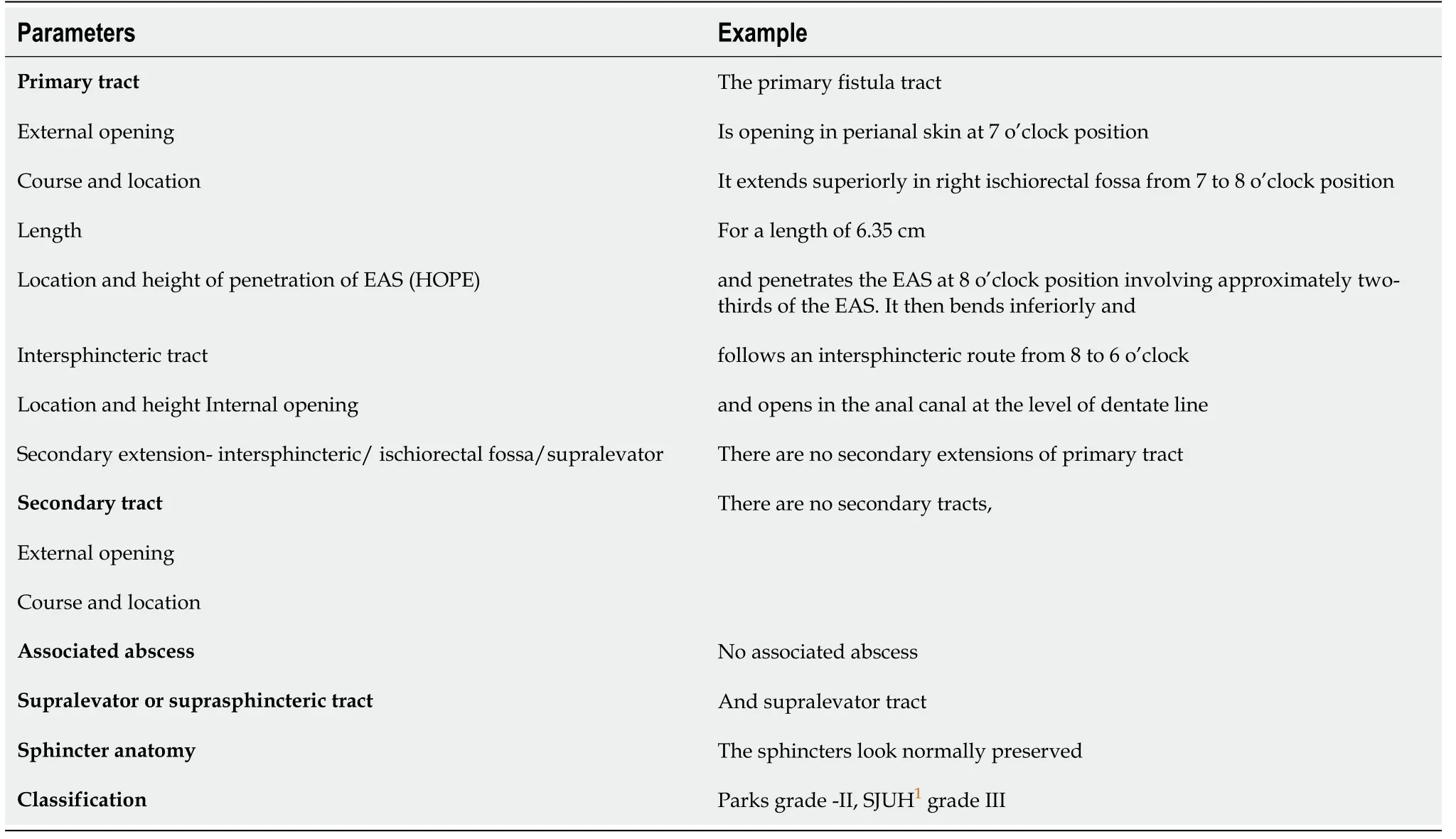
Table 1 Format for the written magnetic resonance imaging report
As can be seen, the novel parameter reported in this study, HOPE (height of penetration of external anal sphincter by the fistula tract) has also been incorporated in the video (Video 1) as well as the reportformat (Table 1) (Figure 1). This parameter (HOPE) conveys the amount of EAS involved by the fistula tract (Figure 1).

Table 2 Format for reporting the fistula magnetic resonance imaging in the video
The study concept was reviewed and approved by the Hospital-Institute Ethics Committee.
CONCLUSlON
This paper describes two novel additions to the MRI reporting of anal fistulas. The first is inclusion of a video along with the standardized written report (Tables 1 and 2, Video 1). This would prevent loss of vital three-dimensional data about the disease when the information is being transferred from the radiologist to the operating surgeon and would significantly enhance the surgeon’s understanding of the fistula anatomy. Second, when the HOPE parameter (height of penetration of external anal sphincter by the fistula) is incorporated in the video as well as written report, the risk of EAS damage would be drastically reduced and the success rate of the surgical procedure would also be enhanced. Therefore,HOPE should be reported as a separate parameter apart from the location of the internal opening. This format of MRI reporting (including a video) can also be stored on PACS (picture archiving and communication system)[9,10]. PACS provide storage and convenient access to medical images from where the clinician can see the report, images as well as the video as per their convenience[9,10].
FOOTNOTES
Author contributions:Garg P conceived and designed the study, collected, and analyzed the data, revised the data,finally approved and submitted the manuscript (Guarantor of the review); Kaur B and Yagnik VD collected, and analyzed the data, revised the data, finally approved and submitted the manuscript; Dawka S critically analyzed the data, reviewed and edited the manuscript, finally approved and submitted the manuscript
Conflict-of-interest statement:None for all the authors.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:India
ORClD number:Pankaj Garg 0000-0002-0800-3578; Baljit Kaur 0000-0002-3882-7578; Vipul D Yagnik 0000-0003-4008-6040; Sushil Dawka 0000-0002-9372-3683.
Corresponding Author's Membership in Professional Societies:American Society of Colon Rectum Surgeons; American Society of Gastrointestinal Endoscopic Surgeons; Endoscopic and Laparoscopic Surgeons of Asia; Association of Surgeons of India.
S-Editor:Wu YXJ
L-Editor:A
P-Editor:Wu YXJ
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- lmaging of acute appendicitis: Advances
- Laparoscopic-assisted endoscopic full-thickness resection of a large gastric schwannoma: A case report
- Surgical timing for primary encapsulating peritoneal sclerosis: A case report and review of literature
- Subacute liver and respiratory failure after segmental hepatectomy for complicated hepatolithiasis with secondary biliary cirrhosis: A case report
- Clinical outcomes of endoscopic resection of superficial nonampullary duodenal epithelial tumors: A 10-year retrospective,single-center study
- How to examine anastomotic integrity intraoperatively in totally laparoscopic radical gastrectomy? Methylene blue testing prevents technical defect-related anastomotic leaks