肠内营养护理指引在脑外伤危重患者中的实施价值
2022-04-28杨芳
杨芳
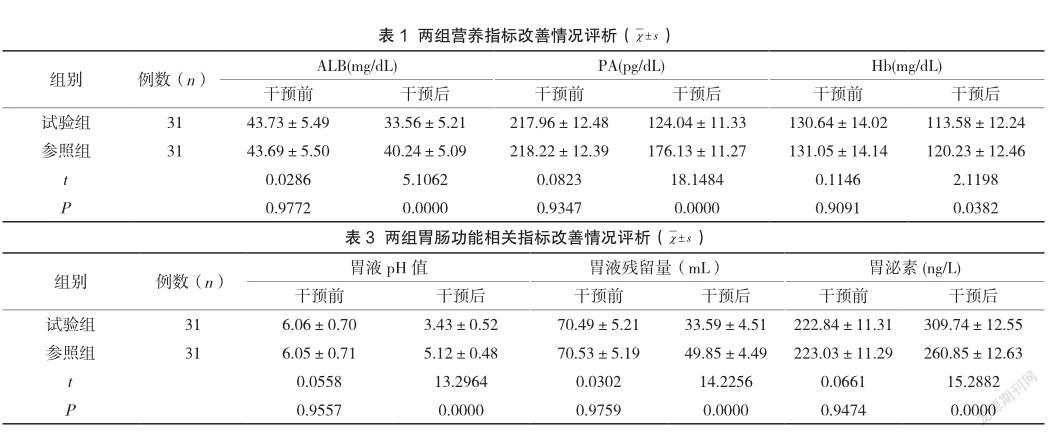
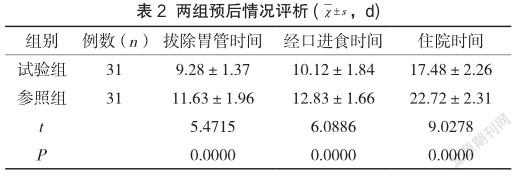
【摘 要】目的:研究、討论脑外伤危重症患者护理中,将肠内营养护理作为方案的临床意义。方法:选取2020年3月至2021年10月的脑外伤危重患者62例,患者分至不同组别,执行奇偶分组法。其中31例归至参照组,脑外伤常规护理。其余31例纳入试验组,场内营养护理。对两组营养指标改善情况、预后情况、胃肠功能相关指标改善情况、并发症发生情况进行统计、处理。结果:(1)各项营养指标经由分析可知,干预前,参照组、试验组数据分布较为均衡(P>0.05)干预后,试验组ALB(血浆白蛋)、PA(血浆前白蛋白)、Hb(血红蛋白)水平均下降,且较参照组低(P<0.05)。(2)各项预后情况指标经由分析可知,拔除胃管、经口进食、住院时间方面,均为试验组数值更小(P<0.05)。(3)各项胃肠功能相关指标经由分析可知,干预前,参照组、试验组差异性较弱(P>0.05)。干预后,试验组胃液pH值、胃液残留量比参照组低,胃泌素水平比参照组高(P<0.05)。(4)各项并发症指标经由分析可知,感染、胃出血、腹泻等发生概率方面,均为参照组更高(P<0.05)。结论:脑外伤危重患者护理中,将肠内营养护理护理作为措施,价值显著。患者胃肠功能提升的同时,营养指标得到改善,并且并发症发生概率减少,预后效果优异。
【关键词】脑外伤;肠内营养护理;危重;临床价值
The implementation value of enteral nutrition nursing guidelines in critical patients with brain trauma
YANG Fang
Taizhou Hospital of Traditional Chinese Medicine, Taizhou, Jiangsu 225300, China
【Abstract】Objective: To study and discuss the clinical significance of enteral nutrition nursing as a scheme in nursing critical patients with brain trauma. Methods: From March 2020 to October 2021, 62 critically ill patients with brain trauma were enrolled. Patients were divided into different groups, and parity grouping was performed. Among them, 31 cases were assigned to the reference group and received routine nursing care for traumatic brain injury. The remaining 31 cases were included in the experimental group, and nutrition nursing was performed on site. The improvement of nutritional indexes, prognosis, improvement of gastrointestinal function related indexes and occurrence of complications in the two groups were counted and processed. Results: (1) According to the analysis of various nutritional indexes, before the intervention, the data distribution of the reference group and the experimental group was relatively balanced(P>0.05).After the intervention, the levels of ALB (plasma white egg), PA (plasma prealbumin) and Hb (hemoglobin) in the experimental group decreased, and were lower than those in the reference group(P<0.05).(2) According to the analysis of various prognostic indicators, the values of extubation, oral feeding and hospital stay in the experimental group are smaller(P<0.05).(3) The analysis of gastrointestinal function related indexes shows that before the intervention, the difference between the reference group and the experimental group is weak(P>0.05).After the intervention, the gastric juice pH and gastric juice residue in the experimental group were lower than those in the reference group, and the gastrin level was higher than that in the reference group(P<0.05).(4) Through the analysis of various complications indicators, it can be seen that the occurrence probability of infection, gastrorrhagia and diarrhea is higher than that of the reference group(P<0.05).Conclusion: In the nursing of critical patients with brain trauma, enteral nutrition nursing is a significant measure. The patients’ gastrointestinal function was improved, the nutritional index was improved, the probability of complications was reduced, and the prognosis was excellent.
【Key Words】Brain trauma; Enteral nutrition nursing; Critical; Clinical value
脑外伤在临床较为多见,患者多处于昏迷状态,严重影响代谢功能。机体代谢异常可诱发营养不良,进而削弱免疫功能,引发一些列并发症[1]。为此,予以脑外伤危重患者肠内营养护理非常关键。临床研究发现,肠内营养支持可恢复患者肠道健康,纠正代谢紊乱[2]。本研究选入62例脑外伤危重患者,对肠内营养护理应用其中的临床意义进行研究、分析,报告如下。
1.1 临床资料
录入对象:脑外伤危重患者,62例。录入最初、最终时间:2020年3月、2021年10月。奇偶分组法分组。参照组31例,男16例,女15例,年龄26岁~66岁,平均年龄(40.52±1.17)岁;试验组31例,男17例,女14例,年龄25岁~65岁,平均年龄(40.39±1.22)岁。检验、评析两组常规资料,未见突出差异(P>0.05),研究意义存在。选入根据:(1)处于昏迷状态患者。(2)存在意识障碍患者。(3)自愿参与本研究患者。排除根据:(1)伴有感染性疾病患者。(2)伴有胃肠道疾病患者。
1.2 方法
参照组:常规护理。护理人员予以患者肠外营养支持。建立静脉通道,输注氨基酸、葡萄糖等。干预1周后,置入胃管,采用鼻饲肠内营养供给方案。
试验组:予以患者肠内营养护理方案,具体内容如下表述:(1)置管。脑外伤危重患者多处于昏迷状态,并且无意识。因此,在置管时需要两名或两名以上护理人员相互配合。(2)营养物质提供。予以患者营养液前,需要对其进行加温处理,目的是减少肠痉挛发生。(3)肠内营养基础护理。营养液输注前,护理人员需要对其浓度、用量进行调整,输注过程中应确保速度合适。
1.3 观察指标
对两组营养指标改善情况、预后情况、胃肠功能相关指标改善情况、并发症发生情况进行统计、处理。
1.4 统计学方法
采用SPSS 21.0统计学软件进行数据分析。计数资料采用(%)表示,进行χ2检验,计量资料采用(χ±s)表示,进行t检验,P<0.05为差异具有统计学意义。
2.1 两组营养指标改善情况评析
各项营养指标经由分析可知,干预前,参照组、试验组数据分布较为均衡(P>0.05)。干预后,试验组ALB、PA、Hb水平均下降,且较参照组低(P<0.05),见表1。
2.2 两组预后情况评析
各项预后情况指标经由分析可知,拔除胃管、经口进食、住院时间方面,均为试验组数值更小(P<0.05),見表2。
2.3 两组胃肠功能相关指标改善情况评析
各项胃肠功能相关指标经由分析可知,干预前,参照组、试验组差异性较弱(P>0.05)。干预后,试验组胃液pH值、胃液残留量比参照组低,胃泌素水平比参照组高(P<0.05),见表3。
2.4 两组并发症发生情况评析
各项并发症指标经由分析可知,感染、胃出血、腹泻等发生概率方面,均为参照组更高(P<0.05),见表4。

脑外伤多由交通事故、跌倒等外力作用导致。脑外伤患者存在不同程度的昏迷症状。相关研究发现,脑外伤患者在昏迷状态下,机体代谢功能难以正常发挥,进而导致脂肪、能量被过度消耗。在此情况下,患者机体免疫功能难以对抗病毒、细菌入侵,最终诱发感染,影响预后效果[3]。
总而言之,在脑外伤危重患者护理中,采用营养肠内营养护理干预方案,效果理想。除改善患者胃肠道功能、营养状况外,还可减少并发症发生,缩短患者住院时间。
参考文献
[1] 王梦寒,杜娟,陈璐瑶,等.早期肠内营养护理对脑外伤昏迷患者营养指标及免疫功能的影响[J].实用妇科内分泌电子杂志,2020,7(28):83-84.
[2] 杨楠.早期肠内营养护理对脑外伤昏迷患者的效果探讨护理[J].中国医药指南,2020,18(15):249-250.
[3] 仇尔宁,苏杭,容耔耘.生长激素联合肠内营养对脑外伤昏迷患者营养状况的影响研究[J].吉林医学,2020,41(1):145-147.
