2型糖尿病患者睡眠呼吸暂停与糖尿病黄斑水肿相关性评估
2022-06-08朱双顾玲佳杨宏伟陶海英
朱双 顾玲佳 杨宏伟 陶海英

[摘要] 目的 探討2型糖尿病患者阻塞性睡眠呼吸暂停(OSA)与糖尿病黄斑水肿(DME)的关系。方法 前瞻性连续纳入2018年11月至2019年9月在台州市第一人民医院就诊的99例2型糖尿病患者,使用谱域光学相干断层扫描技术诊断DME。依据病情将患者分为DME组(DME+组,n=38)和无DME组(DME-组,n=61)。所有患者均进行多导睡眠图(PSG)检测。采用单因素和多因素logistic回归分析考察OSA是否是黄斑水肿的独立危险因素。结果 DME+组平均呼吸暂停低通气指数(AHI)[43.95(13.5,87.3)]高于DME-组[35.18(3.55,90.7)],差异有统计学意义(P<0.05)。DME+组患者中重度OSA患者呼吸暂停低通气指数高于DME-组(97.37% vs.78.69%),差异有统计学意义(P=0.001)。logistic多因素回归校正混杂因素后,AHI>15[OR(95%CI):4.52(1.47~12.01),P<0.001],动脉血氧饱和度低于90%的累积时间(CT90%)≤10%[OR(95%CI):6.39(1.25~32.69),P=0.026]是2型糖尿病发生DME的独立危险因素。AHI和CT90%诊断DME的曲线下面积分别为0.722和0.634,临界值分别为AHI≥37和CT90%≥10。结论 2型糖尿病患者AHI>37和CT90%≥10与DME高度相关。
[关键词] 阻塞性睡眠呼吸暂停;糖尿病性黄斑水肿;谱域光学相干断层扫描术;多导睡眠图
[中图分类号] R587.1 [文献标识码] B [文章编号] 1673-9701(2022)11-0041-04
[Abstract] Objective To investigate the relationship between obstructive sleep apnea-hypopnea(OSA) and diabetic macular edema(DME) in patients with type 2 diabetes mellitus. Methods A total of 99 patients with type 2 diabetes mellitus who visited Taizhou First People′s Hospital in Zhejiang Province from November 2018 to September 2019 were prospectively and consecutively included. DME was diagnosed using spectral-domain optical coherence tomography. Patients were divided into the DME group (DME+ group, n=38) and the non-DME group (DME- group, n=61) according to their condition. Polysomnogram (PSG) was performed in all patients. Univariate and multivariate logistic regression analyses were used to investigate whether OSA was an independent risk factor for macular edema. Results The mean apnea-hypopnea index (AHI) in the DME+ group (43.95[13.5,87.3]) was significantly higher than that (35.18[3.55,90.7]) in the DME- group and the difference was statistically significant (P=0.034). The number of patients with apnea-hypopnea index (AHI) > 30 in patients with moderate to severe OSA was higher in the DME+ group than in the DME- group (97.37% vs. 78.69%), and the difference was statistically significant (P=0.001). Logistic multivariate regression after adjustment for confounders showed AHI>15 (OR [95% CI]: 4.52 [1.47-12.01], P<0.001) and cumulative time of SPO2 below 90% (CT90%)≤10%( OR [95%CI ]∶6.39[1.25-32.69], P=0.026) were independent risk factors for DME in type 2 diabetes mellitus. The area under the curve for the diagnosis of DME was 0.722, and 0.634 for AHI and CT90%, respectively, and the cut-off values were AHI≥37 and CT90%≥10, respectively. Conclusion AHI>37 and CT90%≥10 are highly associated with DME in patients with type 2 diabetes mellitus.C48B0E84-2DC1-4D1C-8AA9-6FBABCF73493
[Key words] Obstructive sleep apnea-hypopnea; Diabetic macular edema; Spectral-domain optical coherence tomography; Polysomnogram
2 型糖尿病患者的阻塞性睡眠呼吸暂停低通气综合征(obstructive sleep apnea-hypopnea syndroms,OSAHS)患病率为23%~86%,高于一般人群[1]。糖尿病性黄斑水肿(diabetic macular edema,DME)约占糖尿病患者的5%,是导致糖尿病患者视网膜病变和视力损害的主要原因[2-4]。阻塞性睡眠呼吸暂停低通气综合征(obstructive sleep apnea-hypopnea,OSA)也可能参与DME的病理生理过程[5]。视网膜在黑暗中需氧量增加,夜间反复的呼吸功能受限可导致黄斑缺氧,导致促炎细胞因子和VEGF的产生增加,继而加重糖尿病性黄斑病变[6]。然而,很少有临床研究调查这两种疾病之间的关系。本研究旨在考察2型糖尿病患者睡眠呼吸暂停与糖尿病黄斑水肿的相关性,现报道如下。
1 资料和方法
1.1 一般资料
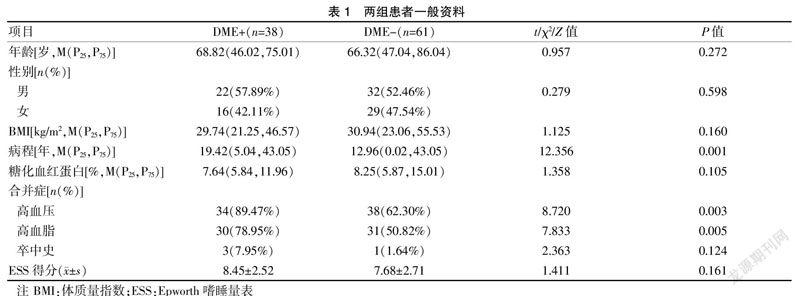
前瞻性纳入2018年11月至2019年9月间在浙江省台州市第一人民医院就诊的99例2型糖尿病患者。入组标准:①符合2型糖尿病的诊断标准[7-8];②年龄≥18岁。排除标准[9]:①有明确OSA病史或曾接受持续气道正压治疗;②慢性呼吸道疾病、自身免疫性疾病史[10]。本研究获得医院医学伦理委员会批准,所有患者均签署知情同意书。采集患者的人口学和常规临床资料。依据病情将患者分为DME患者组(DME+组,n=38)和无DME患者组(DME-组,n=61)。DME+组糖尿病病程、高血压、高血脂人数均高于DME-组,差异有统计学意义(P<0.01)。见表1。
1.2 方法
1.2.1 糖尿病黄斑水肿的诊断 使用谱域光学相干断层扫描(spectral domain optical coherence tomography,OCT)技术,Humphrey 2010 OCT(德国Zeiss公司)测量中心黄斑。患者眼睛常规散瞳15~20 min后,以黄斑中心凹为中心进行3次扫描,获取并记录黄斑部鼻下、鼻上、颞下、颞上区视四个象限距离黄斑中心凹1000 μm处的神经上皮层厚度均值,重复测量6组数据用于统计分析。黄斑中心凹厚度>170 μm者诊断为黄斑水肿[11]。
1.2.2 阻塞性睡眠呼吸暂停测量 ①Epworth嗜睡量表(Epworth sleepiness scale,ESS)测试[12]评估患者白天嗜睡程度。量表总分24分,0~9分属于正常,10~24分属于高危。②使用Embletta(冰岛Medeare Flaga)多导睡眠监测系统记录呼吸暂停低通气指数(apnea hypopnea index,AHI)、血氧减指数(oxygen desaturation index,ODI,指每小时血氧饱和度下降≥4%的次数)、最低血氧饱和度(min SaO2)、氧饱和度≤90%的累积时间占总监测时间的百分比(the cumulative time of SPO2 below 90%,CT90%)。CT90% 5%~10%为轻度缺氧,>10%且≤25%为中度缺氧,>25%为重度缺氧[13]。呼吸暂停低通气指数为≥5次/h诊断为阻塞性睡眠呼吸暂停。中度至重度OSA定义为AHI≥15次/ h,重度OSA定义为AHI≥30次/h[1,14]。
1.3 统计学方法
采用SPSS 23.0统计学软件进行统计学分析。连续变量采用t检验或Mann Whitney U检验,分类采用χ2检验或Fisher精确检验比较组间差异。单因素分析中P<0.20的变量进入多变量logistic回归分析考察OSA是否是2型糖尿病患者發生DME的独立危险因素。接受者操作特性曲线(receiver operating characteristic curve,ROC)分析AHI和CT90%诊断DME的灵敏度、特异度和诊断性能。双侧检验,P<0.05为差异有统计学意义。
2 结果
2.1 两组患者的多导睡眠图结果
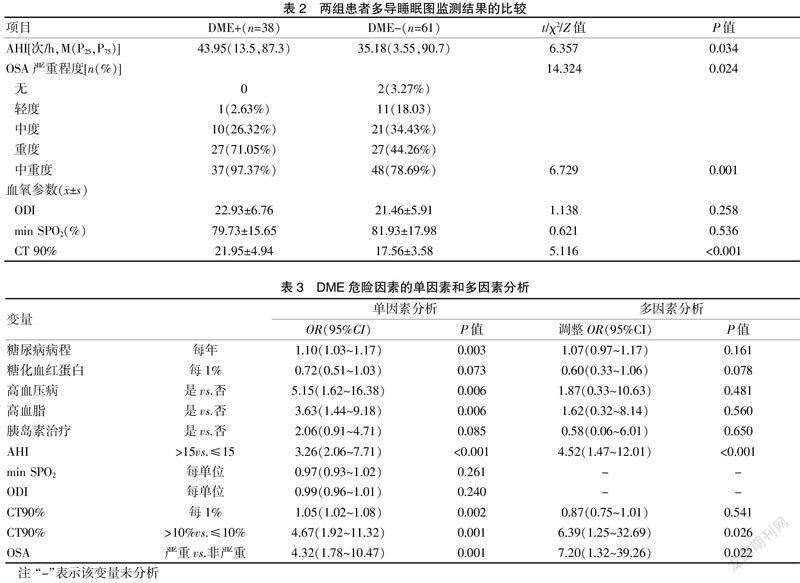
DME+组的平均AHI明显高于DME-组(P=0.034)。97.37%的DME+组患者和78.69%的DME-组患者属于中重度OSA(AHI≥15)(P=0.001)。见表2。
2.2 DME危险因素的回归分析
在多因素分析中,与DME相关的因素为严重OSA[OR(95%CI):7.20(1.32~39.26),P=0.022)],CT 90%高于10%[OR(95%CI):6.39(1.25~32.69),P=0.026]、AHI>15[4.52(1.47~12.01),P<0.001]。见表3。
2.3 AHI和CT90%的值对DME的诊断性能
根据AHI和CT90%诊断DME的ROC曲线,CT90%和AHI的曲线下面积分别为0.722和0.634。AHI的临界值为37,敏感度为68.6%,假阳性率为32.5%,特异度为67.5%;CT90%的临界值为10%,敏感度为67.9%,假阳性率为42.7%,特异度为57.3%。见图1。
3 讨论
本研究结果表明,DME+组患者的平均AHI及中重度OSA患者人数比例明显高于DME-组。AHI≥30和CT90%<10%是2型糖尿病发生DME的独立危险因素。尽管DME+组最低动脉血氧饱和度和氧减指数均较低,但差异无统计学意义。而CT90%与2型糖尿病患者发生DME具有独立相关性。这说明低血氧饱和度的累积时间是一个表示持续缺氧的指标,比单独的最低动脉血氧饱和度更能反映组织缺氧的持续状态。DME+组和DME-组之间的ESS评分比较,差异无统计学意义。ESS评分是一种反映患者白天嗜睡状态的量表,并不能直接反映患者夜间的呼吸睡眠状态,在评价糖尿病患者的DME时,与睡眠记录相结合可能会更全面地反映患者的睡眠状态。前期分析OSA与DME相关性的研究没有得出较为一致的结论[15-17]。这种结果的差异可能与研究者采用的OSA的定义、诊断测量方法以及是否考虑混杂因素等有关。一些生理病理假说可以解释这种联系。视网膜的新陈代谢需要大量的氧,尤其是在夜间需求更高。视网膜缺氧最容易影响黄斑等脆弱区域,导致炎性细胞因子和VEGF的产生,进而血-视网膜屏障的通透性增加[5,9,18-20]。C48B0E84-2DC1-4D1C-8AA9-6FBABCF73493
本研究的局限性首先在于樣本量较小。此外,这是一项横断面研究,因此无法纵向评估OSA发作的时间对DME的影响。
综上所述,2型糖尿病患者AHI>37和CT90%≥10与DME高度相关。建议对2型糖尿病患者常规进行PSG筛查,当发现AHI和CT90%均有增高时,要进行眼科检查排除DME。
[参考文献]
[1] 何权瀛,王莞尔.阻塞性睡眠呼吸暂停低通气综合征诊治指南(基层版)[J].中国呼吸与危重监护杂志,2015, 14(4):398-405.
[2] Fallahi A,Jamil DI,Karimi EB,et al. Prevalence of obstructive sleep apnea in patients with type 2 diabetes:A systematic review and meta-analysis[J].Diabetes Metab Syndr,2019,13(4):2463-2468.
[3] 李冰,叶俊杰.糖尿病黄斑水肿治疗的研究进展[J].中华眼科杂志,2018,54(8):625-630.
[4] Sunil B,Ashraf AP. Dyslipidemia in pediatric type 2 diabetes mellitus[J].Curr Diab Rep,2020,20(10):53.
[5] Lee MW,Lim HB,Kim MS,et,al. Effects of prolonged type 2 diabetes on changes in peripapillary retinal nerve fiber layer thickness in diabetic eyes without clinical diabetic retinopathy[J].Sci Rep,2021,11(1): 6813.
[6] Le HG,Shakoor A. Diabetic and retinal vascular eye disease[J].Med Clin North Am,2021,105(3): 455-472.
[7] 中华医学会糖尿病学分会.中国2型糖尿病防治指南(2017年版)[J].中国实用内科杂志,2018,38(4):292-344.
[8] 《中国高血压防治指南》修订委员会.中国高血压防治指南2018年修订版[J].心脑血管病防治,2019,19(1):6-49.
[9] Chiang JF,Sun MH,Chen KJ,et al. Association between obstructive sleep apnea and diabetic macular edema in patients with type 2 diabetes[J].Am J Ophthalmol,2021, 226(2):217-225.
[10] 中国成人血脂异常防治指南修订联合委员会.中国成人血脂异常防治指南(2016年修订版)[J].中国循环杂志,2016,31(10):937-950.
[11] 杨爱萍,汪浩.黄斑水肿对糖尿病性视网膜病变黄斑区光学相干断层扫描血管成像测量值的影响[J].眼科学报,2018,33(2):89-95.
[12] 彭莉莉,李进让,孙建军,等.Epworth嗜睡量表简体中文版信度和效度评价[J].中华耳鼻咽喉头颈外科杂志,2011,46(1):44-49.
[13] 孙会凤,张继华,周小慧,等.阻塞性睡眠呼吸暂停低通气综合征患者低氧血症与颈动脉内膜斑块形成的相关性分析[J].河北医科大学学报,2019,40(8):963-966.
[14] 美国睡眠医学会(高和,江晓丽编译).美国睡眠医学会睡眠及其相关事件判读手册[M].北京:人民军医出版社,2010:201-205.
[15] Bangh AM,Krogager C,Kristensen PL,et al. Effect of 12-week continuous positive airway pressure therapy on glucose levels assessed by continuous glucose monitoring in people with type 2 diabetes and obstructive sleep apnoea; A randomized controlled trial[J].Endocrinol Dia-betes Metab,2021,4(2):e00 148.
[16] Banerjee D,Leong WB,Arora T,et al. The potential ass-ociation between obstructive sleep apnea and diabetic retinopathy in severe obesity-the role of hypoxemia[J].PLoS ONE,2013,8(11):e79 521.
[17] Chen L,Tang W,Wang C,et al. Diagnostic accuracy of oxygen desaturation index for sleep-disordered breathing in patients with diabetes[J].Front Endocrinol(Lausanne),2021,12(2):e598 470.
[18] Pavone D,Clemenza S,Sorbi F,et al. Epidemiology and risk factors of uterine fibroids[J].Best Pract Res Clin Obstet Gynaecol,2018,46:3-11.
[19] Zhang R,Zhang P,Zhao F,et al. Association of diabetic microvascular complications and parameters of obstru-ctive sleep apnea in patients with type 2 diabetes[J].Diabetes Technol Ther,2016,18(7):415-420.
[20] Gu X,Luo X,Wang X,et al. The correlation between obstr-uctive sleep apnea and diabetic neuropathy:A meta-analysis[J].Primary Care Diabetes,2018,12(5):460-466.
(收稿日期:2021-05-14)C48B0E84-2DC1-4D1C-8AA9-6FBABCF73493
