Efficacy of intravitreal conbercept combined with panretinal photocoagulation for severe nonproliferative diabetic retinopathy without macular edema
2022-04-19NingZhaoJianGuanNaCaiNingNingLiu
Ning Zhao, Jian Guan, Na Cai, Ning-Ning Liu
Department of Ophthalmology, the First Affiliated Hospital of China Medical University, Shenyang 110001, Liaoning Province, China
Abstract
● KEYWORDS: conbercopt; panretinal photocoagulation;severe nonproliferative diabetic retinopathy
INTRODUCTION
D iabetic retinopathy is one of cause of blindness in the developed world. Preventing the recurrence and improving the prognosis of diabetic retinopathy has been the focus of research. Panretinal photocoagulation (PRP) has been the primary treatment for diabetic retinopathy. A study on the early treatment of diabetic retinopathy (ETDRS) recommended that timely PRP should be performed in patients with severe nonproliferative proliferative diabetic retinopathy (SNPDR)[1-2].However, treatment with PRP has limitations[3].
Vascular endothelial growth factor (VEGF) plays a significant role in the neovascularization (NV) of proliferative diabetic retinopathy (PDR). Recently, anti-VEGF agents are widely used for treating PDR with satisfactory results[4-5]. Many authors have confirmed that PRP in combination with anti-VEGF agents is superior to PRP alone in protecting the visual field, reducing vitreous hemorrhage (VH), macular edema (ME), and NV regression in patients with PDR and angiogenesis[6-7].
Conbercept (KH902; Chengdu Kanghong Biotechnology Co.,Ltd., Sichuan Province, China) is a humanized recombinant fusion protein independently developed in China that involves a VEGF binding domain of human VEGFR-1, VEGFR-2, and FC part of human immunoglobulin G1. Conbercept has a larger molecule than ranibizumab and contains the fourth binding domain of VEGFR-2. It can penetrate all retinal levels with greater binding affinity, contributing to longer clearance time[8].Recently, conbercept has been studied and used in treating diabetic ME[9], wet age-related macular degeneration[10],chronic central serous chorioretinopathy[11-12], and PDR[13-14].However, reports on the treatment of SNPDR are rare.In this study, the efficacy and safety profiles of PRP alone were evaluated with intravitreal conbercept (IVC) injection plus PRP in patients with SNPDR without ME.
SUBJECTS AND METHODS
Ethical ApprovalThe protocols applied were certified by the Ethics Committee of the First Affiliated Hospital of China Medical University, and in compliance with the guidelines of the Helsinki Declaration. All patients signed a written informed consent following a description of the benefits and risks before treatment. All individuals involved in the study received informed consent.
Study DesignThis clinical research was a retrospective,comparative, and non-randomized. A total of 56 eyes were investigated from 48 patients with SNPDR and without ME who received PRP with or without conbercept pretreatment between January 2017 and December 2019. They were followed up for at least 6mo and divided into the PRP group and pulse group in the light of whether single-dose IVC was given 1wk before PRP. In the PRP group and pulse group,from January 2019 to December 2019, 23 patients (27 eyes)and 25 patients (29 eyes) are received PRP, respectively.
ParticipantsComprehensive ophthalmic examinations,including the best-corrected visual acuity (BCVA), intraocular pressure (IOP), B-ultrasound, dilated fundus examination with slit lamp biomicroscope, 90 D non-contact slit lamp lens,color fundus photographs, spectral domain optical coherence tomography (SD-OCT; Topcon Inc., Tokyo, Japan) and fundus fluorescein angiography (FFA; TRC.50DC, Topcon, Japan)were performed in all subjects. Data were collected at baseline and 1, 3, and 6mo after treatment (named as month 1, 3, and 6,respectively).
Criteria for inclusion into the study were the following: 1)type 2 diabetes in terms of the American Diabetes Association(ADA) or World Health Organization guidelines, age ≥18y,the glycosylated hemoglobin A1c (HbA1c) ≤10%, and blood pressure <160/90 mm Hg; 2) SNPDR absence of ME was confirmed by color fundus photographs, FFA, and OCT according to the classification criteria by ADA[15-16],central foveal thickness (CFT) was measured as the mean central macular region thickness based on the patient's fovea with a diameter of 1 mm; 3) no retinal photocoagulation or intravitreal injection of anti-VEGF was conducted before this study. Exclusion criteria were the following: 1) ME was considered when CFT was above 210 μm[15]; 2) severe keratopathy, glaucoma, lens opacity that may affect imaging,uveitis, optic neuritis, and a history of other ophthalmic disorders or intraocular surgery; 3) severe-allergic constitution,severe cardiac, hepatic, renal dysfunction, or other systemic diseases; 4) follow-up time was less than 6mo.
Treatment Protocols A posterior segment ophthalmic surgeon(Zhao N) was responsible for both injections and PRP. After local anesthesia, patients in the PRP group underwent a scatter laser treatment using a 532-nm argon green laser (Vision one,Lumenis Inc., CA, USA) for 4 sessions in one month time with one-week intervals. For each session, photocoagulation was performed in the order of the nasal, inferior, superior,and temporal sides with 200-300 μm spot sizes and a pulse duration of 0.2s. To achieve full PRP, 300-400 spots were created for a total of 1200-1600 burns. The power of the laser was individually adjusted and ranged between 100 and 200 mW to produce yellowish-white coagulative spots. One week after IVC, patients in the pulse group underwent PRP. A topical antibiotic was instilled for 3d before treatment. Using a 29-G needle, 0.05 mL of conbercept was injected into the vitreous through the inferotemporal pars plana and 3.5-4.0 mm behind the limbus. The eye ointment, antibiotic eye drops with tobramycin and dexamethasone were used for three days. IOP was reviewed regularly.
Study AssessmentThe difference of BCVA and CFT between the two groups was the primary outcome indicator. Secondary outcome indicators were the comparisons of visual acuity(VA) improvement, rates of treatment effectiveness, and postoperative complications.
Criteria for treatment effectiveness: at the end of follow-up, BCVA improvement ≥2 lines or decline ≥2 lines were considered a visual improvement or visual reduction; otherwise, BCVA was considered visual stability. Treatment was effective if BCVA was increased or remained unchanged.
Statistical AnalysisContinuous variables were presented as means with standard deviations (SDs). Categorical variables were presented as counts and proportions. Data were evaluated using one-way analysis of variance or Chi-square test using SPSS Version 22 (IBM Corp., Armonk, NY, US). SignificantPvalues were less than 0.05.
RESULTS
Basic CharacteristicsAs shown in Table 1, 56 eyes were contained in this study out of 48 patients with SNPDR and without ME. Data were presented as mean±SD. Ages were 50.37±5.50 and 49.41±5.60y for the PRP group and pulse group, respectively. There was no statistical difference between the groups in gender (P=0.785), age (P=0.522), duration of diabetes (P=0.172), preoperative BCVA (P=0.746), CFT(P=0.115), and IOP (P=0.116).
Main Results
Best-corrected visual acuityFor the PRP group, BCVA (log MAR) was 0.14±0.10 before PRP, which was deteriorated to 0.42±0.12 (P<0.001) at 1mo and to 0.28±0.11 at 3mo(P<0.001) before steadily improving to 0.18±0.15 at 6mo(P>0.05). In the pulse group, BCVA was 0.15±0.10 at baseline before PRP, which was continuously decreased at 0.25±0.11 at 1mo (P<0.001), increased subsequently to 0.18±0.09 (P<0.05)at the 3mo before improving to 0.09±0.08 at 6mo (P<0.001).In the period of follow-up, the BCVA in the pulse group was better than that in the PRP group, especially at 1 and 3mo(0.42±0.12vs0.25±0.11,P<0.001; 0.28±0.11vs0.18±0.09,P<0.001; and 0.18±0.15vs0.09±0.08,P=0.008, respectively;Table 2).
Center foveal thicknessThe baseline CFT was 188.74±4.38 in the PRP group and 187.07±3.40 μm in the pulse group(P=0.115). In the PRP group, the thickness of CFT after PRP peaked at 277.30±13.74 μm at 1mo, then decreased from 223.59±8.35 to 210.00±8.51 μm between 3 and 6mo(P<0.001). In the pulse group, the CFT briefly increased to 221.17±6.40 μm at 1mo, which was significant compared to the baseline (P<0.001), then steadily decreased to 185.14±4.61 at 3mo and to 187.07±3.29 μm at 6mo. The changes at 3 and 6mo from the baseline were not statistically significant(P>0.05,P=0.073,P=0.077, respectively), suggesting that CFT returned to its initial foveal thickness. During the followup, the mean CFT of the pulse group was significantly lower than that of the PRP group (277.30±13.74vs221.17±6.40,t=19.412; 223.59±8.35vs185.14±4.61,t=20.815; 210.00±8.51vs187.07±3.29 μm,t=13.471, allP<0.001; Table 3).
The Secondary Outcome
Visual acuity improvement and rates of treatmenteffectivenessVA improvement following treatment is presented in Table 4. In the PRP group, VA was increased in 3 patients (11.11%), decreased in 5 patients (18.52%), unchanged in 19 patients (70.37%) at 6mo. In the pulse group, VA was improved in 13 patients (44.83%), unchanged in 16 out of 29 eyes (55.17%) with no patients having decreased VA. The rate of effectiveness in VA in the pulse group was higher than that in the PRP group (81.48%vs100%,χ2=7.09,P<0.05).
Postoperative complications and adverse eventsThroughout the period of follow-up, no evident eye complications, or systemic adverse reactions (e.g., uveitis reaction, rapid aggravation of cataract, neovascular glaucoma, endophthalmitis, and retinal detachment) were identified. In the pulse group, 2 cases (6.9%)of subconjunctival hemorrhage and one case of transiently increased IOP were reported, the cases were mild and the patients recovered without treatment. At 6mo follow-up, mild recurrent VH with visible fundus information occurred in 5 eyes (18.52%) in the PRP group; it was difficult to assess the retina nerve fiber layer or small vessels[17]. Patients were instructed to monitor the patient's blood glucose, blood pressure and other systemic conditions and take Chinese medicine orally (hexuemingmu). The VH was completely absorbed after 2wk.

Table 1 The comparison of basic characteristics between PRP and pulse group mean±SD

Table 2 BCVA between the two groups before and after treatment mean±SD
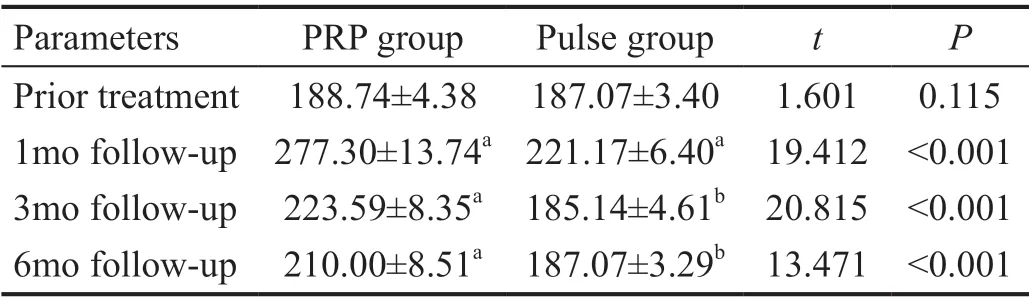
Table 3 CFT between the two groups before and after treatment mean±SD, μm

Table 4 logMAR BCVA improvement between the two groups n (%)
DISCUSSION
The clinical effect of IVC combined with PRP and PRP alone in patients with SNPDR and absence of ME was first compared in this study. The findings show that in most patients, both treatment regimens preserved good VA. However, by reducing PRP-induced ME, the combination therapy was more successful and rapid; BCVA was improved by combination therapy than PRP alone.
To reduce the frequency of visual loss and avoid subsequent NV, PRP should be conducted in patients with severe nonproliferative or early PDR, according to the recommendations of the ETDRS[18]. However, studies have shown that PRP decreased moderate VA in the treatment group by 25%-43%,causing ME, which is the most common cause of VA decline in diabetic eyes[19]. Therefore, the implementation of PRP is hesitated by diabetic patients with SNPDR or nonhigh risk PDR, especially those with good vision. In our study, 81.48%of patients' demonstrated stable or improved VA, 18.52% had decreased VA in the PRP group with no significant difference in VA between baseline and 6mo after PRP. Ganekalet al[20],Shimuraet al[21], McDonald and Schatz[22]reported that stable and improved vision rates were 81.58% and 85%, respectively,in patients with PDR, and no clinically significant ME, whereas 18.42% or 15% of patients had decreased vision after PRP,similar to our results. Compared with other studies, the clinical significance of ME may be caused by pre-existing ME and uncontrolled systemic conditions before and after PRP, leading to decreased vision after PRP[19,22]. In this study, all participants received appropriate treatment for their general diabetes and hypertension status, accompanied by well-controlled HbA1c level and blood pressure during follow-up.
In this study, the changes of CFT were increased in the PRP group at 1mo after PRP before was slowly decreased. CFT at 6mo of follow-up was still higher than that at baseline but did not exceed the range of 368-572 μm for clinical significance of ME[20]. However, VA was decreased significantly after 1 and 3mo of PRP. With follow-up time, VA was steadily improved,reaching the baseline level at the end of follow-up. Therefore,according to the findings of Diabetic Retinopathy Clinical Research Network[23], the thickness of fovea in OCT is not correlated with VA. The measurement of fovea thickness may not be a practical guide for VA. This was also consistent with the findings of Leeet al[15]that VA in patients with severe diabetic retinopathy without ME has not affected by mild macular thickening persists and PRP. It was noteworthy that laser photocoagulation in this study was not conducted in the macular region. The increase in macular thickening was triggered by PRP damage to the perimacular tissue. The heat conduction of retinal photocoagulation from retinal pigment epithelium reaches the retina, causing focal inflammation and likely contributing to ME[24-27]. To further strengthen the therapeutic effect of PRP and solve the issue of rapid vision loss and VH after PRP, the combination of intravitreal injection of anti-VEGF drugs and laser photocoagulation has been proposed by many researchers[28-31]. In this study, we used the characteristics of conbercept of lower VEGF dissociation rate, higher binding affinity, decreased extracellular matrix adhesion, and a longer clearance time to combine with PRP to observe its safety and effectiveness. Our data confirmed that conbercept reduced PRP-induced ME and prevented PRPinduced visual dysfunction. In the pulse group, combined treatment increased BCVA, resulting in more significant vision gain than in the PRP group; the 100% rate of effectiveness in VA was also higher than that in the PRP group (81.48%).
These findings suggest that the combined therapy was superior to PRP alone in improving VA and CFT, and the increase in VA and decrease in CFT were significant after 1mo with one dose of IVC. More importantly, improving vision within a short time frame increases patients' satisfaction, the treatment confidence, and boosts the cure rate.
IVC may play a synergistic role with PRP in reducing angiogenesis, leakage, restoring retinal transparency, decreasing the need for high laser energy and effectively reducing ME,which might explain the results. In this study, IVC before PRP did not prevent the transient increase in CFT 1mo after PRP. Shimuraet al[21]considered that to inhibit the damage caused by additional photocoagulation, a one-week interval of PRP treatment was inadequate to recover from the macular damage and retinal injury of 500 burns. Their results showed that biweekly treatments could restore macular thickening more quickly after PRP than weekly treatment. However,changes in the progression of retinopathy might increase over a more extended period of treatment. Perhaps, IVC combined biweekly PRP is a new alternative in the future.
The small sample size and short follow-up period were the limitations of our study. It is necessary to implement further researches with larger sample size and longer follow-up, for example, more than 12-month, in the future. Meanwhile, visual function after treatment was not evaluated for both groups.Furthermore, there was a lack of automated quantitative approaches for assessing hard exudate and the amount of microaneurysms,which are closely linked to the progression of diabetic retinopathy.
In conclusion,for patients with SNPDR without ME, PRP alone and IVC combined with PRP treatment could maintain good VA. However, IVC seems to be a promising adjunctive therapy for PRP, and the combination therapy may increase BCVA and prevent visual loss and ME caused by PRP.
ACKNOWLEDGEMENTS
We thank all participants in this study. Thanks to the assistance of Dr. Han JN, Zhao Y and other doctors, the ophthalmology examination was completed.
Conflicts of Interest: Zhao N,None;Guan J,None;Cai N,None;Liu NN,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Comment on: Real-world outcomes of two-year Conbercept therapy for diabetic macular edema
- Efficacy of conbercept after switching from bevacizumab/ranibizumab in eyes of macular edema secondary to central retinal vein occlusion
- lntraoperative complication rates in cataract surgery performed by resident trainees and staff surgeons in a tertiary eyecare center in Hungary
- Comparing surgical efficiencies between phacoemulsification systems: a single surgeon retrospective study of 2000 eyes
- Factors associated with corneal astigmatism change after ptosis surgery
- Outcomes of different lines of keratoconus management in a tertiary eye center in north China
