半枝莲联合针灸对2型糖尿病大鼠肝脾肺组织结构的保护作用
2022-04-21鲜淼李玉洁范莹瑛陈宇鹏唐丽田春洋宋睿乐周洪旭陈正礼方静
鲜淼 李玉洁 范莹瑛 陈宇鹏 唐丽 田春洋 宋睿乐 周洪旭 陈正礼 方静

摘要:【目的】明確半枝莲醇提物联合针灸对2型糖尿病(T2DM)的治疗效果,为动物T2DM提供有效的治疗手段,进而保障宠物业的健康发展。【方法】选取60只4周龄的SPF级近交系Wistar雄性大鼠随机分为2组,健康对照组(H组)15只和建模组(M组)45只;链脲佐菌素(45 mg/kg)联合高糖高脂诱导构建T2DM大鼠模型,建模成功后将其随机分为模型对照组(M组,15只)、半枝莲治疗组(S组,15只)及半枝莲联合针灸治疗组(A组,15只,针灸穴位包括脾俞、肾俞、三阴交和足三里)。对A组和S组进行3个疗程(每疗程6 d)的治疗,分别于治疗第7、14和21 d采集各处理组大鼠的尾静脉血测定空腹血糖(FBG),同时各处理组分别处死5只大鼠,取肝脏、脾脏和肺脏固定后制作石蜡切片,肝脏和脾脏采用HE染色,肺脏采用HE染色和Masson染色,观察其组织结构病理变化。【结果】与H组相比,M组大鼠的体重极显著下降(P<0.01,下同),而FBG极显著升高;肝脏细胞由水肿发展为脂肪变性或局灶性坏死,炎症细胞浸润逐渐增强;脾脏组织局部细胞坏死,红髓和白髓分布混乱,淋巴细胞减少且排列紊乱;肺脏肺泡内出血,支气管黏膜下层和血管壁胶原纤维增生,最终导致部分肺泡萎陷或实变消失。与M组相比,A组和S组大鼠的体重呈增长趋势,至治疗第21 d极显著升高,而FBG在治疗第14和21 d均极显著降低;肝脏脂肪变性得到改善、水肿减轻、炎症细胞浸润减少;脾脏红髓和白髓结构、生发中心均逐渐趋于正常,淋巴细胞数量和脾小结数量均增多,且A组大鼠的增加数量多于S组大鼠;肺脏内出血减轻、炎症细胞减少,A组大鼠肺脏的肺间隔增厚程度低于S组大鼠。【结论】STZ联合高脂高糖诱导T2DM大鼠模型稳定,能对大鼠肝脏、脾脏和肺脏造成损伤。半枝莲或半枝莲联合针灸治疗对T2DM大鼠肝脏、脾脏和肺脏组织结构均具有较好的改善效果,且以针灸配合半枝莲的效果更优。
关键词: 大鼠;2型糖尿病(T2DM);半枝莲;针灸;肝脏;脾脏;肺脏;组织结构
中图分类号: S853.619 文献标志码: A 文章编号:2095-1191(2022)01-0238-10
Protective effects of Sculellaria barbata combined with acupuncture on the structure of liver, spleen and lung
in type 2 diabetes mellitus rats
XIAN Miao1, LI Yu-jie1, FAN Ying-ying1, CHEN Yu-peng1, TANG Li1*,TIAN Chun-yang1,2,
SONG Rui-le1,3, ZHOU Hong-xu1, CHEN Zheng-li1, FANG Jing1
(1College of Veterinary Medicine, Sichuan Agricultural University/Key Laboratory of Animal Disease and Human Health of Sichuan Province, Chengdu 611130, China; 2Sichuan Liziping National Nature Reserve Administration, Yaʼan,Sichuan 625400, China; 3Animal Husbandry and Veterinary Station of Yingshan County,
Nanchong, Sichuan 637700, China)
Abstract:【Objective】To explore the therapeutic effect of Sculellaria barbata alcohol extract combined with acupuncture on type 2 diabetes mellitus (T2DM) in rats, so as to provide effective treatment for animal T2DM and to ensure the healthy development of the pet industry. 【Method】 A total of 60 male SPF Wistar rats aged four weeks were randomly divided into two groups: 15 in the healthy control group (group H) and 45 in the modeling group (group M); Rat T2DM was modeled by the administration of streptozotocin(STZ, 45 mg/kg) combined with a high sugar and lipid diet. Rats successfully modeled were randomly divided into the model control group (group M with 15 rats), S. barbata treatment group (group S with 15 rats) and S. barbata combined with acupuncture treatment group (group A with 15 rats, and the acupuncture points were Pishu, Shenshu, Sanyinjiao and Zusanli). Group A and group S were treated for 3 courses with 6 d per course. The caudal venous blood were collected to measure fasting blood glucose (FBG) on the 7th, 14th and 21st days of treatment. Simultaneously, 5 rats in each treatment group were killed and their liver, spleen and lung were fixed and paraffin sections prepared. The pathological changes in organizational structure were observed in the liver and spleen stained with HE, while the lung was stained with HE and Masson. 【Result】Compared with group H, the weight of rats in group M decreased significantly(P<0.01, the same below), while FBG increased significantly; liver cells developed from edema to steatosis or focal necrosis and the infiltration of inflammatory cells increased gradually; the spleen tissue showed local cell necrosis, the distribution of red pulp and white pulp was chaotic and lymphocytes appeared to decline in number with a disordered arrangement; pulmonary alveoli displayed hemorrhaging with collapsed or absent alveoli with consolidation and collagen fibers in the bronchial submucosa and vascular wall were more prolific.Compared with group M, the weight of rats in group A and group S showed an increasing trend and increased significantly on the 21st day of treatment, while FBG decreased significantly on the 14th and 21st days of treatment; hepatic steatosis was improved, edema was reduced and infiltration of inflammatory cells was reduced; the structure and germinal center of red pulp and white pulp of spleen gradually tended towards the healthy control and the number of lymphocytes and splenic nodules increased with a higher increase in group A than in group S; lung internal hemorrhaging and inflammatory cells were decreased; the thickening degree of the pulmonary septum in group A was lower than that in group S. 【Conclusion】The model of T2DM in rats induced by STZ combined with a high lipid and high sugar diet effectively and stably induces T2DM symptoms with damage to the liver, spleen and lung. S. barbata alone or combined with acupuncture both improve the organizational structure of the liver, spleen and lung in T2DM symptomatic rats, while the effect of S. barbata combined with acupuncture is more significant.
Key words: rats; type 2 diabetes mellitus(T2DM); Sculellaria barbata; acupuncture; liver; spleen; lungs; organizational structure
Foundation items: National Natural Science Foundation of China (31402269);General Project of Education Department of Sichuan(17ZB0348)
0 引言
【研究意义】随着人们生活水平的不断提高,近年来宠物数量迅猛增长。糖尿病(Diabetes mellitus,DM)在动物中的发病率逐年升高,已成为家养动物最常见的疾病之一,尤其对宠物业的健康发展已造成严重威胁(刘金鹏等,2015;赵一等,2020);此外,采用传统的化学药物治疗DM存在多种毒副作用,包括心血管疾病风险增加、胃肠道不良反应及体重增加等(王涛和印晓星,2016)。中药不仅具备抗菌消炎和调控机体自身免疫等作用,还具有低毒、低残留、环保及不易产生耐药性等优点(郗玉玲等,2013;王蓉等,2019;曹冶等,2020;董書伟等,2021),尤其是联合针灸在DM治疗研究中已成为焦点(殷茵等,2016)。因此,进一步探究针药结合疗法对动物DM的治疗效果,可为促进宠物业的健康发展提供技术支持。【前人研究进展】DM是一种因血液胰岛素含量绝对或相对不足而引起以血糖过高为特征的内分泌代谢疾病(韦玲静等,2014),其中2型糖尿病(Diabetes mellitus type 2,T2DM)常伴有肝脏、脾脏和肺脏等多器官损伤(秦双红等,2020)。T2DM治疗的关键是通过降低血糖而改善胰岛素抵抗(阮凌,2020),而中药可通过降低血糖、改善胰岛素抵抗,进而有效治疗T2DM及其并发症。陈璇等(2015)研究表明,白虎二地汤可通过调节炎症因子而减轻炎症反应,并通过PI3K胰岛素信号转导途径改善胰岛素抵抗;姜楠楠等(2017)研究指出,黄地安消胶囊可通过IRS-1/PI3K信号通路调控IRS-1蛋白活性,显著增加肝脏对葡萄糖的摄取,提高肝糖原合成,从而达到改善胰岛素抵抗的作用;徐洁淼等(2018)研究发现,木丹颗粒对DM及并发症的疗效在于其可改善胰岛素抵抗及胰岛β细胞功能、抑制胰岛β细胞凋亡、减轻血管炎症反应和抗氧化应激等。临床上采用针灸治疗T2DM也能显著降低大鼠血清中胰岛素及胰岛素抵抗素的含量,从而达到理想的治疗效果(张思依,2017),其高频针灸穴位有脾俞、三阴交、足三里和肾俞(翁瑜君等,2016;于慧娟等,2018;高大红等,2019)。针药结合对T2DM有更好的疗效,能更有效地降低患者血糖、调节血脂异常及改善胰岛素抵抗(葛玲玲等,2019)。姚玉芳等(2004)对T2DM患者进行耳针结合三黄降糖汤治疗,结果发现针药结合起协同作用,其治疗总有效率为93.33%,较耳针组提高20.00%,较中药组则提高20.33%。杨洁和何威(2007)采用中药方剂(人参、黄芪和苍术等)结合针灸(足三里等)治疗68例T2DM(并发症胃轻瘫),其疗效明显优于降糖药/胰岛素+吗丁啉组。韩纬哲(2019)根据患者证型采用6个经方配合针灸(三阴交、足三里及肾俞等穴位)治疗T2DM患者290例,其有效率为97.58%,较临床常规用药组(口服格列齐特缓释片)提高15.48%。【本研究切入点】中药半枝莲是唇形科(Lamiaceae)植物半枝莲(Scutellaria barbata D. Don)的干燥全草,归肺、肝、肾经,具有清热解毒、化瘀利尿等功效(王翊豪等,2017),其提取物能显著抑制大鼠蔗糖负荷后的血糖上升,改善胰岛素抵抗及调控脂肪代谢(王涛等,2013),提示半枝莲可在T2DM防治中发挥重要作用,但至今尚无采用半枝莲联合针灸治疗T2DM的研究报道。【拟解决的关键问题】以链脲佐菌(Streptozocin,STZ)联合高糖高脂诱导构建大鼠T2DM模型(邵俊伟和蔡逊,2014),再采用灌服半枝莲醇提物与针灸相结合的方法进行治疗,通过HE染色观察肝脏、脾脏和肺脏的组织结构变化,同时以Masson染色观察肺脏结缔组织变化,旨在明确半枝莲醇提物联合针灸对T2DM的治疗效果,为动物T2DM提供有效的治疗手段,进而保障宠物业的健康发展。
1 材料与方法
1. 1 试验材料
选用60只4周龄的SPF级近交系Wistar雄性大鼠(体重200~220 g),合格证号SCXK(川)2015-030),购自成都达硕实验动物有限公司;经四川农业大学动物伦理委员会批准,按照《实验动物护理与使用指南》对所有大鼠进行处理。普通饲料购自成都达硕实验动物有限公司,高糖高脂饲料购自北京博爱港商贸有限公司;HE染液购自成都谷歌生物科技有限公司;Masson染液购自北京索莱宝生物科技有限公司;STZ购自Sigma公司;半枝莲粉末(生产批号160701)购自四川利民中药饮片有限公司。柠檬酸缓冲液:A液为2.10 g柠檬酸加入100 mL蒸馏水配制而成;B液为2.94 g柠檬酸钠加入100 mL蒸馏水配制而成;A液与B液1∶1混合,pH 4.2~4.5。5‰ STZ溶液:0.5 g STZ溶于100 mL柠檬酸缓冲液,现配现用。
1. 2 半枝莲醇提物制备
采用95%乙醇超声波提取半枝莲,提取率为3.8%,总酚含量约80 mg/g,具体制备步骤如下:精准称量10.00 g半枝莲粉末加入干燥的250 mL三角瓶中,加入100 mL 95%乙醇,室温超声波提取60 min,滤纸加纱布抽滤;按照相同方法重复提取1次,合并2次滤液,旋转蒸发至10 mL,置于冷冻干燥机至恒重,冷冻保存(况伟等,2015)。然后精密称取一定量的半枝莲醇提物,以生理盐水稀释,根据李中华等(2010)的方法制备成含生药量为0.25 g/mL的醇提物,4 ℃冷藏备用。
1. 3 试验动物分组及治疗
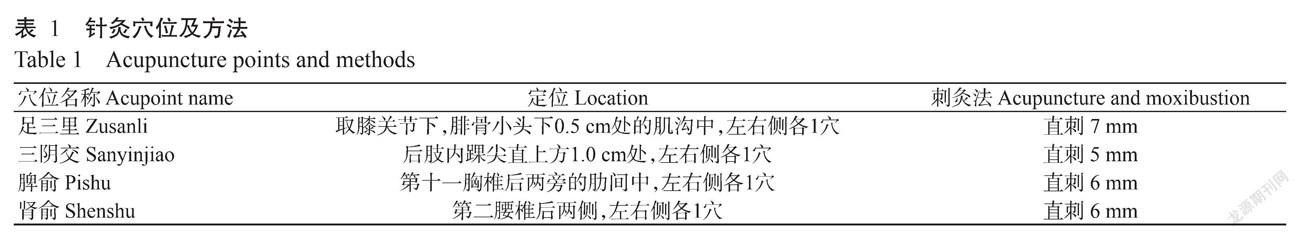
所有大鼠使用普通饲料适应性饲养1周后,按体重无差异原则随机分为健康对照组(H组,15只)和模型组(M组,45只)。H组饲喂普通饲料,M组饲喂高糖高脂饲料,连续饲喂30 d后禁食不禁水24 h。第32 d对全部大鼠进行称重,30 min内M组大鼠经腹腔注射5% STZ建模,注射剂量为45 mg/kg(Zhou and Zhou,2018);H组大鼠经腹腔注射柠檬酸缓冲液(4.5 mL/kg)。分别于第35和37 d,通过尾静脉采血测定大鼠空腹血糖(FBG),以FBG>7.8 mmol/L为成功建模标准(Zhou and Zhou,2018)。确定建模成功后,即第38 d将45只T2DM大鼠随机分为3个组,分别为模型对照组(M组,15只)、半枝莲治疗组(S组,15只)和半枝莲联合针灸治疗组(A组,15只)。从第39 d开始,每天在16:00时统一灌胃给药,H组和M组大鼠按1 mL/100 g的剂量灌服生理盐水,S组和A组大鼠则按1 mL/100 g的剂量灌服半枝莲醇提物(0.25 g/mL)。A组大鼠在每天9:00时针灸足三里和三阴交2个穴位,留针30 min;15:00时针灸脾俞和肾俞2個穴位,留针30 min;6 d为1个疗程,共计3个疗程,疗程间隔1 d,具体针灸穴位及方法见表1。试验过程中,H组大鼠饲喂普通饲料,其余各组饲喂高糖高脂饲料,自由饮水,定期清洁鼠笼,治疗周期共21 d。
1. 4 临床症状及生理生化指标观察
于试验第46、53和60 d(治疗第7、14和21 d)分别观察记录大鼠精神状态及体重变化;采集大鼠尾静脉血用于FBG测定。
1. 5 组织病理学观察
分别于治疗第7、14和21 d处死各处理组5只大鼠,剖解后肉眼观察大鼠肝脏、脾脏和肺脏的形态及颜色等;然后迅速采样置于4%多聚甲醛中固定24 h,制作石蜡切片并进行HE染色,同时取肺脏石蜡切片进行Masson染色;显微镜下观察各器官的组织结构变化;脾脏计数脾小结数量,肺脏测量肺间隔厚度。
1. 6 统计分析
试验数据采用SPSS 22.0进行统计分析,以单因素方差分析(One-way ANOVA)检测其差异显著性。
2 结果与分析
2. 1 治疗期间大鼠的临床症状及FBG变化规律
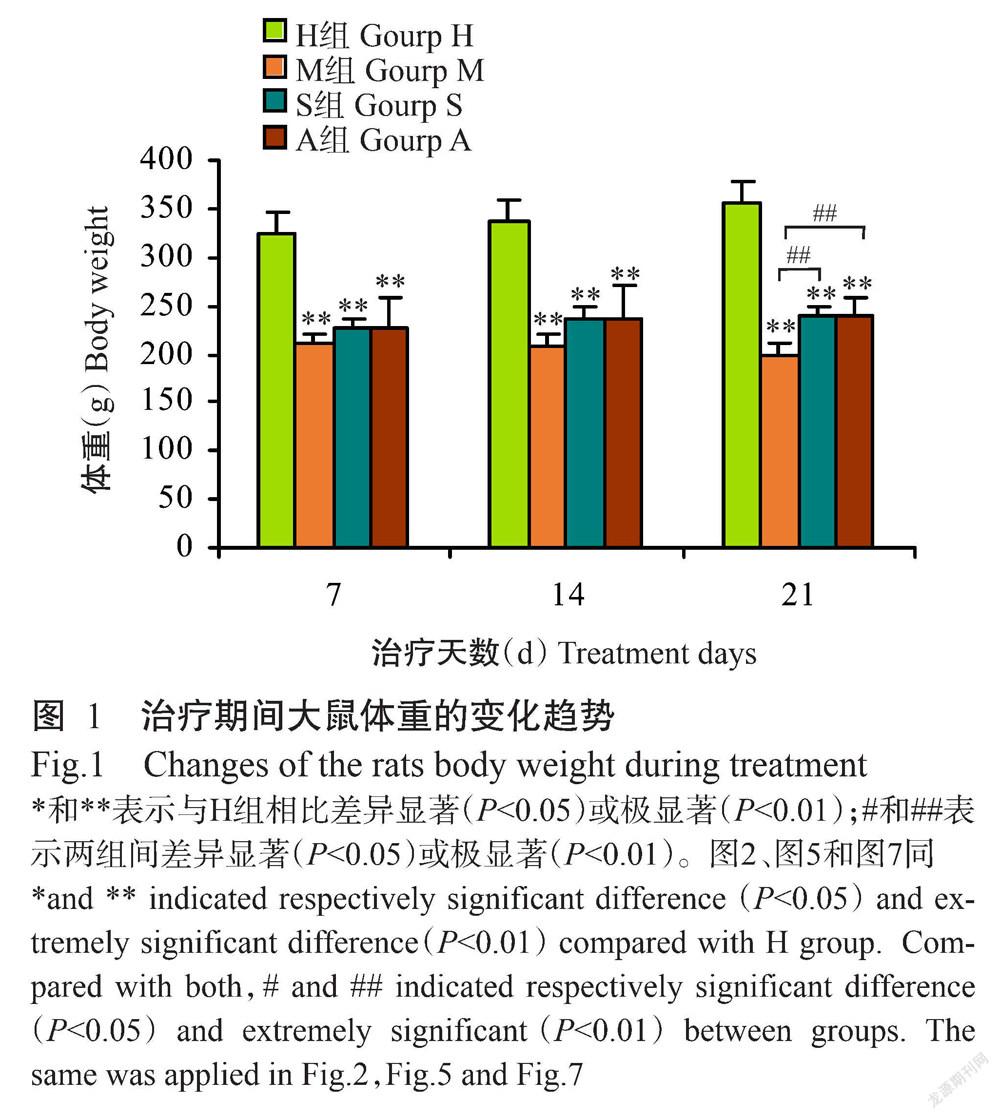
如图1所示,随着治疗时间的推移,H组大鼠的体重呈逐渐增长趋势,而M组大鼠的体重呈下降趋势。与H组相比,M组、A组和S组大鼠的体重均极显著下降(P<0.01,下同)。与M组相比,A组和S组大鼠的体重呈增长趋势,至治疗第21 d极显著升高。整个治疗期间,A组和S组大鼠的体重非常相近,差异不显著(P<0.05,下同)。
如图2所示,随着治疗时间的推移,M组大鼠的FBG呈逐渐升高趋势,而A组和S组大鼠的FBG呈下降趋势。与H组相比,M组大鼠的FBG极显著升高。与M组相比,治疗第7 d,S组大鼠的FBG略有升高,而A组大鼠的FBG显著降低(P<0.05,下同);至治疗第14和21 d,A组和S组大鼠的FBG均极显著降低。整个治疗期间,A组大鼠的FBG均低于S组大鼠。
2. 2 大鼠肝脏组织结构的变化
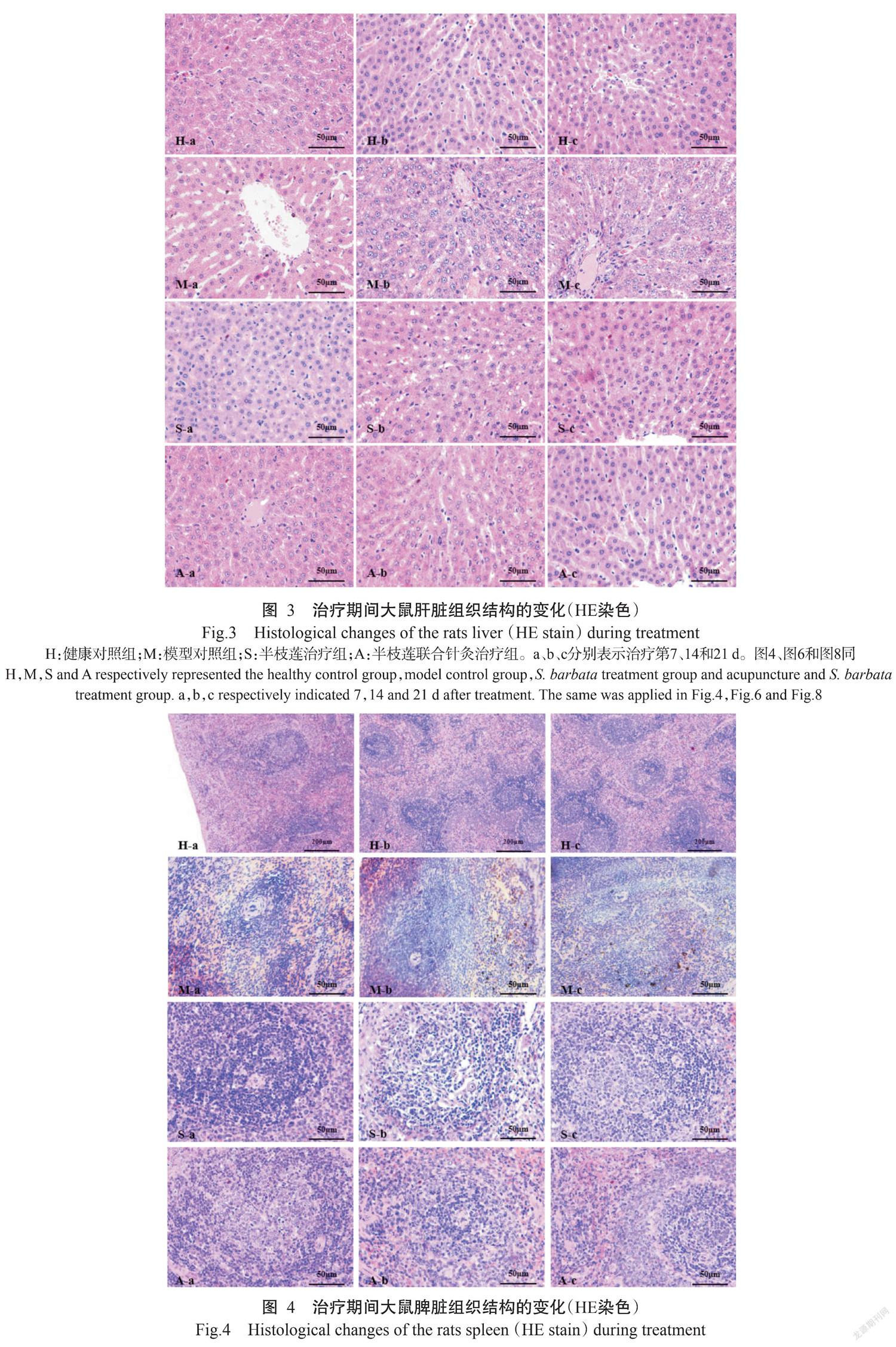
H组大鼠肝脏组织结构正常(图3:H-a、H-b和H-c)。整个治疗期间,M组大鼠的肝小叶结构由紊乱发展到坏死,肝索、肝窦结构模糊不清,肝细胞水肿逐渐加重;肝细胞由水肿发展到脂肪变性或局灶性坏死,炎症细胞浸润逐渐增强;治疗第14 d肝中央静脉可见出血,治疗第21 d可见中央静脉淤血(图3:M-a、M-b和M-c)。S组大鼠肝脏组织结构在治疗第7 d表现为肝小叶分界、结构混乱,肝细胞脂肪变性;至治疗第14和21 d肝小叶的病变情况逐渐得到改善,组织结构逐渐完整,肝索排列恢复整齐,肝窦结构清晰,脂肪变性及炎症细胞浸润减少(图3:S-a、S-b和S-c)。A组大鼠肝脏组织结构在治疗第14和21 d其肝小叶的肝细胞边界清晰,肝索逐渐清晰,炎症细胞浸润减少,其组织结构逐渐接近于H组;肝细胞水肿和脂肪变性均明显减少(图3:A-a、A-b和A-c)。可见,M组大鼠肝脏组织结构损伤加重,而A组和S组大鼠肝脏组织损伤得到缓解,尤其是A组逐渐接近于H组水平。
2. 3 大鼠脾脏组织结构的变化
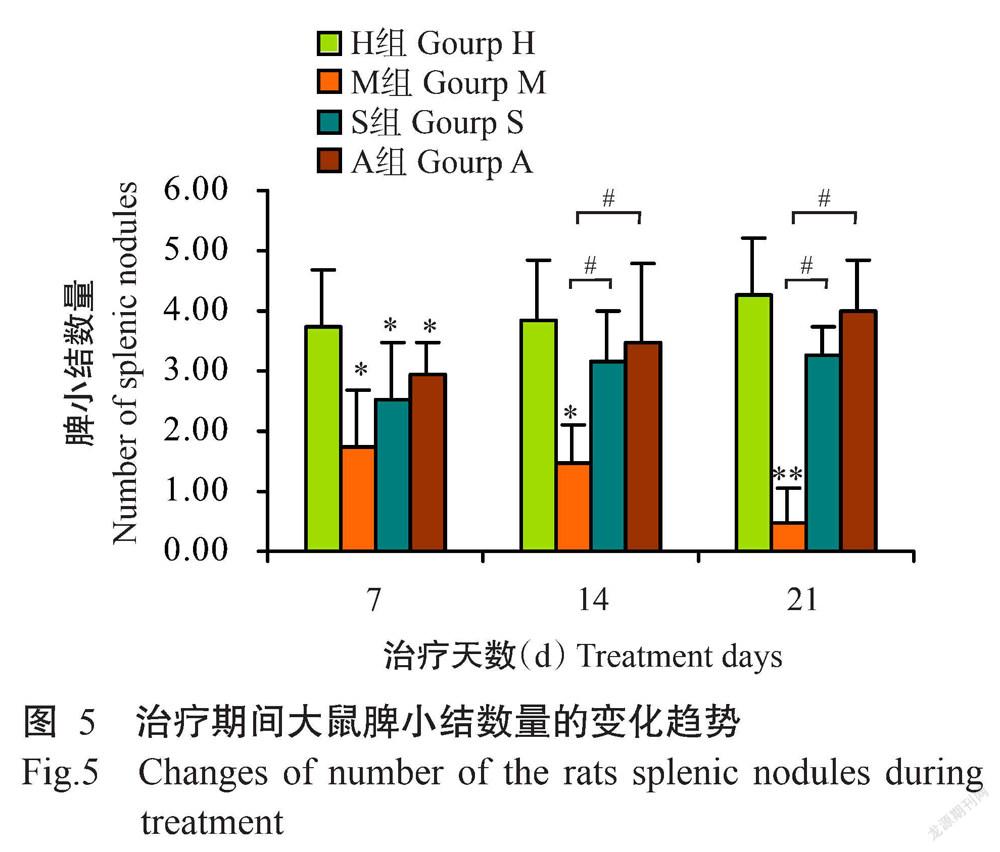
H组大鼠脾脏组织结构正常(图4:H-a、H-b和H-c)。整个治疗期间,M组大鼠脾脏被膜皱缩逐渐加重,红髓和白髓分界处结构逐渐混乱,生发中心不明显,边缘区变薄,动脉周围淋巴鞘变薄,淋巴细胞数量减少且排列由稀疏发展到紊乱;至治疗第14 d出现脾小梁断裂,治疗第21 d脾小梁动脉充血,脾脏局部可见细胞坏死(图4:M-a、M-b和M-c)。S组大鼠脾脏在治疗第14和21 d其被膜皱缩逐渐缓解,红髓和白髓结构清晰,可观察到明显的生发中心,动脉周围淋巴鞘较M组大鼠的稍厚,淋巴细胞排列较M组大鼠的紧密,边缘区逐渐增厚(图4:S-a、S-b和S-c)。A组大鼠脾脏被膜由轻微皱缩逐渐改善为平滑,以治疗第14和21 d最明显;红髓和白髓结构、生发中心均逐渐趋于正常,动脉周围淋巴鞘逐渐变厚,淋巴细胞排列较紧密,与H组大鼠相近(图4:H-a、H-b和H-c)。可见,M组大鼠脾脏组织结构损伤逐渐加重,而A组和S组大鼠脾脏组织损伤得到缓解,尤其是A组逐渐接近于H组水平。
随着治疗时间的推移,H组大鼠的脾小结数量呈缓慢增加趋势;M组大鼠的脾小结数量持续减少,几乎消失;A组和S组大鼠的脾小结数量逐渐增加,治疗结束后接近于H组水平。至治疗第7 d,H组大鼠的脾小结数量显著多于M组、A组和S组,且A组和S组多于M组,但差异不显著;至治疗第14 d,M组大鼠的脾小结数量显著少于H组、A组和S组;至治疗第21 d,M组大鼠的脾小结数量极显著少于H组、A组和S组,H组与A组和S组间无显著差异(图5)。
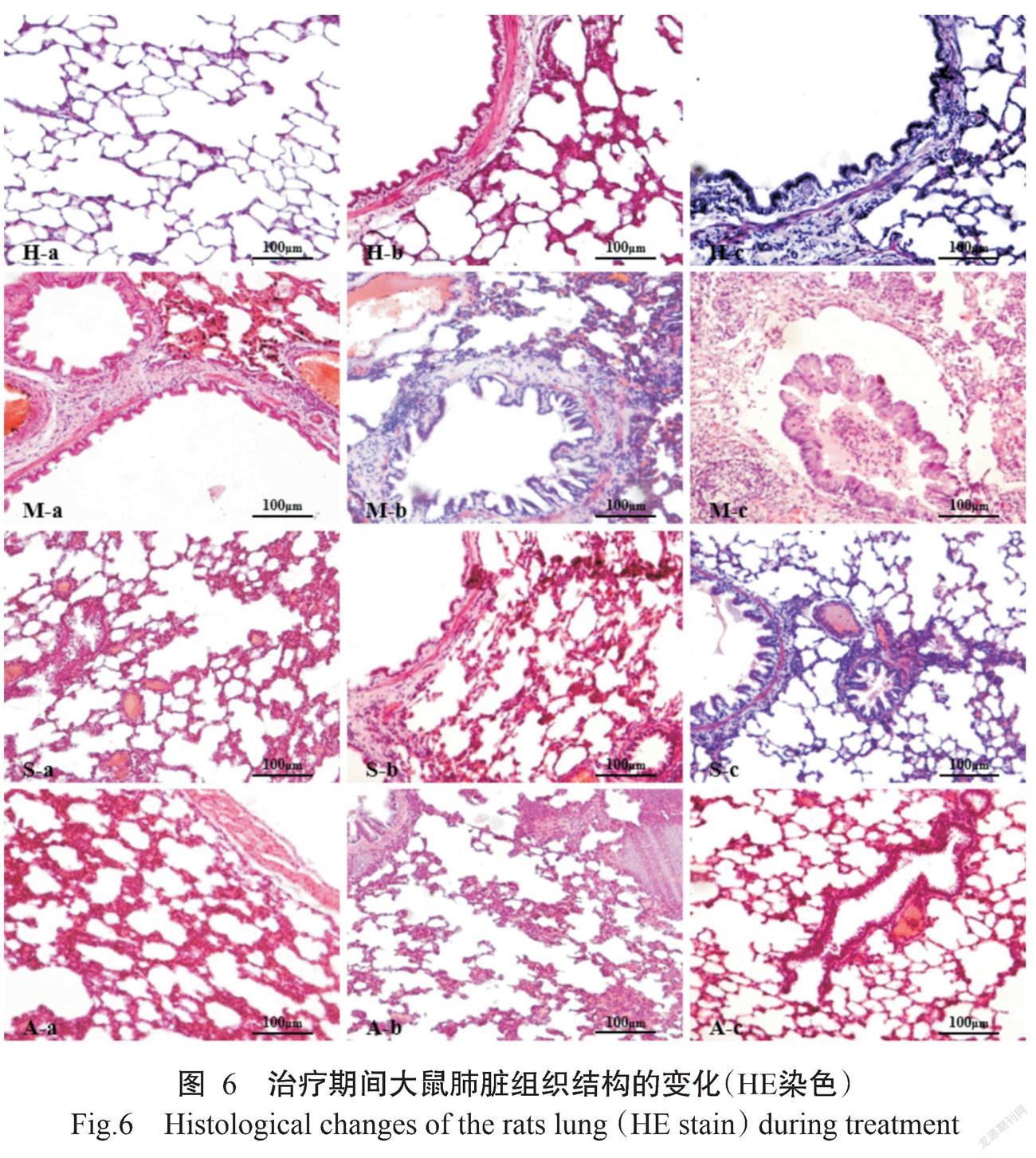
2. 4 大鼠肺脏组织结构的变化
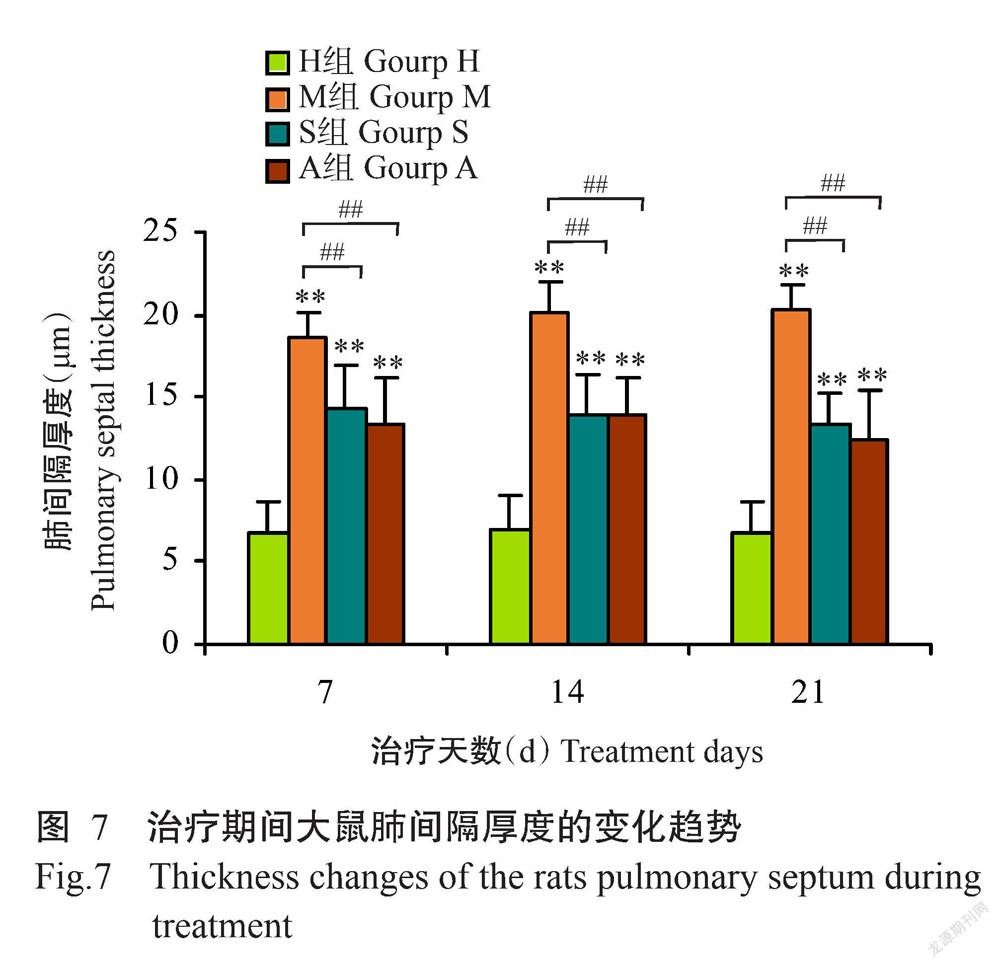
整个治疗期间,H组大鼠肺脏组织正常,肺泡结构完整清晰,肺泡壁薄(图6:H-a、H-b和H-c)。M组大鼠的肺泡内大量出血,肺泡隔厚度增加,肺泡面积减小,小支气管和细支气管黏膜下层胶原纤维大量增生,管壁显著增厚,肺间质可见明显的炎症细胞浸润;至治疗第21 d肺组织结构模糊(图6:M-a、M-b和M-c)。S组大鼠肺泡内的出血情况逐步得到改善,肺泡隔显著增厚,小支气管和细支气管粘膜下层胶原纤维增生逐渐减少,管壁增厚逐渐减少,肺间质内炎症细胞浸润减少(图6:S-a、S-b和S-c)。A组大鼠肺泡基本完整清晰,肺泡隔增厚减轻,肺泡内轻微出血,小支气管和细支气管粘膜下层胶原纤维增生减少,管壁增厚较S组薄,肺间质内有少量炎症细胞浸润,至治疗第14和21 d改善更明显(图6:A-a、A-b和A-c)。此外,对HE染色切片进行肺间隔厚度测量发现,治疗过程中H组大鼠肺间隔厚度无明显变化,M组大鼠肺间隔厚度呈上升趋势,而A组和S组大鼠肺间隔厚度呈下降趋势。其中,H组大鼠肺间隔厚度极显著低于M组、A组和S组,而M组又极显著高于治疗组A组和S组(图7)。可见,M组大鼠肺脏组织结构损伤逐渐加重,而A组和S组大鼠肺脏组织损伤得到缓解,尤其是A组接近于H组水平。
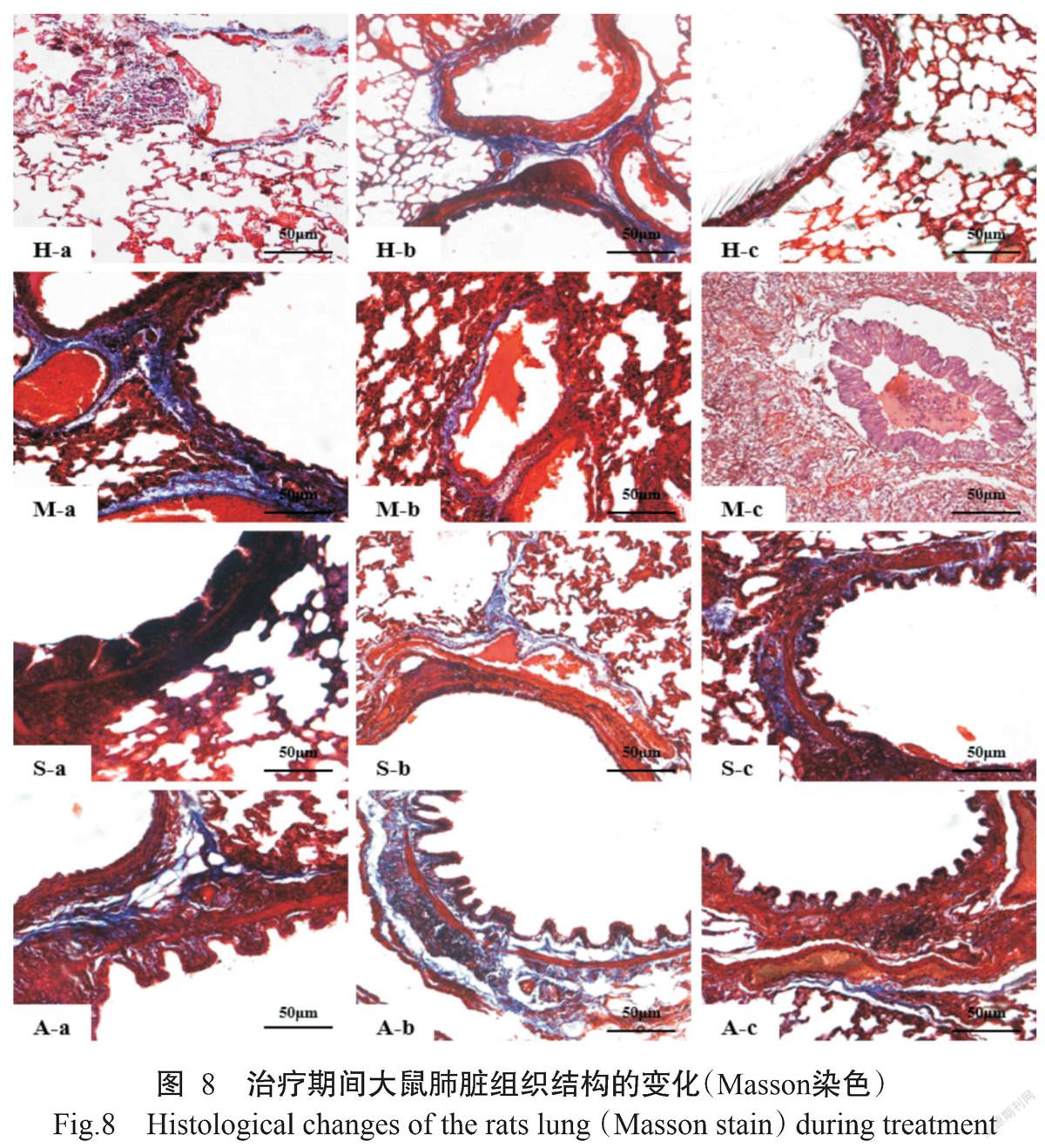
Masson染色结果显示:H组大鼠肺泡结构清晰完整(图8:H-a、H-b和H-c)。M组大鼠的肺泡内大量出血,支气管黏膜下层和血管壁可见胶原纤维大量增生,管壁显著增厚,整个治疗期间纤维化程度均呈增强趋势,最终导致部分肺泡萎陷或实变消失(图8:M-a、M-b和M-c)。至治疗第7 d,S组大鼠支气管黏膜下层胶原纤维增生,但随着治疗时间的推移,支气管黏膜下层胶原纤维增生逐渐减少(图8:S-a、S-b和S-c);A组大鼠肺泡结构基本完整清晰,肺泡内有轻微出血,随着治疗时间的推移,支气管黏膜下层胶原纤维增生逐渐减少(图8:A-a、A-b和A-c)。
3 讨论
3. 1 T2DM对肝脏、脾脏和肺脏组织结构的影响
本研究结果表明,M组大鼠体重显著减轻,肝脏病变明显,肝细胞由水肿发展到脂肪变性或局灶性坏死。究其原因可能是采用高糖高脂饲料饲喂大鼠后,大鼠体内摄入外源性脂肪增多,乳糜颗粒经小肠进入血液的含量增多,继而引起肝脏内脂类物质代谢障碍,肝脏转运中性脂肪的能力降低,中性脂肪沉积于肝脏内;同时大鼠摄入过多糖类后肝脏合成和贮存糖原的负荷增加,过多的糖类通过糖异生转化为脂肪酸蓄积于肝细胞內,而游离脂肪酸具有较强的细胞毒性,会引起肝细胞炎症细胞浸润、脂肪变性或坏死(宋爽等,2012),最终造成肝细胞脂蛋白合成障碍,机体脂肪代谢平衡失调,引起大鼠体重降低。
脾脏是动物体内最大的免疫器官,李静和刘德义(2010)通过腹腔注射STZ制备DM大鼠模型发现脾脏发生明显病变。在本研究中,M组大鼠脾脏的红髓、白髓分布紊乱,淋巴细胞数量减少,表明T2DM会引起脾脏组织结构损伤,局部细胞坏死,进而导致机体的细胞免疫和体液免疫受到抑制,引起机体免疫功能障碍,与李静和刘德义(2010)的研究结果相似。此外,Parker等(2015)研究发现健康大鼠发育期间脾脏内可见大量脾小结形成。本研究在治疗期间通过脾小结计数发现,H组大鼠的脾小结数量持续少量增加,M组大鼠的脾小结数量则持续减少,表明发生T2DM时大鼠脾脏的细胞免疫功能受到抑制。
在慢性炎症作用下,多种细胞因子分泌失调,持续引起炎症和胶原过度表达,造成肺脏长期处于损伤状态,大量成纤维细胞被持续激活,细胞外基质不断沉积,导致肺脏损伤修复从生理性愈合转变为病理性纤维化(Yamagishi et al.,2012)。肺脏在持续高血糖状态下,由于细胞外基质沉积和纤维化而受到损伤(Klein et al.,2010)。本研究结果表明,M组大鼠肺脏病变,尤其是纤维化程度也表现出随高糖高脂饲养时间延长而不断加重的现象。
3. 2 半枝莲联合针灸对T2DM大鼠肝脏、脾脏和肺脏组织结构的影响
半枝莲在降血脂、改善肝细胞脂肪变性和修复受损肝细胞等方面作用显著(罗艺萍,2010),还能增强免疫活性(王涛等,2013),尤其是半枝莲黄酮能显著降低DM小鼠血糖,提高脾脏指数,在体内具有明显的免疫增强作用,可通过提高免疫力而对DM起缓解作用。半枝莲能明显改善肺纤维化,抑制早期纤维化结节出现(徐昌君等,2016),且被广泛应用于肺脏和肝脏等器官的纤维化治疗。在本研究中,S组大鼠的肝脏、脾脏和肺脏组织结构病变得到明显改善,表明半枝莲治疗对T2DM大鼠肝脏、脾脏和肺脏组织结构损伤有明显的缓解作用。
由针灸治疗DM的临床文献可知,针灸治疗T2DM疗效显著,可有效减轻免疫功能损伤(朴耕希等,2010)。结合针灸理论(张海燕等,2012)分析发现,穴位针刺可能会改变药物作用的靶部位、脏器和机体的血药浓度,以及脏器和机体对药物的敏感性等,从而增强药物治疗效果。此外,赵微(2013)研究发现,针药联合治疗T2DM的疗效显著,显著高于单独用药的效果。本研究选取最常选用的三阴交、足三里、脾俞和肾俞,结果显示,A组和S组大鼠的肝脏、脾脏、肺脏组织结构变化相近,其损伤均得到明显改善;且A组更接近于H组水平,表明针药联合在一定程度上提高了单纯用药对T2DM的治疗效果,但效果差异不显著。究其原因可能是选取穴位过少或存在其他与T2DM关系更紧密的穴位,在穴位的选取及配合上有待改善;也可能是针药治疗过短导致效果不够明显,但具体原因还需进一步探究。
4 结论
STZ联合高脂高糖诱导T2DM大鼠模型稳定,能对大鼠肝脏、脾脏和肺脏造成损伤。半枝莲或半枝莲联合针灸治疗对T2DM大鼠肝脏、脾脏和肺脏组织结构均具有较好的改善效果,且以针灸配合半枝莲的效果更优。
参考文献:
曹冶,于吉峰,谢晶,张先惠,彭广能,钟志军,康润敏. 2020. 中药(赶黄草+波棱瓜子)提取物对小鼠维生素A急性中毒早期的治疗效果[J]. 南方农业学报,51(7):1737-1743. [Cao Y,Yu J F,Xie J,Zhang X H,Peng G N,Zhong Z J,Kang R M. 2020. Effects of Chinese herbal(Herpetospermum caudigerum+Penthorum chinense Pursh)extracts on early stage of acute vitamin A poisoning in mice[J]. Journal of Southern Agriculture,51(7):1737-1743.] doi:10.3969/j.issn.2095-1191.2020.07.029.
陈璇,徐凛峰,汪悦,周方圆,何晓瑾. 2015. 白虎二地汤改善2型糖尿病大鼠胰島素抵抗分子机制的研究[J]. 南京中医药大学学报,31(4):364-367. [Chen X,Xu L F,Wang Y,Zhou F Y,He X J. 2015. The molecular mechanism of baihu erdi decoction in the improvement of insulin resistance in type 2 diabetic rats[J]. Journal of Nanjing University of Traditional Chinese Medicine,31(4):364-367.] doi:10.14148/j.issn.1672-0482.2015.0364.
董书伟,樊灵芝,李磊,王海峰,朱海鲸,翟军军,屈雷,王胜义. 2021. 黄白双花口服液治疗犊牛腹泻的系统药理学分析[J]. 南方农业学报,52(1):1-10. [Dong S W,Fan L Z,Li L,Wang H F,Zhu H J,Zhai J J,Qu L,Wang S Y. 2021. A systematic pharmacological analysis of Huangbaishuanghua oral liquid for treating calf diarrhea[J]. Journal of Southern Agriculture,52(1):1-10.] doi:10.3969/j.issn.2095-1191.2021.01.001.
高大红,袁爱红,张庆萍,王友刚,黄海燕. 2019. 针刺对2型糖尿病大鼠下丘脑GLUT3基因和蛋白的影响[J]. 时珍国医国药,30(3):733-736. [Gao D H,Yuan A H,Zhang Q P,Wang Y G,Huang H Y. 2019. Effect of acupuncture on GLUT3 gene and protein in hypothalamus of type 2 diabetic rats[J]. Lishizhen Medicine and Materia Medica Research,30(3):733-736.] doi:10.3969/j.issn.1008-0805. 2019.03.079.
葛玲玲,蔡德锋,邢建平,张金媛. 2019. 针药并用对早期2型糖尿病患者胰岛素抵抗指数的影响[J]. 上海针灸杂志,38(9):992-996. [Ge L L,Cai D F,Xing J P,Zhang J Y. 2019. Effect of acupuncture plus medication on insulin resistance index in early-stage type 2 diabetes patients[J]. Shanghai Journal of Acupuncture and Moxibustion,38(9):992-996.] dio:10.13460/j.issn.1005-0957.2019.09.0992.
韩维哲. 2019 六经辨治结合中医适宜技术对社区2型糖尿病干预的临床研究[D]. 济南:山东中医药大学. [Han W Z. 2019. Clinical study on intervention of six meridian differentiation and treatment combined with appropriate technology of traditional Chinese medicine on community type 2 diabetes mellitus[D]. Jinan:Shandong University of Traditional Chinese Medicine.] doi:10.27282/d.cnki.gsdzu.2019.000111.
姜楠楠,郭明飞,高家荣,方朝晖,姜辉,魏良兵,单莉,韩利平. 2017. 黄地安消胶囊改善自发性T2DM大鼠胰岛素抵抗机制研究[J]. 中药药理与临床,33(6):109-114. [Jiang N N,Guo M F,Gao J R,Fang Z H,Jiang H,Wei L B,Shan L,Han L P. 2017. Mechanism of Huangdi Anxiao capsules improving insulin resistance in sponta-neous T2DM rats[J]. Pharmacology and Clinics of Chinese Materia Medica,33(6):109-114.]
况伟,刘志伟,张晨,桂小琪. 2015. 半枝莲抗氧化活性成分的提取[J]. 中国食品添加剂,(9):36-41. [Kuang W,Liu Z W,Zhang C,Gui X Q. 2015. Extraction of active antioxidant components from Scutellaria barbata[J]. China Food Additive,(9):36-41.] doi:10.3969/j.issn.1006-2513.2015.09.004.
李静,刘德义. 2010. 丹参对链脲佐菌素糖尿病大鼠脾、肾组织结构的影响[J]. 畜牧兽医学报,41(11):1467-1471. [Li J,Liu D Y. 2010. Effect of Danshen root on morphologic change of spleen and kidney in diabetic rats induced by STZ[J]. Acta Veterinaria et Zootechnica Sinica,41(11):1467-1471.]
李中华,赵晓芳,李圭,余胜明. 2010. 半枝莲水煎液對免疫性肝纤维化大鼠TGF-β1及TIMP-1表达的影响[J]. 时珍国医国药,21(11):2820-2821. [Li Z H,Zhao X F,Li G,Yu S M. 2010. Effect of Scutellaria barbata decoction on TGF-β1 and TIMP-1 in rats with immune liver fibrosis[J]. Lishizhen Medicine and Materia Medica,21(11):2820-2821.] doi:10.3969/j.issn.1008-0805.2010.11.045.
刘金鹏,何绍纯,刘燕,夏茂华,阎京. 2015. 黑冠猕猴糖尿病诊治及病因分析[J]. 现代农业科技,(9):286-287. [Liu J P,He S C,Liu Y,Xia M H,Yan J. 2015. Diagnosis treatment and etiological analysis of diabetes in black crowned macaque[J]. Modern Agricultural Science and Technology,(9):286-287.]
罗艺萍. 2010. 黄酮类化合物的药理活性研究进展[J]. 亚太传统医药,6(4):126-128. [Luo Y P. 2010. Advances in pharmacological research of flavonoids[J]. Asia-Pacific Traditional Medicine,6(4):126-128.]
朴耕希,刘艳艳,徐玉东,王宇,尹磊淼,杨永清. 2010. 针灸治疗2型糖尿病临床研究进展[J]. 江西中医学院学报,22(1):72-75. [Pu G X,Liu Y Y,Xu Y D,Wang Y,Yin L M,Yang Y Q. 2010. Progress of clinical study of Ⅱ diabe-tic in acupuncture and moxibustion[J]. Journal of Jiangxi University of Traditional Chinese Medicine,22(1):72-75.] doi:10.3969/j.issn.1005-9431.2010.01.022.
秦双红,余臣祖,康学东,李芳芳 2020. 基于“肝藏血、主疏泄”的生理功能探讨糖尿病的发病机制[J]. 中国中医基础医学杂志,26(6):729-730. [Qin S H,Yu C Z,Kang X D,Li F F. 2020. Study on the pathogenesis of diabetes mellitus based on the physiological function of liver sto-ring blood and regulating discharge[J]. Chinese Journal of Basic Medicine in Traditional Chinese Medicine,26(6):729-730.] doi:10.3969/j.issn.1006-3250.2020.06.008.
阮凌. 2020. 魔芋多聚糖对改善2型糖尿病大鼠糖脂代谢异常的机制研究[J]. 江西农业学报,32(6):88-92. [Ruan L. 2020. Mechanism of konjac glucomannan in improving abnormal glycolipid metabolism of type 2 diabetes rats[J]. Acta Agriculturae Jiangxi,32(6):88-92.] doi:10.19386/j.cnki.jxnyxb.2020.06.16.
邵俊伟,蔡逊. 2014. 高脂饮食联合链脲佐菌素建立2型糖尿病大鼠模型的研究进展[J]. 中国实验动物学报,22(4):90-93. [Shao J W,Cai X. 2014. Research progress of rat models of type 2 diabetes induced by high calorie diet combined with streptozotocin[J]. Acta Laboratorium Animalis Scientia Sinica,22(4):90-93.] doi:10.3969/j.issn. 1005-4847.2014.04.020.
宋爽,徐慧兰,肖水源,李桂源. 2012. 糖尿病家族史、饮食及肥胖与糖尿病交互作用[J]. 中国公共卫生,28(2):159-160. [Song S,Xu H L,Xiao S Y,Li G Y. 2012. Interactive effcets of family history of diabetes,diet and obesity on type 2 diabetes mellitus[J]. Chinese Journal of Public Health,28(2):159-160.]
王蓉,冯秀永,林佳. 2019. 中药结合针灸对周围性面瘫分期治疗的临床研究[J]. 内蒙古中医药,38(2):67-68. [Wang R,Feng X Y,Lin J. 2019. Clinical study on staged treatment of peripheral facial paralysis with traditional Chinese medicine combined with acupuncture[J]. Inner Mongolia Journal of Traditional Chinese Medicine,38(2):67-68.] doi:10.3969/j.issn.1006-0979.2019.02.046.
王涛,刘雪枫,张祎,何枢衡,安雅婷. 2013. 半枝莲改善糖脂代谢异常作用机制及药效物质基础研究[J]. 天津中医药,30(7):387. [Wang T,Liu X F,Zhang Y,He S H,An Y T. 2013. Mechanism of Scutellaria barbata improving abnormal glucose and lipid metabolism and its pharmacodynamic material basis[J]. Tianjin Journal of Traditional Chinese Medicine,30(7):387.] doi:10.11656/j.issn.1672-1519.2013.07.02.
王涛,印晓星. 2016. 2型糖尿病治疗药物研究进展[J]. 药学进展,40(5):323-330. [Wang T,Yin X X. 2016. Advances in therapeutics of type 2 diabetes mellitus[J]. Progress in Pharmaceutical Sciences,40(5):323-330.]
王翊豪,许晓义,杨斯琪,宋高臣. 2017. 半枝莲药理作用及化学成分提取的研究进展[J]. 牡丹江医学院学报,38(6):116-118. [Wang Y H,Xu X Y,Yang S Q,Song G C. 2017. Research progress on pharmacological action and extraction of chemical constituents from Scutellaria chinensis[J]. Journal of Mudanjiang Medical University,38(6):116-118.] doi:10.13799/j.cnki.mdjyxyxb.2017.06. 040.
韦玲静,黄玥萌,严雪瑜,蒋钦杨,兰干球,郭亚芬. 2014. 大鼠胰岛素Ⅱ基因启动子克隆与功能验证[J]. 南方农业学报,45(10):1861-1865. [Wei L J,Huang Y M,Yan X Y,Jiang Q Y,Lan G Q,Guo Y F. 2014. Cloning and functional verification of rat insulin II gene promoter[J]. Journal of Southern Agriculture,45(10):1861-1865.] doi:10. 3969/j:issn.2095-1191.2014.10.1861.
翁瑜君,唐梁,何海明. 2016. 靳三针疗法干预对T2DM大鼠模型胰岛素抵抗的影响[J]. 广西中医药,39(5):69-71. [Weng Y J,Tang L,He H M. 2016. Effect of Jin Sanzhen therapy on insulin resistance in T2DM rat model[J]. Guangxi Journal of Traditional Chinese Medicine,39(5):69-71.]
郗玉玲,赵英政,陈明,李大通,李鹏. 2013. 糖尿病小鼠免疫指数、胰腺线粒体自由基的变化及半枝莲黄酮的干预作用[J]. 实用临床医药杂志,17(23):1-4. [Xi Y L,Zhao Y Z,Chen M,Li D T,Li P. 2013. Changes of immune index and free radical of pancreas mitochondrion in diabetic mice and interventional function of flavonoids extracted from scutellaria barbata[J]. Journal of Clinical Medicine in Practice,17(23):1-4.] doi:10.7619/jcmp.201323001.
徐昌君,方松文,李宏彬,但勇,張川,徐林林,刘杨,张莉莉,杨长福. 2016. 黄芪提取物对肺纤维化小鼠肺泡炎症影响及抗纤维化作用研究[J]. 世界科学技术—中医药现代化,18(4):646-652. [Xu C J,Fang S W,Li H B,Dan Y,Zhang C,Xu L L,Liu Y,Zhang L L,Yang C F. 2016. Impacts of astragalus extract on the alveolar inflammation and anti-fibrosis effects in pulmonary fibrosis mice[J]. World Science and Technology-Modernization of Traditional Chinese Medicine,18(4):646-652.] dio:10.11842/ wst.2016.04.015.
徐洁淼,王镁,于世家. 2018. 木丹颗粒(糖末宁)治疗糖尿病及多种并发症的实验和临床研究证据[J]. 中华中医药学刊,36(2):384-387. [Xu J M,Wang M,Yu S J. 2018. Experimental and clinical evidence of Mudan granule (Tangmoning) in treatment of diabetes mellitus and various complications[J]. Chinese Archives of Traditional Chinese Medicine,36(2):384-387.] doi:10.13193/j.issn.1673-7717.2018.02.034.
杨洁,何威. 2007. 针药并用治疗2型糖尿病胃轻瘫68例[J]. 光明中医,22(12):41-43. [Yang J,He W. 2007. 68 cases of type 2 diabetic gastroparesis treated by acupuncture combined with medicine[J]. Guangming Journal of Chinese Medicine,22(12):41-43.] doi:10.3969/j.issn.1003-8914. 2007.12.024.
姚玉芳,王茎,黄学勇,周传云,吴成长,曾永蕾. 2004. 耳针对2型糖尿病患者糖代谢的影响[J]. 安徽中医学院学报,23(1):28-30. [Yao Y F,Wang J,Huang X Y,Zhou C Y,Wu C Z,Zeng Y L. 2004. Effect of auriculo-acupuncture on glucose metabolism in patients with type 2 diabetes[J]. Journal of Anhui Traditional Chinese Medical College,23(1):28-30.] doi:10.3969/j.issn.1000-2219.2004.01.012.
殷茵,刘志诚,徐斌. 2016. 针灸治疗2型糖尿病的临床研究进展[J]. 世界中医药,11(11):2480-2482. [Yin Y,Liu Z C,Xu B. 2016. Clinical research progress of type 2 diabetes treatment by acupuncture and moxibustion[J]. World Chinese Medicine,11(11):2480-2482.] doi:10.3969/j.issn. 1673-7202.2016.11.071.
于慧娟,臧晓明,张昕. 2018. 针灸治疗2型糖尿病选穴规律现代文献研究[J]. 山东中医药大学学报,42(1):37-40. [Yu H J,Zang X M,Zhang X. 2018. Analysis on rules of selecting acupoints in treating type 2 diabetes mellitus with acupuncture and moxibustion based on modern lite-ratures[J]. Journal of Shandong University of Traditional Chinese Medicine,42(1):37-40.] doi:10.16294/j.cnki. 1007-659x.2018.01.012.
张海燕,邬伟魁,李芳,万亮琴,宋伟,芦乾,贺娅,杨明. 2012. 针药结合治疗糖尿病及其并发症研究进展[J]. 中国实验方剂学杂志,18(4):260-264. [Zhang H Y,Wu W K,Li F,Wan L Q,Song W,Lu Q,He Y,Yang M. 2012. Therapy of acupuncture combined with medicine for treatmentof diabetes and its complications[J]. Chinese Journal of Experimental Traditional Medical Formulae,18(4):260-264.] doi:10.3969/j.issn.1005-9903.2012.04.072.
张思依. 2017. 针刺治疗高脂饮食诱导的肥胖C57BL/6小鼠胰岛素抵抗的效应机制研究[D]. 武汉:湖北中医药大学. [Zhang S Y. 2017. Influence of acupuncture on insulin resistance in C57BL/6 mice on a chronic high-fat diet[D]. Wuhan:Hubei University of Traditional Chinese Medicine.]
赵微. 2013. 针药联合治疗2型糖尿病19例临床观察[J]. 针灸临床杂志,29(7):27-28. [Zhao W. 2013. Clinical efficacy observation on primary trigeminal neuralgia with acupuncture:19 cases[J]. Journal of Clinical Acupuncture and Moxibustion,29(7):27-28.] doi:10.3969/j.issn.1005-0779.2013.07.013.
赵一,吴江,康恺,栗烨,李光辉,刘斌,郎贯存,安立龙,效梅. 2020. Activin A诱导大鼠胰腺导管干细胞分化形成胰岛β细胞[J]. 南方农业学报,51(1):209-216. [Zhao Y,Wu J,Kang K,Li Y,Li G H,Liu B,Lang G C,An L L,Xiao M. 2020. Activin A induced rat pancreatic ductal stem cells in vitro differentiation into pancreatic islets β cells[J]. Journal of Southern Agriculture,51(1):209-216.] doi:10.3969/j.issn.2095-1191.2020.01.027.
Klein O L,Krishnan J A,Glick S,Smith L J. 2010. Systematic review of the association between lung function and type 2 diabetes mellitus[J]. Diabetic Medicine,27(9):977-987. doi:10.1111/j.1464-5491.2010.03073.x.
Parker G A,Picut C A,Swanson C,Toot J D. 2015. Histolo-gic features of postnatal development of immune system organs in the sprague-dawley rat[J]. Toxicologic Pathology,43(6):794. doi:10.1177/0192623315578720.
Yamagishi S I,Maeda S,Matsui T,Ueda S,Fukami K,Okuda S. 2012. Role of advanced glycation end products(AGEs) and oxidative stress in vascular complications in diabetes[J]. Biochim Biophys Acta,1820(5):663-671. doi:10. 1016/j.bbagen.2011.03.014.
Zhou Y,Zhou J. 2018. Tranilast treatment attenuates cerebral ischemia-reperfusion injury in rats through the inhibition of inflammatory responses mediated by NF-κB and PPARs[J]. Clinical and Translational Science,12(2):196-202. doi:10.1111/cts.12606.
(責任编辑 兰宗宝)
