Minimally invasive outpatient management of iliopsoas muscle abscess in complicated spondylodiscitis
2022-05-30VasilikiFesatidouEvangelosPetsatodisDimitriosKitridisPanagiotisGivissisEfthimiosSamoladas
lNTRODUCTlON
Iliopsoas muscle abscess (IPA) is a rare infective clinical condition often related to nonspecific symptoms and a variety of etiologies[1]. It was first described by Mynter in 1881 and was characterized as “acute psoitis”[2]. Two proposed mechanisms lead to IPA. Primary IPAs are caused by a hematogenous spread of an infective microorganism that leads to IPA formation due to the muscle’s rich vascularity, especially in immunocompromised patients. Secondary IPAs are developed by a contiguous spread of an intra-abdominal inflammatory process or by musculoskeletal conditions such as spondylodiscitis, sacroiliitis, or tuberculosis of the spine[1,3,4].
Spondylodiscitis is the most common form of spinal infection, affecting the intervertebral disc and the adjacent vertebral bodies and can present isolated or combined with other underlying conditions such as infections, malignancy, and immunosuppression[5]. Pyogenic spondylodiscitis can result in IPA due to direct expansion into the iliopsoas.
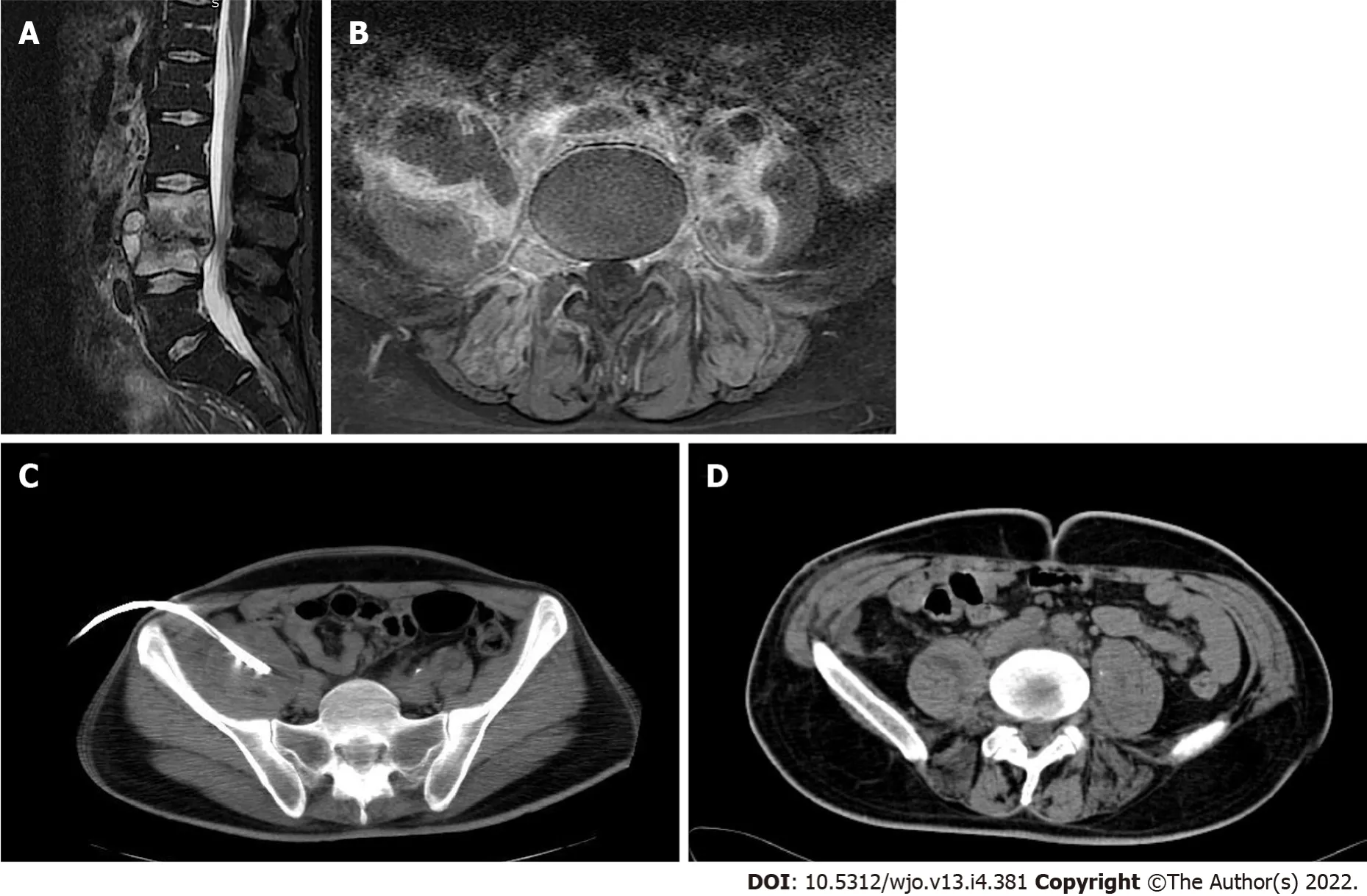
Symptoms of IPA may be insidious and nonspecific due to the location of the iliopsoas muscle, but the classical clinical presentation described in the literature includes the triad of fever, back pain, and limp[6,7]. Due to the atypical clinical features, diagnosis is oftentimes delayed leading to increased morbidity and mortality. Once an IPA is suspected, computed tomography (CT) scan is recommended, with a high sensitivity rate approaching 100%, whereas magnetic resonance imaging (MRI) of the spine is the most indicative imaging for spondylodiscitis[4,8]. There is no uniform treatment strategy for IPA. Traditionally, surgical drainage of the abscess along with a broad-spectrum antibiotic treatment was the preferred treatment[1,9,10]. However, more recent literature reports that the percutaneous CT-guided abscess drainage is a safe and equally effective alternative[1,8,11]. The purpose of the current study was to present and evaluate a case series of 8 patients diagnosed with spondylodiscitis complicated with IPA. The patients were managed with antimicrobial therapy, minimally invasive percutaneous CTguided drainage, and the addition of a short-term drain insertion in an outpatient setting.
MATERlALS AND METHODS
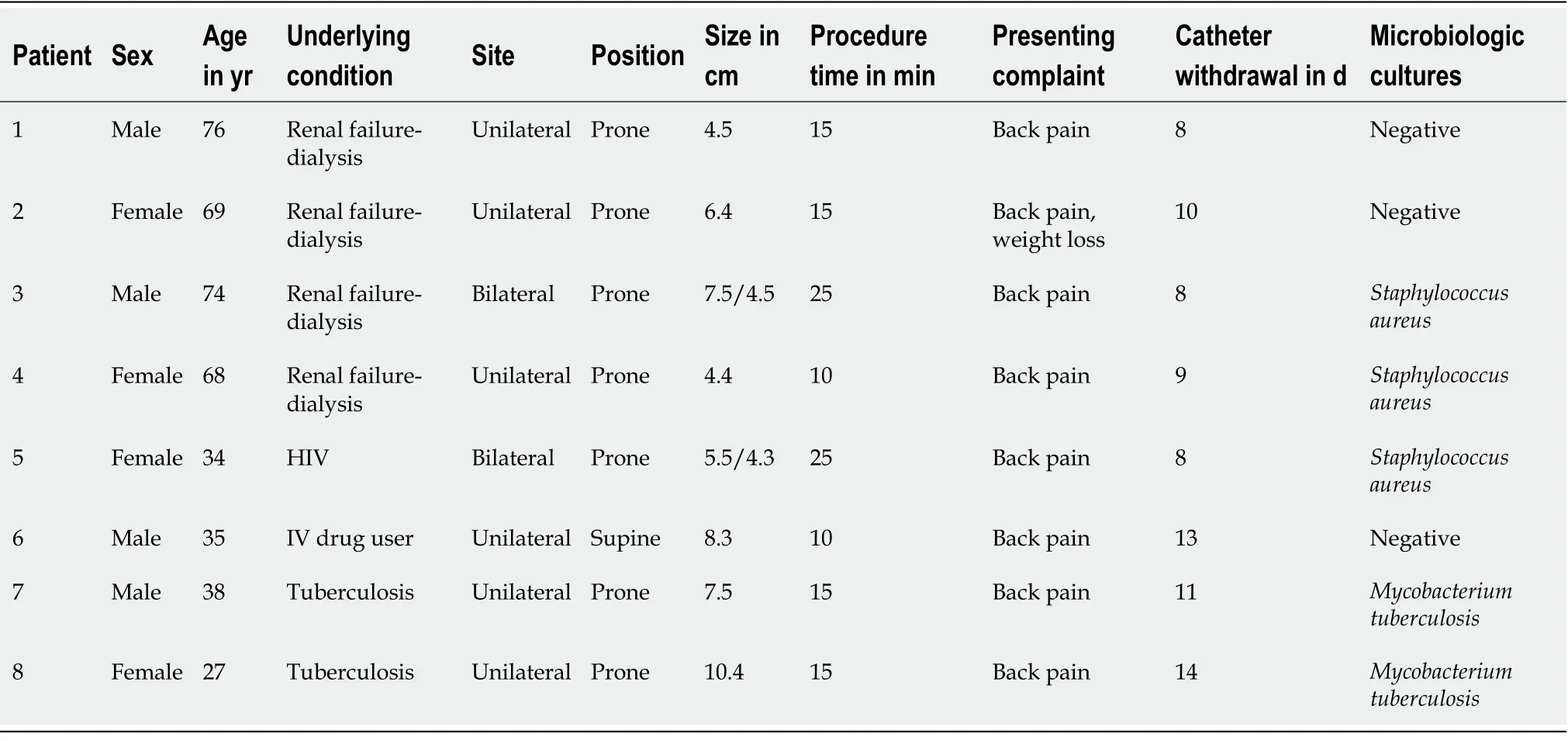
A retrospective collection and analysis of all radiologically diagnosed cases of IPA that were treated with CT-guided percutaneous drainage from 2016 to 2020 in the department of Interventional Radiology of a tertiary University hospital was performed. All cases initially presented to the spinal outpatient clinic complaining of back pain and were diagnosed with spondylodiscitis and IPA formation after an MRI and a CT scan. Records were extracted from the Interventional Radiology department’s database. Data were reviewed for patient demographics, underlying conditions, isolated microorganisms, antibiotic regimes used, abscess size, days until the withdrawal of the catheter, and final outcome.
All abscesses were defined as secondary IPAs due to the concurrent presence of spondylodiscitis. Two patients were diagnosed specifically with tuberculosis of the spine. There was no neurological compromise, spinal instability, or bone deformity present due to spondylodiscitis.
For the first time she succeeded well, for the people were glad to buy the woman s wares27 because she was good-looking, and they paid her what she asked; many even gave her the money and left the pots with her as well. So they lived on what she had earned as long as it lasted, then the husband bought a lot of new crockery. With this she sat down at the corner of the market-place, and set it out round about her ready for sale. But suddenly there came a drunken hussar28 galloping23 along, and he rode right amongst the pots so that they were all broken into a thousand bits. She began to weep, and did now know what to do for fear. Alas! what will happen to me? cried she; what will my husband say to this?
CT-guided percutaneous drainage
All draining procedures were performed by direct insertion of a 12 Fr pigtail catheter into the abscess cavity. Before the procedure, a CT and MRI scan were performed. Values of international normalized ratio less than 1.5 and platelet count greater than 50000/μL were required to proceed with the drainage, and antiplatelet or anticoagulation medication had to be discontinued accordingly. Patients were placed in the prone position in most cases (7 out of 8 patients). The placement decision was made depending on the best approach to the abscess cavity. All procedures were performed under local anesthesia and aseptic conditions. After an initial CT scan for approach planning, the trocar pigtail catheter was advanced into the abscess cavity under CT guidance. When the trocar reached the middle of the fluid collection it was withdrawn while the catheter was advanced and secured in position (Figure 1). Manual aspiration of the fluid was then performed, and the catheter was connected to a drainage bag. The inserted drain was removed if there was no drainage for 48 h.
RESULTS
A total of 8 patients that underwent CT-guided percutaneous IPA drainage were included in the study (Table 1). Their mean age was 52.6 ± 20.8-years-old, and there were six unilateral and two bilateral cases, a total of 10 abscesses. All cases were secondary; six were in immunocompromised patients [renal failure, HIV, intravenous (IV) drugs] with spondylodiscitis and two were in patients diagnosed with tuberculosis of the spine.
All patients presented at the spine outpatient clinic complaining of back pain for at least 3 mo with worsening at night, and 1 patient also mentioned weight loss. At clinical examination, there was local sensitivity and palpable muscle spasm found in all patients with no neurological compromise. All patients remained afebrile. From the laboratory investigation, there was an increase in inflammatory markers (C-reactive protein and erythrocyte sedimentation rate).
Treatment success was marked by clinical and laboratory improvement along with radiological confirmation of recession of the abscess and eventually catheter removal. All patients were clinically evaluated 6 mo after the end of their treatment.
The poor betrothed19 bride dressed herself entirely20 in black,25 and when she thought of her future bridegroom, tears came into her eyes. Nothing but contempt and mockery fell to her lot from her sisters. Take care, said the eldest, if thou givest him thy hand, he will strike his claws into it. Beware! said the second. Bears like sweet things, and if he takes a fancy to thee, he will eat thee up. Thou must always do as he likes, began the elder again, or else he will growl7. And the second continued, But the wedding will be a merry one, for bears dance well. 26 The bride was silent, and did not let them vex21 her. Bearskin, however, travelled about the world from one place to another, did good where he was able,27 and gave generously to the poor that they might pray for him.
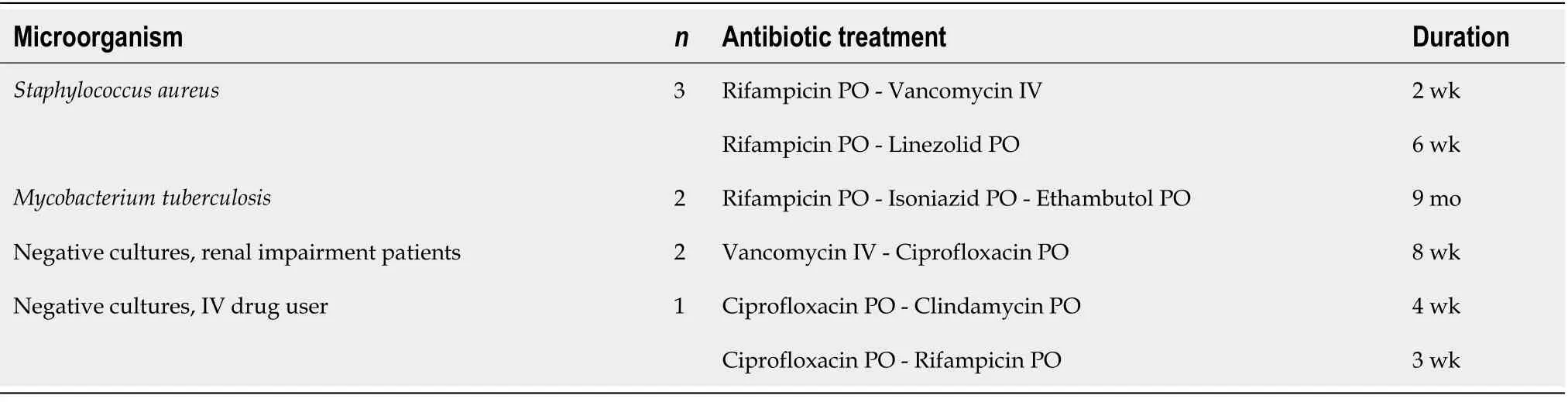
Microbiology samples from the abscess fluid were sent in all cases.was isolated in 3 cases,was isolated in 2 patients, and there was no specific microorganism isolated in 2 renal impairment/dialysis patients and 1 IV drug user. All patients initially received empiric antibiotic therapy with ciprofloxacin and clindamycin orally. After the culture results, patients withculture isolation received a targeted 2-wk course of intravenous vancomycin and oral rifampicin with daily outpatient visits, followed by oral linezolid and rifampicin for another 6 wk. The tuberculosis patients underwent a 9-mo antimicrobial treatment with oral isoniazid, ethambutol, and rifampicin, whereas the patients with no specific microorganism isolated received an 8-wk empiric antibiotic treatment as presented in Table 2. All abscesses were successfully drained on the first attempt, and all patients had a complete resolution of symptoms. There were no recurrences at the 6-mo follow-up.
DlSCUSSlON
Oh, Queen, thou art fairest of all I see,But over the hills, where the seven dwarfs dwell,Snow-white is still alive and well,And none is so fair as she.
The clinical triad of IPA symptoms as described by Mynter[2] in 1881 includes back pain, limping, and fever. Subsequent studies have identified more nonspecific symptoms such as weight loss, lower extremity pain, lower extremity edema, gastrointestinal symptoms, and a palpable mass[8]. The laboratory findings include elevated white blood cell count, C-reactive protein, and erythrocyte sedimentation rate as well as anemia[3,4]. In the present case series, none of the patients presented with the typical IPA symptomatology. The patients’ underlying conditions along with the raised inflammatory markers guided the physicians to suspect an inflammatory condition of the spine.
The final diagnosis of IPA is confirmed by the imaging findings. Several studies recommend ultrasound as the initial radiological investigation. However, it is an operator-dependent procedure with a low diagnostic rate[1,9,14]. CT scan is considered to be the “gold standard” for a definitive diagnosis of IPA, and MRI adds more detailed imaging of the abscess wall, the soft tissues, and the surrounding structures without the need for IV contrast infusion[3,15-17]. Both MRI and CT scans were performed in the current study and revealed signs of spondylodiscitis with unilateral or bilateral IPA formation in all patients. Although IPA is mainly described as an outcome of spondylodiscitis[7], literature also describes spondylodiscitis as a complication of an established IPA[18]. Therefore, it could not be clearly stated which condition was presented first. Spondylodiscitis, however, did not require invasive treatment in contrast to the IPA formation.
He rubbed his eyes and pinched himself, and when he was quite sure he was not dreaming he said to a man who was smoking his pipe before the door, Where am I? Where are you? Can t you see? Before the King s palace, of course
The literature traditionally suggests early surgical management of the IPA, which suggests a long inhospital stay. The surgical procedure of choice, according to Ricci[9] in 1986, was abscess drainage through a lower abdominal muscle-splitting, extraperitoneal incision. In more recent years, with the evolution of interventional radiology, minimally invasive percutaneous drainage of retroperitoneal abscesses, including IPA, is the treatment method of choice[11]. This approach is preferred especially for immunocompromised patients, as it eliminates the need for general anesthesia and is also associated with a shorter hospital stay, minimizing morbidity and mortality. There is currently no literature describing the management of such patients with a drain insertion in an outpatient setting. In the current series, all patients were managed as outpatients. All patients underwent CT-guided drainage and drain insertion without delay from the time of diagnosis. The drain insertion increased the success rate of the drainage, and no repeat procedures were necessary.
The diagnosis was confirmed by MRI followed by CT. According to imaging calculations, the mean abscess size was 6.3 ± 2.1 cm. There was no bone deformity or spinal degeneration observed. The drainage procedure was arranged immediately and performed in the next 1-3 d from the initial diagnosis. A 12 Fr pigtail drain was inserted in all cases, as previously described. The average time until the withdrawal of the catheter was 10 ± 2 d.
Empiric antibiotic therapy should cover againstand gram-negative and grampositive microorganisms, including bowel flora and common urinary tract infection bacteria, and targeted therapy should be commenced immediately after the culture results[14]. For mycobacterial infections, a 9-mo conventional antituberculosis therapy was applied. For non-mycobacterial infections, as all cases presented with vertebral involvement, the minimum duration of the antibiotic treatment was 8 wk, including at least 2 wk of IV vancomycin, and prolonged according to laboratory and radiological findings. Those receiving IV vancomycin visited the outpatient clinic daily for the first 2 wk for the infusions.
The drain catheter remained in place until no drainage was observed for 2 consecutive days. A follow-up CT scan was performed between days 7 and 14 to confirm abscess recession.
The current study has several limitations. First, it is a single-center study of a small pilot patient group, which reflects the rarity of the condition. Second, no control group was recruited. Moreover, the retrospective study design might introduce recall or patient selection bias.
You want to sharpen up on defending against crosses from the left, I told him, that goal as got in on Saturday wouldn t ave appened! Mark my words.
CONCLUSlON
Complicated spondylodiscitis with IPA formation in immunocompromised patients could be managed in an outpatient setting.
ARTlCLE HlGHLlGHTS
Research background
There has been an evolution in the management of complicated spondylodiscitis with iliopsoas muscle abscess (IPA) formation through the years and computed tomography (CT)-guided drain insertion with antibiotic therapy being the current practice.
We present a case series of 8 patients suffering from spondylodiscitis complicated with IPA, successfully treated with a minimally invasive approach of combined percutaneous abscess drainage with drain insertion and antibiotic therapy. Immunosuppression is the predominant underlying condition in IPA and may be responsible for the insidious presenting signs and symptoms[9]. In the current series, there was a higher prevalence of IPA in patients that were on renal dialysis, immunocompromised by HIV, or IV drug users. Moreover, tuberculosis is linked to secondary IPA due to vertebral involvement[11-13]. Although tuberculosis is rare, there were 2 cases of secondary IPA in patients with tuberculosis of the spine.
Research motivation
The minimally invasive outpatient management of IPA is a safe and effective approach with a high success rate and low morbidity.
Research objectives
The purpose of the current study was to describe the care management of complicated spondylodiscitis.
Research methods
A 4-year retrospective collection and analysis of all radiologically diagnosed cases of IPA that were treated with CT-guided percutaneous drainage. Data included patient demographics, underlying conditions, isolated microorganisms, antibiotic regimes used, abscess size, days until the withdrawal of the catheter, and final outcome. All draining procedures were performed by direct insertion of a 12 Fr pigtail catheter into the abscess cavity.
Also note that the prince is not called Prince Charming in the original tale. Walt Disney popularized the name with its usage in his film version of Cinderella.Return to place in story.
Research results
Here on the heath were riches unknown to him until now; for flowers, blackberries, andbilberries were to be found in profusion, so large and sweet that whenthey were crushed beneath the tread of passers-by the heather wasstained with their red juice
Research conclusions
The minimally invasive outpatient management of IPA, which combines CT-guided percutaneous drainage and placement of a drain with proper antibiotic treatment, proved to be a safe and effective approach with a high success rate and low morbidity.
Research perspectives
More studies should be performed in order to prove the cost effectiveness and the decreased morbidity of the minimally invasive outpatient management of these patients.
All 8 patients were diagnosed with IPA formation secondary to complicated spondylodiscitis, and two of them were diagnosed with spinal tuberculosis. All 8 patients showed complete recession of the symptoms and radiological findings after the CT-guided abscess drainage and the long-term antibiotic therapy. The microbiology cultures identified Staphylococcus aureus in 3 cases and Mycobacterium tuberculosis in 2 cases and were negative in the remaining 3 cases. There was no need for patient hospitalization.
Fesatidou V wrote the manuscript; Kitridis D reviewed the manuscript, performed a critical revision, and submitted the manuscript; Petsatodis E acquired and analyzed the data; Samoladas E and Givissis P supervised the study and contributed to patient care.
The study was approved by the Institutional Review Board.
All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
All authors have nothing to disclose.
No additional data are available.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Then the lid sprang up to the right, and the princess came out, straight over him, and rushed round the church, howling and shrieking33 Sentry, where are you? Sentry, where are you? She went towards the altar, and right up to it, but there was no one there; then she screamed again,My father has set no sentry in, War and Pest will now begin
Greece
Vasiliki Fesatidou 0000-0002-9787-6548; Evangelos Petsatodis 0000-0002-6252-1130; Dimitrios Kitridis 0000-0002-6063-8650; Panagiotis Givissis 0000-0002-8649-1159; Efthimios Samoladas 0000-0002-1892-7707.
But the harder she pulled the firmer seemed the plant, and at last, determined2 not to be beaten, she gave one great tug3, and the rosemary remained in her hands
Wang JL
Filipodia
Wang JL
杂志排行
World Journal of Orthopedics的其它文章
- Existing fixation modalities for Jones type fifth metatarsal fracture fixation pose high rates of complications and nonunion
- lntegrity of the hip capsule measured with magnetic resonance imaging after capsular repair or unrepaired capsulotomy in hip arthroscopy
- Direct anterior approach hip arthroplasty: How to reduce complications - A 10-years single center experience and literature review
- Comparing complications of outpatient management of slipped capital femoral epiphysis and Blount’s disease: A database study
- ls it necessary to fuse to the pelvis when correcting scoliosis in cerebral palsy?
- Lateral epicondylitis: New trends and challenges in treatment