Outcomes of different lines of keratoconus management in a tertiary eye center in north China
2022-04-19JingZhangXianLiDuLeiWanYanLingDongLiXinXie
INTRODUCTION
There are racial differences in the presentation of keratoconus
.Both Asians and Caucasians were studied by Pearson
.Compared with Caucasians, Asians were found to have a fourfold increase in keratoconus incidence, with younger presentation and earlier requirement for corneal grafting.Our current study presents a large-scale Asian population of keratoconic patients. The average age of the patients at the initial diagnosis was consistent with previous reports involving Asians
. The ratio of male to female was 3.7:1, which was consistent with most previous studies.
At present, rigid gas permeable (RGP) lens wear, corneal collagen crosslinking (CXL) and keratoplasty are the main treatments for keratoconus
. However, there has been no adequate clinical classification system developed for keratoconus; the historical Amsler-Krumeich classification does not incorporate current information and technological advances
. Many studies have explored and establishing a new classification system for keratoconus, but no scheme has involved therapeutic classification
. A therapeutic classification that is reasonably accurate and readily adoptable could help us to answer the challenging question regarding which treatment is most appropriate for different stages of keratoconus. Shandong Eye Institute is a tertiary eye center in north China capable of providing a variety of treatment options for keratoconic patients, such as RGP, CXL, and corneal transplantation. We retrospectively studied our population of keratoconic patients over a 20-year period to evaluate the outcomes of different treatment approaches and to provide data to inform further research.
坤二少爷自幼聪颖,三岁能背唐诗百首,四岁呤诗作赋,乡人谓之神童。只憾张神童生逢乱世,读至县立麟山中学时,尚未完成学业学校停办,便辍学回乡。适逢老父过世,长兄张铁头闯荡江湖,油坊无人打理,便子承父业,年方十六做了油坊主。
SUBJECTS AND METHODS
This study was approved by the Ethics Committee of Shandong Eye Institute and adhered to the tenets of the Declaration of Helsinki. Informed consent was obtained from all subjects in this study. None participants received a stipend. Medical records of patients with keratoconus treated with RGP lens wear, CXL, and corneal transplantation at Shandong Eye Institute between January 1997 and December 2017 were reviewed. Patients with other concurrent eye diseases or previous eye surgeries were excluded.
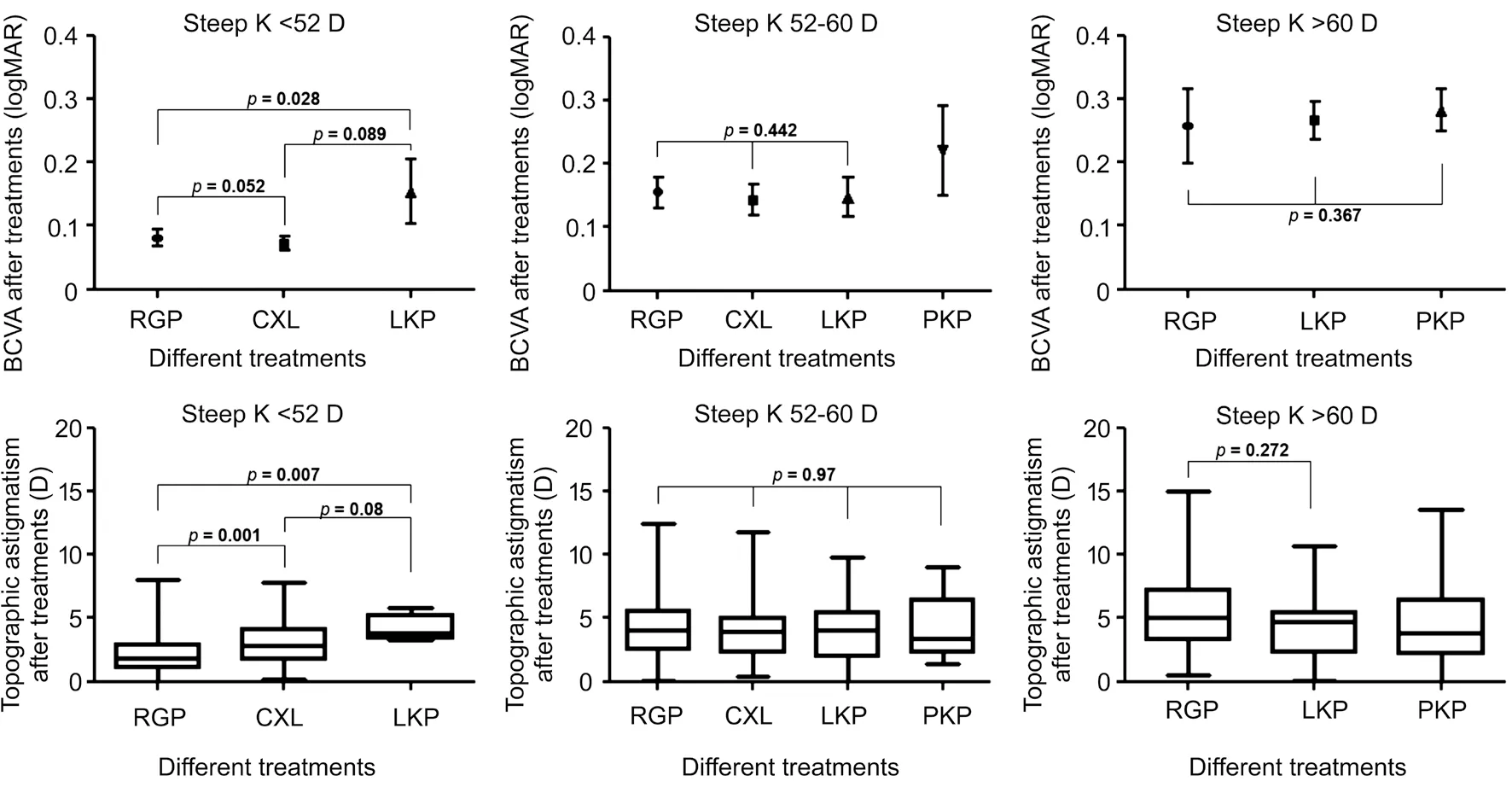
When the steep K was between 52 to 60 D, the BCVA in the eyes treated with RGP lens, CXL and LKP was 0.16±0.25,0.14±0.14, and 0.15±0.12 logMAR respectively (
=0.442).The TA in the eyes treated with RGP lens, CXL, LKP and PKP was 4.1±2.2, 4.1±2.5, 4.0±2.8, and 4.2±2.0 D, respectively(
=0.97).
Statistical analyses were performed using SPSS (version 22.0,IBM SPSS Inc., Chicago, IL, USA). Descriptive statistics were reported as means±standard deviation (SD). Normality of data distribution was tested using the 1-sample Kolmogorov-Smirnov test. Differences between before and after treatment were assessed with the paired-samples
-test if variables had a normal distribution and with the Wilcoxon signed-rank test if the variables did not have a normal distribution. Differences in steep K groups were assessed with the one-way analysis of variance (ANOVA) if variables had a normal distribution with equal variance and with the Mann-Whitney
test or the Kruskal-Wallis test if the variables did not have a normal distribution or had unequal variance. The endothelial cell density (ECD) between the lamellar keratoplasty (LKP) and penetrating keratoplasty (PKP) groups at different time points was assessed with the Mann-Whitney
test. Frequency analyses were performed using the Fisher's exact Chi-square test. Basic characteristic differences between the treatment groups were compared using ANOVA. Logistic regression analysis was used to detect the related factors for keratoplasty options. The receiver operating characteristic (ROC) curve analysis was performed to test the ability of analysed variables to distinguish between keratoplasty and non-keratoplasty. The area under the receiver operating characteristic curve (AUC)with 95% confidence interval (95%CI) was estimated, and the optimal cut-off values were determined. Comparison of the area under the AUCs was performed using the z-test. Twotailed
values less than 0.05 were considered statistically significant.
As the time span of this study was large, only the results from the same type of corneal topography systems for individual patients were included to avoid any errors caused by instrument difference. The corneal topography equipment included the Tomey screening system (Tomey Corp, Nagoya, Japan),the Obscan II (Bausch & Lomb, Rochester, NY, USA), and the Oculus Pentacam (Oculus Optikgerate GmbH, Wetzlar,Germany).
The patients were grouped into a mild-moderate group and an advanced group according to the CLEK (the Collaborative Longitudinal Evaluation of Keratoconus) Study
. The advanced group was further divided into a steep K<60 D group and steep K>60 D group. Relevant patient details were documented, including gender, age, time of first consultation at our institute, treatment selections, best corrected visual acuity(BCVA), corneal curvature, topographic astigmatism (TA), and thinnest corneal thickness (TCT) before treatment. For all eyes with follow-up>18mo after treatment, the corneal curvature,BCVA, TA, and TCT at the final follow-up point were recorded. The occurrence, timing, and treatment of related complications were also recorded.
RESULTS
The patients were 913 males and 249 females, with a gender ratio of 3.7:1. The average age at initial diagnosis was 20.9±6.0y(range, 6-58y). The average age was 20.5±5.5y (range, 6-48y)in males and 22.3±7.5y (range, 11-58y) in females (
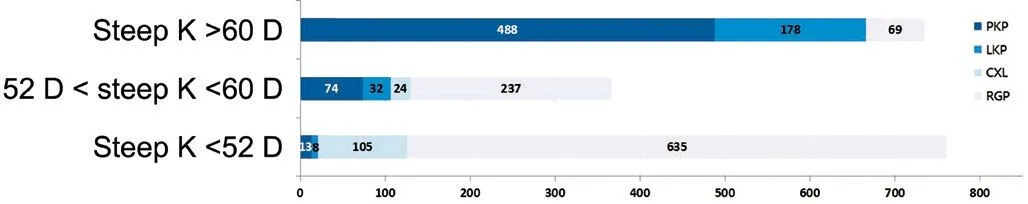
<0.001).Among the keratoconic eyes, 50.5% (941/1863) of the eyes wore RGP lenses, 6.9% (129/1863) underwent CXL, 11.7%(218/1863) had lamellar keratoplasty (LKP), and 30.9%(575/1863) had penetrating keratoplasty (PKP). In the eyes with steep K<52 D, nonsurgical management (RGP) accounted for 83.4%, while in the eyes with steep K>60 D, surgical management (CXL, LKP, and PKP) accounted for 90.6%(Figure 1).
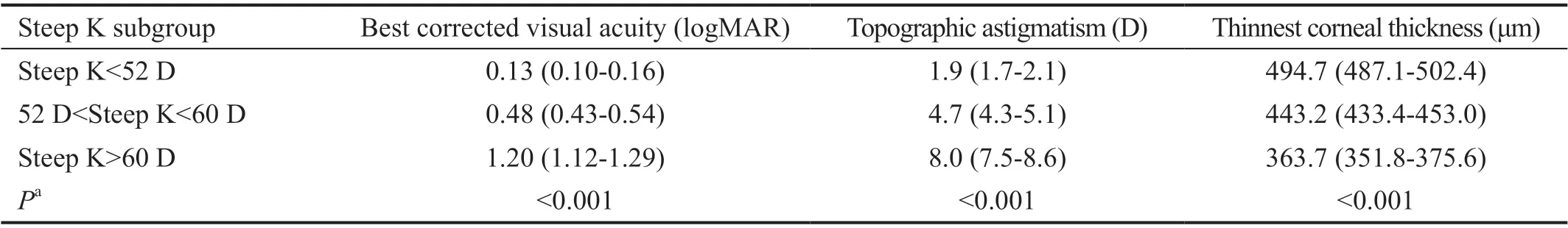
There were 618 eyes for which the follow-up was more than 18mo after treatment. The 348 (56.3%) eyes wore RGP lenses,for which the follow-up was 54.0±31.9mo (range, 18.1-172.1mo).Totally 90 eyes (14.6%) underwent CXL, for which the follow-up was 22.3±3.7mo (range, 18.1-32.3mo). The 75 eyes (12.1%)had LKP, for which the follow-up was 47.9±30.5mo (range,18.2-156.1mo) and 105 eyes (17.0%) had PKP, for which the follow-up was 57.3±45.9mo (range, 18.3-241.9mo). The steeper curvature was accompanied by worse BCVA, greater TA, and thinner corneal thickness before treatment (Table 1).
Outcomes of Treatments
At the last time of follow-up, the best contact lens corrected visual acuity(BCLVA) after RGP lens wear was better than the best spectacle corrected visual acuity (BSCVA) before treatment(0.12±0.22 logMAR, 0.32±0.32 logMAR, respectively,
<0.001,
=348). Higher steep K values were associated with lower BCLVA after treatment (
<0.001). The mean steep K value improved from 50.9±5.9 to 51.4±6.9 D (
=0.009). The mean TA decreased from 3.5±2.4 to 3.1±2.3 D (
<0.001).The mean TCT decreased from 480.1±46.1 to 466.2±48.4 μm(
<0.001; Table 2).
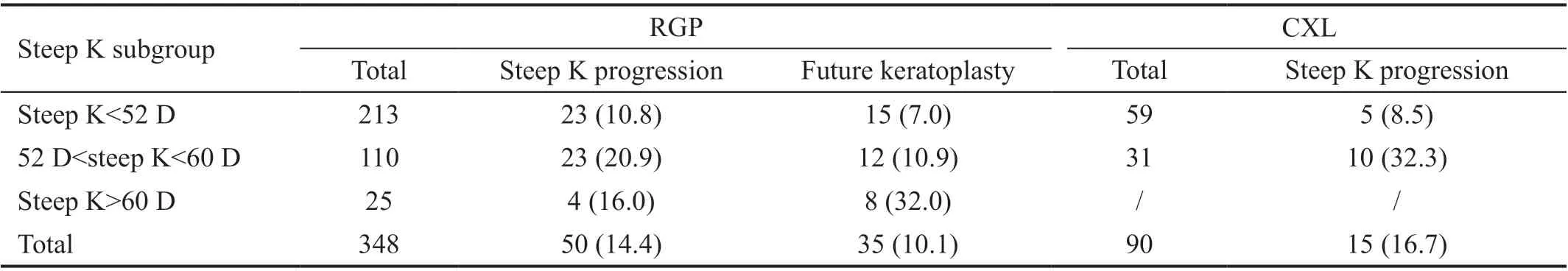
The incidence of steep K progression in the eyes with RGP lenses was 14.4% (50/348). In the setting of larger initial steep K (>52 D) 20.0% (27/135) had progression, while 10.8%(23/213) progressed in the setting of lower initial steep K(<52 D;
=0.019). The 10.1% (35/348) of the eyes underwent keratoplasty after 29.6±20.1mo (range, 3.2-82.5mo) of RGP lens wear, with a significant difference between steep K>52 D subgroup and steep K<52 D subgroup (14.8% and 7.0%,respectively,
=0.027). In the 135 eyes in which steep K was>52 D, the probability of future keratoplasty was significantly higher in the steep K>60 D subgroup versus steep K<60 D subgroup (32.0% and 10.9%, respectively,
=0.008; Table 3).
As of the last follow-up, BCVA improved from 0.21±0.19 logMAR to 0.10±0.11 logMAR after CXL (
<0.001,
=90). Higher steep K values were associated with lower BCVA after treatment(
=0.003). The steep K, TA and TCT after treatment showed no significant difference compared to preoperative among all K subgroups (Table 2).
The incidence of steep K progression in the eyes that underwent CXL was 16.7% (15/90), with a significantly higher incidence in the steep K>52 D subgroup compared to the steep K<52 D subgroup (32.3% and 8.5%, respectively,
=0.007;Table 3).
At the last follow-up, the BCVA had improved from 0.94±0.57 to 0.24±0.21 logMAR after LKP (
<0.001,
=75). The BCVA after LKP was 0.27±0.22 logMAR in the steep K>60 D subgroup, and 0.15±0.12 logMAR in the subgroup in which steep K was between 52 to 60 D(
=0.025). The mean steep K value decreased from 62.7±5.3 to 46.6±2.7 D (
<0.001). The mean TA decreased from 8.4±3.9 to 4.4±2.4 D (
<0.001). The mean TCT increased from 380.5±62.5 to 545.6±42.5 μm (
<0.001; Table 2).
At the last follow-up, the BCVA had improved from 1.22±0.53 to 0.27±0.32 logMAR after PKP (
<0.001,
=105). The BCVA after PKP showed no significant difference among different curvature subgroups(
=0.611). The mean steep K value decreased from 67.3±6.7 to 47.8±4.1 D (
<0.001). The mean TA decreased from 6.6±3.3 to 4.6±3.1 D (
<0.001). The mean TCT increased from 356.8±75.3 to 504.2±37.4 μm (
<0.001; Table 2).
The rate of immune rejection was 1.3% (1/75) after LKP and 8.6%(9/105) after PKP (
=0.047). After PKP rejection, the BCVA decreased to 0.53±0.42 logMAR (
=0.012).
Steep K is an important grading treatment indicator. When steep K is <52 D, RGP lenses should be recommended. It is the best time for LKP when the steep K ranges from 52 to 60 D.
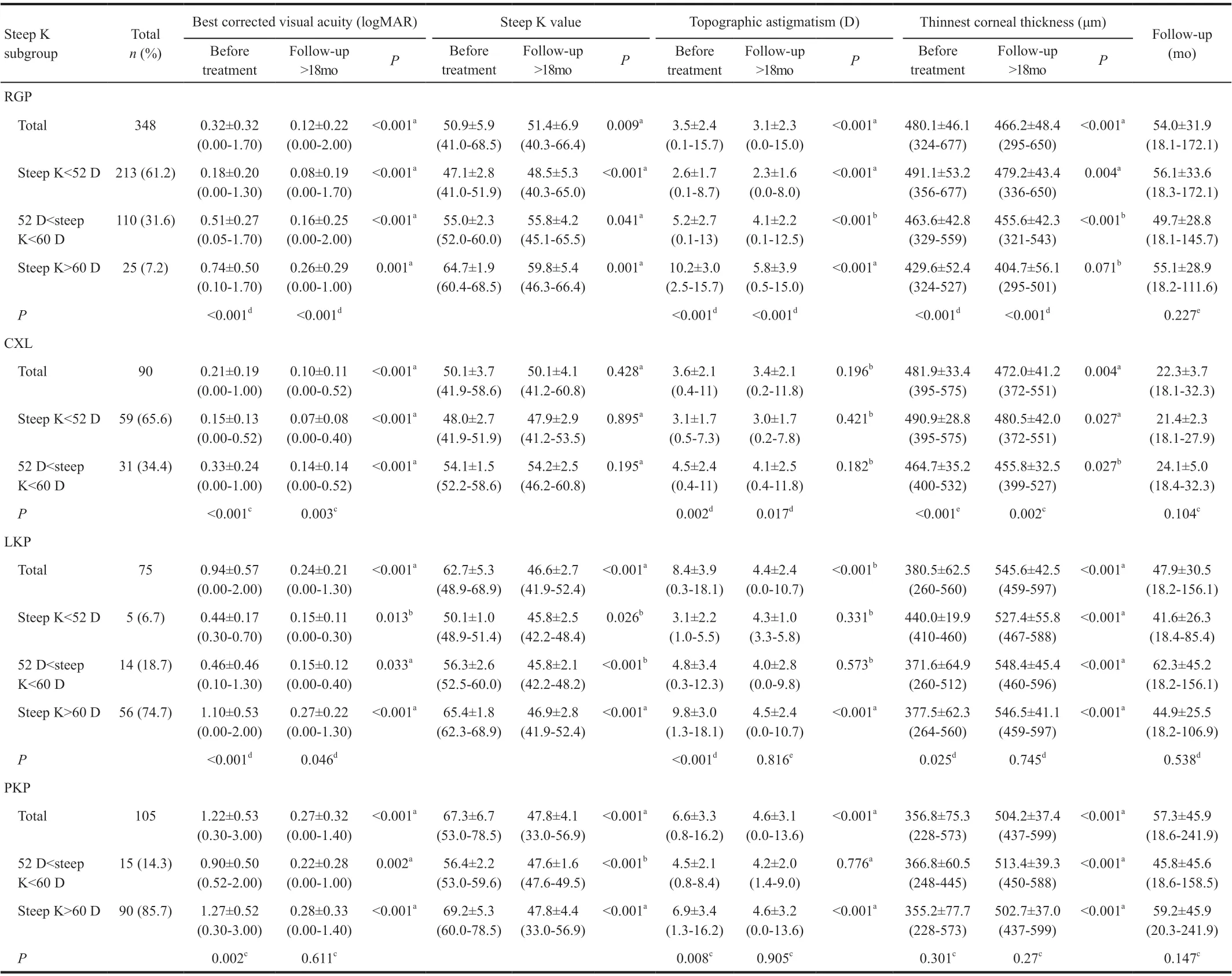
When the steep K was <52 D, the BCVA after treatment in the eyes with RGP lens, CXL and LKP was 0.08±0.19, 0.07±0.08, and 0.15±0.11 logMAR respectively(
=0.017). Among them, the RGP group was better than LKP group (
=0.028); the difference did not reach significance between CXL group and LKP group (
=0.089), and the RGP and LKP group (
=0.052). The TA after treatment in the eyes with RGP lens, CXL and LKP was 2.3±1.6, 3.0±1.7, and 4.3±1.0 D, respectively (
<0.001). Among them, the RGP group was lower than the LKP group (
=0.007) and CXL group (
=0.001); the CXL group and LKP group were not significantly different (
=0.08).
2.6 两组不良反应发生率比较 研究组不良反应发生率低于对照组,差异有统计学意义(P<0.05)。见表6。
A total of 1162 patients (1863 eyes) with keratoconus who fit the following inclusion criteria were included: clinically evident keratoconus defined by the evidence of one or more of the following clinical findings using the slit-lamp microscopy in at least one eye: corneal stromal thinning, conical protrusion of the cornea at the apex, Fleischer ring, Vogt's striae, and anterior corneal scarring
.
Contralateral eyes of patients with clinical keratoconus in one eye were also included. Patients with keratoconus who did not receive any treatment were excluded.
When the steep K was >60 D, the BCVA and TA after treatment in the eyes with RGP lens, LKP and PKP showed no significant difference (Figure 2).
选种抗病品种,播种无菌种子;轮作倒茬病苗病秧清出田外深埋或烧毁,消灭病原载体。病秧不还田;推广滴灌和配方施肥,推广配方叶面肥,提高农田作业质量,规范田间管理,创造适合食葵生长发育的优良环境条件,培育壮苗,抵抗病菌入侵;加强栽培管理合理施肥灌水,不偏施氮肥,生长后期打掉植株下部的黄叶、老叶,保持田间通分透光,增强植株的抗病能力。
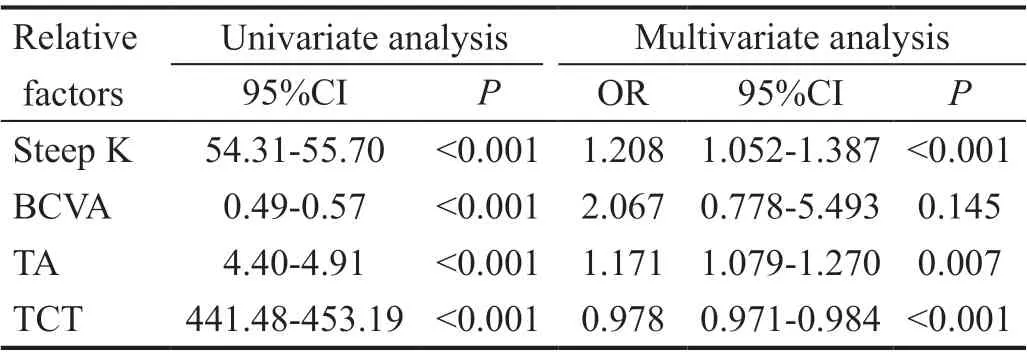
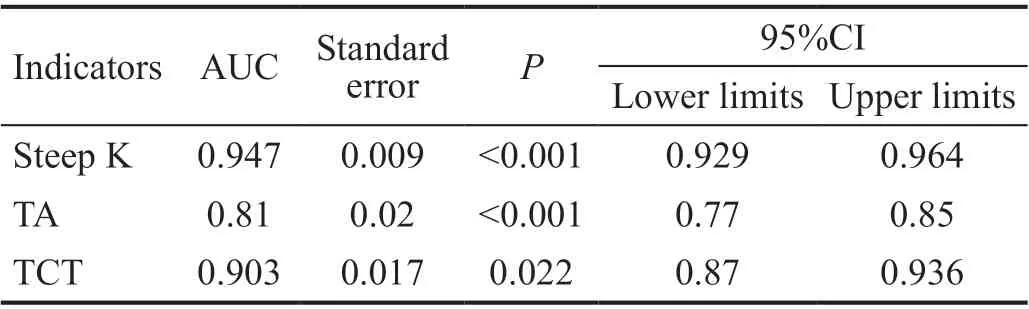
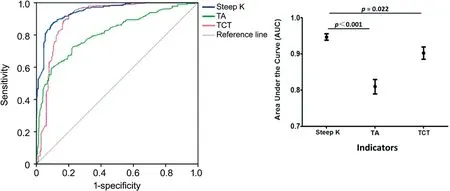
The results of the univariate and multivariate regression analyses are summarized in Table 4. Univariate analyses revealed that treatment options to keratoconus was significantly associated with the steep K (
<0.001), BCVA (
<0.001), TA(
<0.001), and TCT (
<0.001). The following factors in the multivariate analysis remained a significant relation with the different treatments: steep K [odds ratio (OR)=1.208, 95%confidence interval (CI): 1.052-1.387], TA (OR=1.171, 95%CI:1.079-1.270), and TCT (OR=0.978, 95%CI: 0.971-0.984). A comparative analysis of steep K, TA, and TCT was performed to unveil a predictive index power. Unsurprisingly, the level of steep K, TA, and TCT followed the treatment choice between the keratoplasty and non-keratoplasty, although steep K reached the most significant meaning (AUC=0.947,
<0.01)
TA (AUC=0.81,
=6.247,
<0.01) and TCT (AUC=0.903,
=2.287,
=0.022; Table 5 and Figure 3). While looking for a promising steep K cut-off, we observed that 57.2 D allows for the diversification of whether the keratoplasty should be chosen, and showed a sensitivity of 87.8% with a specificity of 89.5%.
三是农田灌溉工程规模化管理适应了市场经济制度要求。政府投资或补助建设的农田水利工程,一般是移交给工程所在村集体安排管理,而村集体安排的管理一般只是收取电力运行费,不收取工程折旧费和维护费,管理好的村庄在工程维修上由村集体给予补贴或按照 “一事一议”原则召开会议研究筹集,协调成本高昂,如果筹资协调不成还将导致工程瘫痪。以往村集体所管理的农田水利工程大都只是一个福利工程,并且有可能只是村里一部分人的,这个福利工程是没有维护经费保障的,随时面临着中止运行的风险。而规模化管理将农田水利工程灌溉服务作为商品,进行成本核算,工程运行和维护等管理费用有着落,有利于工程的可持续使用。
DISCUSSION
The description of keratoconus was first published 150 years ago. During the past two decades, the diagnosis and management of keratoconus has undergone a revolution of technological advances in surgical options and equipment.Experts reached a global consensus on keratoconus in 2015:abnormal posterior ectasia, abnormal corneal thickness distribution, and clinical noninflammatory corneal thinning are now mandatory findings for diagnosis of keratoconus. True unilateral keratoconus is exceedingly rare or non-existent
.
There has been no adequate clinical classification system for keratoconus
. As the most widely used keratoconus classifications, both the Amsler-Krumeich classification and the CLEK Study used corneal curvatures as their only or primary indicators for classification. In the current study, steeper curvature was accompanied by worse BCVA, greater TA, and thinner corneal thickness before treatment. This demonstrates the importance of K values in the severity grading of keratoconus. Sray
reported that, in addition to corneal scarring, the steep corneal curvature was the most relevant risk factor for PKP, and a cut-off level for this higher risk corneal curvature was identified at 55 D (mean K) by Reeves
;the base curve of RGP lens is based on the corneal curvature;a steep curvature is directly related to the probability of RGP lens fitting. In analysis the current study population, as steep K increased, the proportion of surgical treatment became higher,demonstrating the influences of curvature on the selection of treatments for keratoconus. A higher steep K value appeared to have several adverse implications for the various treatment groups: the BCVA after treatment decreased gradually whether treated with RGP lens, CXL or LKP group; the incidence of steep K progression increased in RGP lens and CXL groups;the probability of future keratoplasty increased in the RGP lens group. These data demonstrate the important influences of K values on the outcome of keratoconic treatment.
Halting disease progression and recovering vision are two major goals in the management of keratoconus
. When steep K was >52 D, RGP lenses lost their advantage in vision correction.The longest follow-up of keratoplasty was 20y in this study,which showed that the current corneal transplantation can provide patients with long-term satisfactory vision correction.The incidence of keratoconus is a slowly increasing
.Recently, more research has focused on the role of CXL in improving vision and halting the progress of keratoconus
.In these studies, almost all failed cases (progression of disease or repeated CXL) occurred in eyes with corneal curvature over 55 D or 58 D, with a failure rate ranging from 7.6% to 12.36%
. In the current study, as the steep K value increased,the incidence of keratoconus progression increased, while the steep K and TA showed no changes after CXL. It is necessary to assess the longer-term results of CXL in steep curvature.
马克思列宁主义关于人民群众历史观的理论和实践,也深刻影响着中国共产党的发展方向、目标选择以及旗帜道路。中国共产党在领导中国革命、建设和改革中,为人民群众谋利益,遵从人民群众的首创精神,与人民群众同呼吸、共命运,又创造性地运用和发展了马列主义群众史观,使其焕发出顽强的生命力和持续的创新力。基于此,马克思列宁主义群众史观就成为中国共产党群众史观生成的逻辑起点。
采用回顾性调研的方法,收集患者相关信息(性别、年龄、体重、体格特征、实验室检查指标等)进行统计和分析。信息内容见表1。
In contrast to CXL, corneal transplantation is the traditional treatment for keratoconus. Keratoplasty can provide a satisfactory visual acuity for keratoconic patients of varied races
. LKP has been recognized as superior to PKP,and this finding is reinforced by our data
. Our group successfully modified deep LKP and employed it for the treatment of advanced keratoconus with steep curvature
.
Concerns about keratoplasty have focused on rejection of allografts and long-term graft survival. The rate of rejection after keratoplasty, particularly LKP, for keratoconus is much lower than for other diseases. The corneal endothelial cell loss rate slowed down over time
. It is worth noting that even if ECD dropped to 1000 cells/mm
or less, endothelial dysfunction did not appear in the current study. This suggests that the occurrence of endothelial dysfunction requires some additional stimulating factors, such as inflammation and rejection, to disrupt the balance of corneal endothelial compensation mechanisms. Absent such stimuli, the corneal endothelium can maintain its own homeostasis for extended periods.
It is important to achieve a global consensus on the management of keratoconus. We propose that when steep K is <52 D, RGP lenses should be recommended because of their better BCVA.When steep K is between 52 to 60 D, the BCVA and TA after treatment in the eyes with RGP lens, CXL and LKP showed no significant difference, but the risk of curvature progression became higher. So, the patients should be monitored more closely in order to best time LKP. In the current study, when steep K is 57.2 D, LKP should be required. If LKP is delayed,BCVA may be worse, and PKP may even be required, followed by the risk of corneal endothelial dysfunction
. Further research of a promising steep K cut-off for the diversification of whether the CXL should be chosen in steeper K group is needed. At the same time, we also pay attention to the treatment progress of RGP and CXL to continuously update our grasp of the treatment boundary
.
The existing keratoconus therapies include corneal surgery,refractive surgery, and optical correction, which may involve multiple subspecialties. Long-term goal-directed therapy is needed for the treatment of keratoconus. Steep
K, which can reflect the severity of keratoconus and has a major impact on treatment options and outcomes, appears to be a reasonably accurate and readily adoptable classification scheme to assist in treatment decisions. We speculate that improvements may be achievable by adjusting the grading point of steep K, or designing a more accurate therapeutic classification based on the steep K by introducing BCVA and corneal thickness as subindicators. However, the steep K is an undoubtedly important therapeutic classification indicator in the current retrospective study.
当下,创新成了最高频的词。习总书记多次强调,创新驱动发展,创新是发展的第一动力。教育改革就是要着力培养学生的学习能力、创新能力、解决问题的能力和主动适应社会的能力,创新学习正是基于这四种能力的一种教育思想和教育理论。它致力于解决我国基础教育中普遍存在的“重教轻学”“重接受轻创新”的弊病,着力解决三个问题:一是转变教师教学观念,使教师具备“创新学习”的理念。二是变革课堂教学方式,使教师通过创新学习原理的自觉运用,在“教”与“学”的双主体互动关系中,创造出生动活泼的课堂。三是让广大中小学生想创新、能创新、会创新,掌握创新学习的方法与技能。
Supported by the Natural Science Foundation of Shandong Province (No.ZR2015YL037); the Innovation Project of Shandong Academy of Medical Sciences (No.2018-21).
None;
None;
None;
None;
None.
1 Gomes JAP, Tan D, Rapuano CJ, Belin MW, Ambrósio R Jr, Jr G,Malecaze F, Nishida K, Sangwan VS, Group of Panelists for the Global Delphi Panel of Keratoconus and Ectatic Diseases. Global consensus on keratoconus and ectatic diseases.
2015;34(4):359-369.
2 Parker JS, van Dijk K, Melles GRJ. Treatment options for advanced keratoconus: a review.
2015;60(5):459-480.
3 McMahon TT, Szczotka-Flynn L, Barr JT, Anderson RJ, Slaughter ME,Lass JH, Iyengar SK, Group CLEKS. A new method for grading the severity of keratoconus: the Keratoconus Severity Score (KSS).
2006;25(7):794-800.
4 Li XH, Yang HY, Rabinowitz YS. Keratoconus: classification scheme based on videokeratography and clinical signs.
2009;35(9):1597-1603.
5 Rabinowitz YS. Keratoconus.
1998;42(4):297-319.
6 Szczotka LB, Barr JT, Zadnik K. A summary of the findings from the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study.CLEK Study Group.
2001;72(9):574-584.
7 Ferrari G, Rama P. The keratoconus enigma: a review with emphasis on pathogenesis.
2020;18(3):363-373.
8 Pearson AR, Soneji B, Sarvananthan N, Sandford-Smith JH. Does ethnic origin influence the incidence or severity of keratoconus?
(
) 2000;14(Pt 4):625-628.
9 Naderan M, Shoar S, Rezagholizadeh F, Zolfaghari M, Naderan M.Characteristics and associations of keratoconus patients.
2015;38(3):199-205.
10 Shirayama-Suzuki M, Amano S, Honda N, Usui T, Yamagami S,Oshika T. Longitudinal analysis of corneal topography in suspected keratoconus.
2009;93(6):815-819.
11 Sray WA, Cohen EJ, Rapuano CJ, Laibson PR. Factors associated with the need for penetrating keratoplasty in keratoconus.
2002;21(8):784-786.
12 Reeves SW, Stinnett S, Adelman RA, Afshari NA. Risk factors for progression to penetrating keratoplasty in patients with keratoconus.
2005;140(4):607-611.
13 Ezzeldin M, Filev F, Steinberg J, Frings A. Excimer laser treatment combined with riboflavin ultraviolet-A (UVA) collagen crosslinking(CXL) in keratoconus: a literature review.
2020;40(9):2403-2412.
14 Badawi AE, Abou Samra WA, El Ghafar AA. Predictive factors of the standard cross-linking outcomes in adult keratoconus: one-year follow-up.
2017;2017:4109208.
15 Hersh PS, Stulting RD, Muller D, Durrie DS, Rajpal RK. United states multicenter clinical trial of corneal collagen crosslinking for keratoconus treatment.
2017;124(9):1259-1270.
16 Raiskup F, Theuring A, Pillunat LE, Spoerl E. Corneal collagen crosslinking with riboflavin and ultraviolet-A light in progressive keratoconus: ten-year results.
2015;41(1):41-46.
17 Myerscough J, Roberts H, Yu AC, Elkadim M, Bovone C, Busin M. Five-year outcomes of converted mushroom keratoplasty from intended deep anterior lamellar keratoplasty (DALK) mandate 9-mm diameter DALK as the optimal approach to keratoconus.
2020;220:9-18.
18 Daniel MC, Bӧhringer D, Maier P, Eberwein P, Birnbaum F, Reinhard T. Comparison of long-term outcomes of femtosecond laser-assisted keratoplasty with conventional keratoplasty.
2016;35(3):293-298.
19 Li H. Comparison of long-term results after manual and femtosecond assisted corneal trephination in deep anterior lamellar keratoplasty for keratoconus.
2020;13(4):567-573.
20 Song YW, Zhang J, Pan ZQ. Systematic review and meta-analysis of clinical outcomes of penetrating keratoplasty versus deep anterior lamellar keratoplasty for keratoconus.
2020;18(4):417-428.21 Shi WY, Li SX, Gao H, Wang T, Xie LX. Modified deep lamellar keratoplasty for the treatment of advanced-stage keratoconus with steep curvature.
2010;117(2):226-231.
22 Armitage WJ, Dick AD, Bourne WM. Predicting endothelial cell loss and long-term corneal graft survival.
2003;44(8):3326-3331.
23 Writing Committee for the Cornea Donor Study Research Group,Lass JH, Benetz BA, Gal RL, Kollman C, Raghinaru D, Dontchev M,Mannis MJ, Holland EJ, Chow C, McCoy K, Price FW Jr, Sugar A,Verdier DD, Beck RW. Donor age and factors related to endothelial cell loss 10 years after penetrating keratoplasty: Specular Microscopy Ancillary Study.
2013;120(12):2428-2435.
24 Inoue T, Hara Y, Kobayashi T, Zheng XD, Suzuki T, Shiraishi A,Ohashi Y. Corona sign: manifestation of peripheral corneal epithelial edema as a possible marker of the progression of corneal endothelial dysfunction.
2016;60(5):349-356.
25 Iqbal M, Elmassry A, Tawfik A, Abou Samra W, Elgharieb M,Elzembely H, Soliman A, Saad H, El Saman I, Saeed A, Farouk M, Tawfik T, Abou Ali A, Fawzy O. Analysis of the outcomes of combined cross-linking with intracorneal ring segment implantation for the treatment of pediatric keratoconus.
2019;44(2):125-134.
猜你喜欢
杂志排行
International Journal of Ophthalmology的其它文章
- Comment on: Real-world outcomes of two-year Conbercept therapy for diabetic macular edema
- Efficacy of intravitreal conbercept combined with panretinal photocoagulation for severe nonproliferative diabetic retinopathy without macular edema
- Efficacy of conbercept after switching from bevacizumab/ranibizumab in eyes of macular edema secondary to central retinal vein occlusion
- lntraoperative complication rates in cataract surgery performed by resident trainees and staff surgeons in a tertiary eyecare center in Hungary
- Comparing surgical efficiencies between phacoemulsification systems: a single surgeon retrospective study of 2000 eyes
- Factors associated with corneal astigmatism change after ptosis surgery
