A systematic review and meta-analysis for platelet-rich plasma in treatment of knee osteoarthritis
2022-04-07RongXieShangQuanWangLingHuiLiXuWeiJieYuJiaWenZhanRuiXieXiaoJuanChangLiGuoZhu
Rong Xie, Shang-Quan Wang, Ling-Hui Li, Xu Wei, Jie Yu, Jia-Wen Zhan, Rui Xie,Xiao-Juan Chang, Li-Guo Zhu✉
1. Beijing University of Chinese Medicine, Beijing 100029, China
2. Wangjing Hospital of China Academy of Traditional Chinese Medical Scinences, Beijing 100102, China
Keywords:Platelet-rich plasma Knee osteoarthritis Pain Function Double-blind controlled trials Systematic review Meta-analysis
ABSTRACT Objective: To systematically evaluate the efficacy and safety of platelet-rich plasma in patients with knee osteoarthritis. Methods: The Pubmed, Cochrane Library, Embase,and Medline were investigated from 2005 through May 2020.All randomized double-blind controlled trials were included the effect of PRP injections for KOA. Literature screening and data extraction were carried out independently by two researchers, and the quality of the included randomized controlled trials was evaluated one by one according to the Cochrane collaboration standards.Meta-statistical analysis was performed for the studies that met the inclusion standards using RevMan5.3. Results: In this study,(1)Seven studies met the eligibility criteria, including 250 patients in the experiment (PRP)group and 230patients in the control(no PRP)group.(2)Metaanalysis results showed that the WOMAC Scores was differed significantly between the PRP and no PRP groups at the 6 months follow-up(MD=9.63,95%CI:3.29 to 15.96,P=0.003),and 12 months follow-up(MD=3.85,95%CI:2.66 to 5.04,P<0.00001)(P<0.05).In a comparison of KOOS function scores at the 6 months follow-up, PRP improved knee function scores more than no PRP(MD=8.63,95%CI:0.85 to 16.42,P=0.03) (P<0.05).PRP injections reduced pain more effectively than no PRP injections in patients with KOA at 3,6 months of follow-up, and the VAS pain score showed a significant difference(SMD=0.88,95%CI:0.13 to 1.62,P=0.02)(SMD=0.85,95%CI:0.11 to 1.59,P=0.002)(P<0.05). However, Adverse Events (AEs) were all not significantly different(RR=0.96,95%CI:0.65 to 1.40,P=0.82)(P>0.05).(3)Results showed that PRP has significant advantages in pain relief and functional improvement. Conclusions:In improving knee function and relieving pain, PRP showed superiority to other non-surgical treatments in long-term follow-up from well-designed double-blind trials. Due to the limited quality and data, more high-quality multi-center studies are required.
1. Introduction
Knee osteoarthritis (KOA) is a common chronic osteoarticular degenerative disease in the elderly, which can lead to varying degrees of cartilage degeneration, hyperplasia and structural changes[1].Studies have shown that KOA is a chronic bone and joint disease related to age. According to the census data of 2000 in China, the number of symptomatic KOA patients in the population over 60 years old in China has reached 15 million[2].With the aggravation of degeneration, the main manifestations are knee joint pain, joint disorder and function limitation, which makes the quality of life of the elderly seriously decline[3].There are many nonsurgical treatments for KOA, including oral medications,functional exercises, intraarticular injections, and other conservative treatments[4-5].According to the American College of Rheumatology(ACR), nonsurgical treatment has become the first-line treatment for KOA and plays an important role in the management of KOA.Although there are reports [6-7] that non-surgical treatment can relieve pain and improve joint function in patients with early KOA,the limited efficacy of non-surgical treatment has become more and more obvious and has been proved to be unable to change the trend of joint degeneration [8], leading to total knee replacement for patients with severe KOA to improve their quality of life.
A large number of in vitro and in vivo studies have shown that growth factors contained in platelet-rich plasma (PRP) play an important role in tissue damage and cartilage degeneration [9-10].Growth factors can stimulate cell proliferation and differentiation,promote angiogenesis and accelerate tissue repair [11]. At the same time, platelets attract white blood cells to the site of the damage and reduce inflammation.At present, PRP has been used to treat degenerative diseases of bone and cartilage and soft tissue injury,playing an important anti-inflammatory and tissue regeneration role. However, the use of PRP injection therapy remains highly controversial.Filardo et al. [12] found more adverse events including pain, stiffness and swelling in patients treated with PRP injection.At the same time, studies [13] have proved that drugs including non-steroidal anti-inflammatory drugs (NSAID), corticosteroids and hyaluronic acid are safe and effective in alleviating pain and improving joint function in PATIENTS with KOA.However, many studies [14-18] have shown that injection of PRP is a safe and effective treatment for KOA, which can not only reduce inflammatory factors and synovial fluid in arthritic joints, but also significantly reduce pain and improve clinical function without increasing the risk of adverse events.Several recent systematic reviews have also demonstrated that PRP is effective compared to other non-surgical treatments, but there is no consensus on the advantages of PRP, particularly the lack of high-quality double-blind randomized controlled trials (DB-RCTs).The purpose of this study was to explore the efficacy and safety of PRP injection and other drug therapy for pain and functional level of KOA patients by comparing WOMAC, KOOS, VAS and AEs scores of different drugs for KOA patients with 12 months follow-up, and to provide evidence-based clinical guidance for the treatment of KOA.
2. Materials and methods
2.1 Literature search
All double-blind randomized controlled trials of PRP injection and KOA published in PubMed, Embase, Medline, Cochrane Library and other databases were searched from 2005 to May 2020. Key Words: platelet-rich plasma; PRP; knee osteoarthritis; KOA; knee;osteoarthritis; Arthritis.
2.2 Inclusion and Exclusion Criteria
2.2.1 Inclusion criteria were included
1) double-blind randomized controlled trial of KOA published abroad,2) comparison platelet-rich plasma and other non-surgical treatment, 3) at least one of the following outcome indicators:Western Ontario and McMaster Universities Arthritis Index(WOMAC), Knee Osteoarthritis Outcome Score (KOOS), the visual analogue scale (VAS), and adverse events (AEs),and at least six months follow-up.
2.2.2 Exclusion criteria were included
1) non-randomized controlled studies and retrospective studies,2) duplicate publications and There are obvious errors in data and incomplete relevant data.
2.3 Outcome Measures
The outcome measures will be the Western Ontario and MacMaster Universities Osteoarthritis Index (WOMAC), the visual analogue scale (VAS), Knee Osteoarthritis Outcome Score (KOOS) and Adverse Events (AEs).
2.4 Literature screening and data extraction
Two evaluators independently read the title and abstract of the literature, screened the literature, extracted the data and crosschecked. In case of any disagreement, a third party was requested to help solve it. After excluding obviously irrelevant literature,the full text was further read to determine whether to include the study in the end. Develop a unified data extraction table, extract relevant literature research data, and clarify the basic situation of the research object. Data extraction mainly includes: first author,year, country, study type, grouping method, patient characteristics,imaging classification, number of cases in observation group and control group, follow-up time, outcome indicators and other items. If necessary, contact the author to supplement the data lacking.
2.5 Evaluation of literature methodological quality
Methodological quality was assessed using the Cochrrane Collabation's Risk Bias Assessment Tool [19], which used the following items: application of randomization, implementation of allocation hiding, implementation of the blind method associated with the study, completeness of the outcome data, selective reporting,and the presence of other biases.
2.6 Statistic Analysis
Heterogeneity test and meta-analysis were performed using RevMan 5.3 software. The fixed effect model and random effect model were used to analyze the data. First, statistical heterogeneity analysis was conducted. I2<50% was considered as no statistical heterogeneity or small heterogeneity among studies, and fixed effect model was used to combine data. I2>50% thought that there was some heterogeneity among the studies, and the effect size was combined by the random effects model. If heterogeneity is found,sensitivity analysis or subgroup analysis is performed to determine the source of heterogeneity. If more than 10 studies were included in an outcome indicator, an inverted funnel plot was used to analyze whether there was publication bias. In the study, relative risk (RR)was used as the effect scale for the dicclassification variables. Mean difference (MD) was used for the measurement data with the same unit and measurement method. When the measurement methods were different or the units were inconsistent, standardized mean difference (SMD) was used. At the same time, 95% confidence interval (CI) was given, with P<0.05, indicating that the difference between the two groups was statistically significant [19].
3. Results
3.1 Literature retrieval and screening results
According to the specified search terms, a total of 1786 literatures were searched, among which 838 were repeated references. 763 literatures unrelated to the research topic were excluded from the title abstract, and the remaining 185 literatures were finally included after reading the full text and according to the inclusion and exclusion criteria [20-26]. See Figure 1 for the specific retrieval and screening process. All included studies were double-blind randomized controlled trials, with 250 patients in the treatment(PRP) group and 230 in the control (no PRP) group. All of the studies were conducted between 2015 and 2019, and the age groups included were concentrated between 45 and 65 years old. The imaging K-L grading scale of the included patients was I to IV, and the follow-up time was 6 to 12 months. In the 7 studies, all patients were comparable for gender, age, BMI, and sample size at baseline,with P>0.05. See Table 1 for details.

Figure 1 Flow chart of literature search and screening
3.2 Literature quality and bias risk assessment of included studies
All included studies were double- blind randomized in design according to the CochraneCollaboration “Risk of bias”[19]. Theincomplete outcome data was reported in the one study resultin in a high risk bias20. Selective and other biases were described in the studies by Yu et al, Nayanaet al, Four studies lost some patients during follow-up [20,21,24,26]. In general, all the 7 trials included were of good quality, and the results of methodological processes are shown in Figure 2,3.
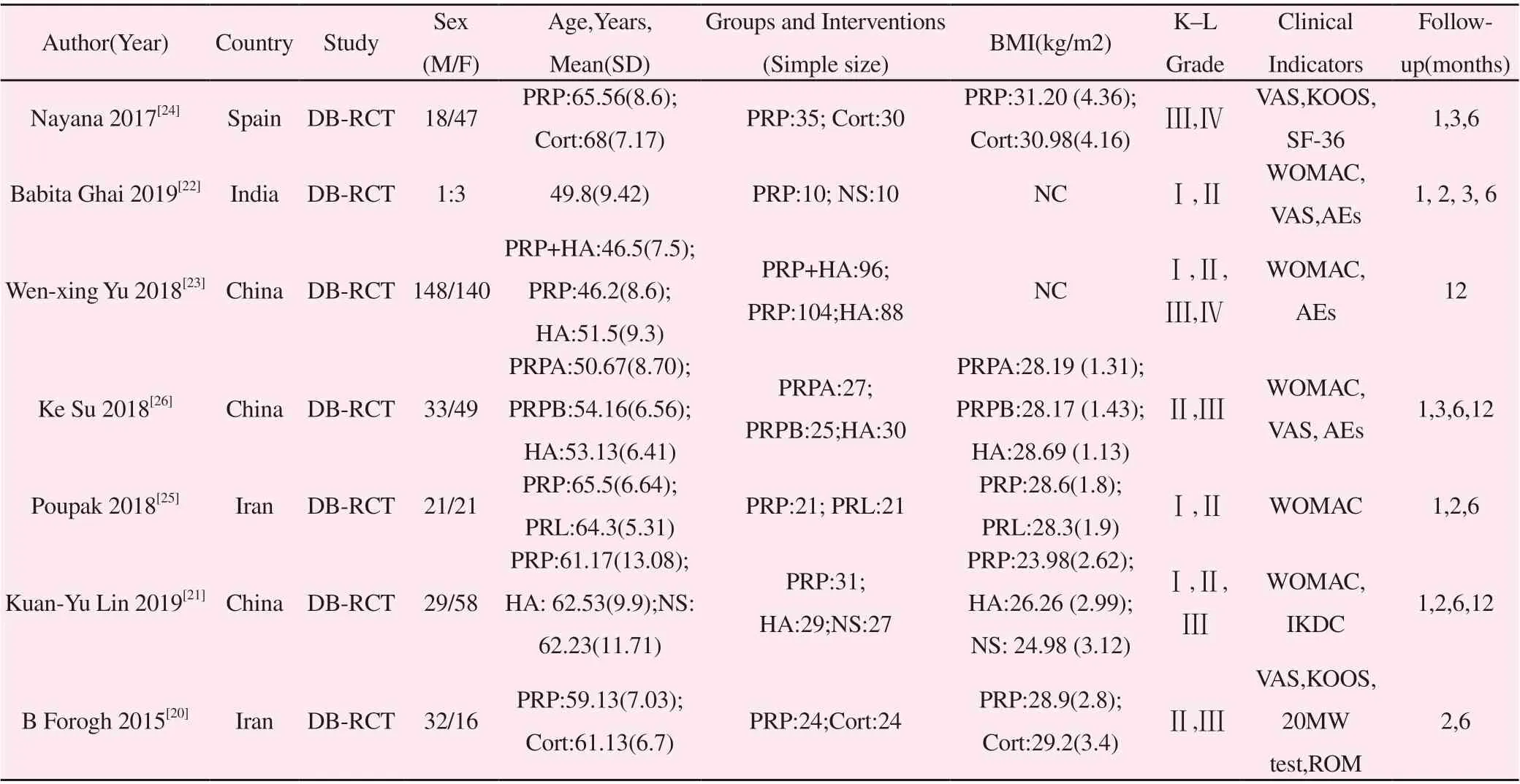
Table 1 The basic characteristics of the study

Figure 2 Risk of bias assessment of the study

Figure 3 Risk of bias summary of the study
3.3 Outcomes of the meta-analysis
3.3.1 WOMAC scores at the 6-months follow-up
A total of 4 studies[21,22,25,26] reported WOMAC Total scores at 6 month after treatment. Theheterogeneity test indicated a high degree of homogeneity (I2=86%, MD: 9.63, 95% CI: 3.29 to15.96, P=0.003<0.05), A randomed-effects model was used for meta analysis; Three studies[22,25,26]respectively reported Physical function, Stiffness, Pain of WOMAC scores at 6 months aftertreatment. The pooled analysis showed that the subjects in the PRP and no PRP groups exhibitedsimilar Stiffness after treatment(I2=92%, MD: 1.26, 95% CI: 0.02 to 2.50, P=0.05). However,thePhysical function recovery and Pain relief in the PRP group performed better than those in the no PRP group (I2=98%, MD:12.03, 95% CI: 0.60 to 23.45, P=0.04) and (I2=92%, MD: 2.90,95% CI: 0.60 to 5.20, P=0.01). (Fig. 4).
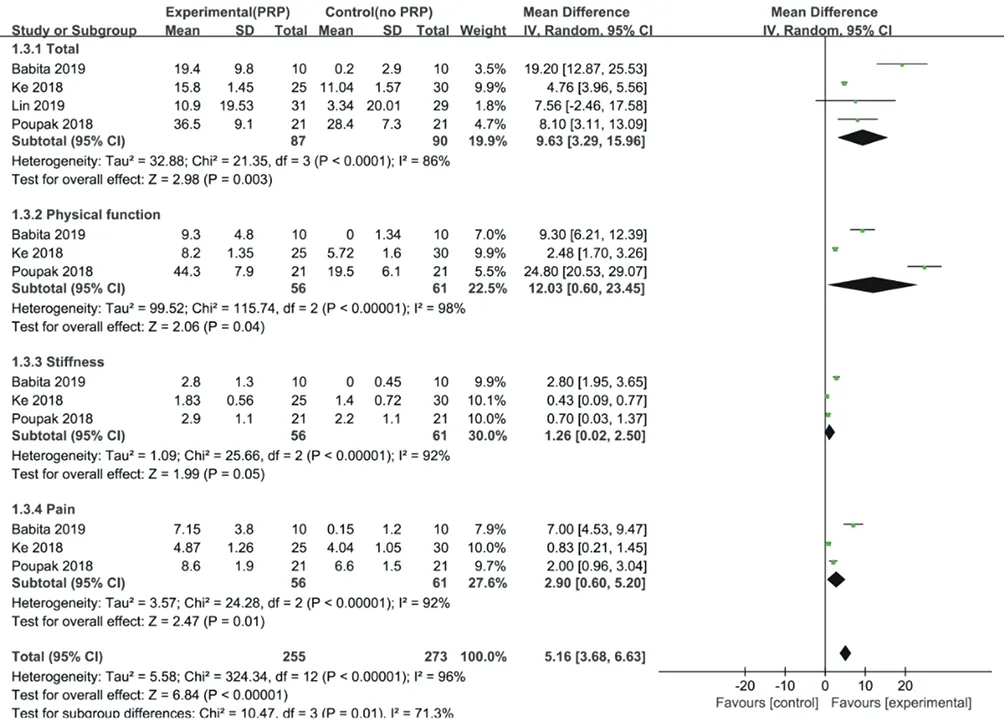
Figure 4 Forest plot of WOMAC score comparison between PRP and other drugs in KOA at 6 months follow-up
3.3.2 WOMAC scores at the 12-months follow-upA total of 3 studies[21,23,26] reported comparisons of the WOMAC scores at 12 months after treatment.The heterogeneity test indicated that the homogeneity was low (I2<50%), and a fixed-effects model was used for meta-analysis. The subgroup analysis results indicated that patients in the PRP group showed better than those of the group receiving no PRP at WOMAC Total scores(I2=0%, MD: 3.85, 95%CI: 2.66 to 5.04, P<0.05), Physical function recovery(I2=0%, MD:3.28, 95% CI: 2.13 to 4.43, P<0.05), Stiffness(I2=17%, MD: 0.52,95% CI: 0.24 to 0.79, P<0.05) , and Pain relief(I2=0%, MD: 0.86,95% CI: 0.33 to 1.39, P<0.05) after treatment. (Fig. 5).
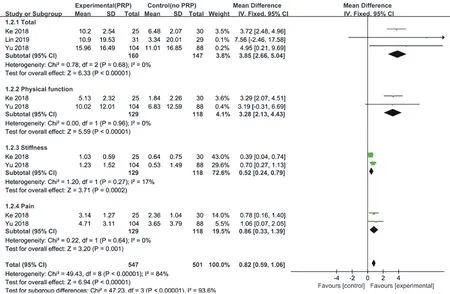
Figure 5 Forest plot of WOMAC score comparison between PRP and other drugs in KOA at 12 months follow-up
3.3.3 VAS scores
Four studies[20,22,24,26] reported the Visual Analogue Scales(VAS) scores at 3, 6 months aftertreatment. The heterogeneity test suggested a high degree of homogeneity (I2>50%), and a random effects model was used for meta analysis. We can find that VAS scores in the PRP group showedsignificant difference than no PRP group at 3 months(SMD=0.88; 95% CI: 0.13 to 1.62; P<0.05), 6 months(SMD=0.85; 95% CI: 0.11 to 1.59; P<0.05). (Fig. 6).
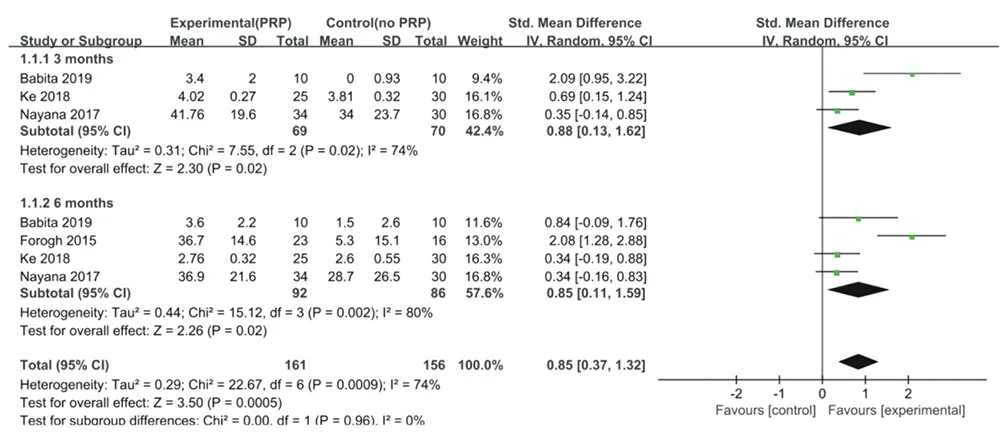
Figure 6 Forest plot of VAS score comparison between PRP and other drugs in KOA at 3 and 6 months follow-up
3.3.4 KOOS scores at the 6-months follow-up
Two studies[20,24] reported Pain, Symptoms, Quality of life,Sport, Function of the Knee OsteoarthritisOutcome Score(KOOS)at 6 months after treatment. The heterogeneity test suggested a high degreeof homogeneity (I2>50%), and a random-effects model was used for meta-analysis. A subgroupanalysis was performed to compare the scores based on the different aspects of KOOS. The analysisresults showed that there is no significant differences in the PRP group comparing with no PRP at Pain (I2=90%, MD: 18.74,95% CI: -3.60 to 41.08, P=0.10), Symptoms (I2=92%, MD: 8.60,95% CI: -11.58 to 28.78, P=0.40), and Sport(I2=69%, MD: 2.89,95% CI: -6.33 to 12.11, P=0.54).However, the treatment in the PRP groups indicated better efficacy than those in the no PRP groups at Quality of life improvment (I2=0%, MD: 12.06, 95% CI: 6.15 to 17.96, P<0.05) , and Function recovery (I2=0%, MD: 8.63, 95% CI:0.85 to 16.42, P=0.03) after treatment. (Fig. 7).
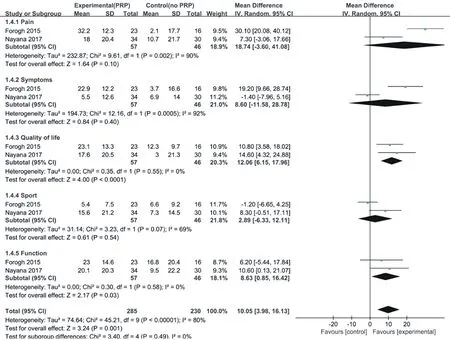
Figure 7 Forest plot of KOOS score comparison between PRP and other drugs in KOA at 6 months follow-up
3.3.5 Adverse EventsAdverse Events(AEs) was reported in three studies[22,23,26] based on the length of follow-up. Theheterogeneity test showed that the homogeneity was a low degree (I2=38%), and a fixed-effectsmodel was used for meta-analysis. The analysis results did not reveal significant difference betweenPRP compared with no PRP (RR:0.96, 95% CI: 0.65 to 1.40, P=0.82). (Fig. 8)

Figure 8 Forest plot of adverse events in PRP versus other medications for treating KOA
4. Discussion
KOA is a chronic bone and joint disease caused by a variety of pathogenic factors, mainly characterized by cartilage degeneration and bone hyperplasia, which has serious adverse effects on society and economy, especially on patients' quality of life [27]. Its main symptoms are joint pain, swelling and dysfunction, making it the most common degenerative disease among the elderly. At the same time, with the increase of age, weight, activity and trauma,the incidence of KOA also increases year by year [28].However,the pathogenesis and pathological mechanism of KOA has not been clarified at present, and some studies have shown that the proliferation and degeneration of articular cartilage and the reduction of chondrocytes may be the main cause of KOA. Other studies have found that the dynamic balance between articular cartilage injury and repair is affected by the expression of inflammatory cytokines including IL-1 and TNF [29]. Therefore, how to reduce the number of relevant inflammatory factors and maintain the balance between the destruction and repair mechanism of articular cartilage has become a research hotspot. In addition, the clinical treatment of KOA aims to improve the patient's quality of life by reducing pain and improving joint function. At present, non-surgical therapy can relieve various symptoms of early KOA and improve the quality of life of patients,which is recognized and supported by doctors [30].However, we still face many problems. Some studies [31-32] suggest that nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen and intraarticular corticosteroids should be used as initial treatment for mild to moderate KOA, but their use is limited by their potential toxicity and side effects and failure to delay degeneration of articular cartilage. Therefore, the current treatment approach for KOA still focuses on the early application of multiple interventions to delay joint structural damage.
PRP is a high concentration of platelets from the patient itself,which contains a large number of growth factors, including transforming growth factor β(TGF-β), platelet-derived growth factor (PDGF) and fibroblast growth factor (FGF), which can produce a large number of collagen fibers and promote cell proliferation, differentiation and repair of damaged tissues, especially damaged cartilage. In addition, it causes little damage to the human body and can avoid inflammatory reaction or blood infection, which is one of the main advantages of the new biotherapy for PATIENTS with KOA in recent years [29,33-35].Several studies [36-37] have found that PRP is a safe and effective alternative treatment that can relieve pain, improve function and reduce degradation of articular cartilage in PATIENTS with KOA, especially with better clinical outcomes at longer follow-up periods. However, PRP treatment remains controversial, with several in vivo and in vitro studies reporting adverse events in the PRP group, including vomiting, swelling,reduced function, and increased pain. In addition, PRP injection dose, time, frequency and technique may be different for patients at different stages of cartilage degeneration [38]. Therefore, it is difficult to confirm the effectiveness and safety of this method in alleviating pain and improving function of patients at different stages, especially for severe elderly KOA patients, and it still needs to be verified.This study conducted a high-quality systematic evaluation of the efficacy and safety of PRP injection therapy compared with other treatments for the level of pain and functional improvement in patients with KOA. Data for our study were reported from seven double-blind randomized controlled trials comparing pain relief and improvement in function at 3, 6, and 12 months of follow-up in the PRP versus non-PRP groups. Primary outcome measures were WOMAC(total score, pain, function, stiffness, swelling), VAS score,and secondary outcome measures were KOOS(pain, symptoms,quality of life, movement, function) and AEs. The results of this meta-analysis and subgroup analysis showed significant differences between PRP injection and other conservative treatments at 6 and 12 months with respect to WOMAC total score, pain, function, and swelling. In terms of VAS score reduction, patients in PRP group had significant pain relief at 3 and 6 months, indicating that PRP treatment has a positive effect on alleviating pain and improving physical function. In addition, there was no significant difference in KOOS(pain, symptoms, movement) after 6 months. However,at 6 months, the PRP group was significantly better at improving quality of life and function than the other conservative groups.Nayana et al. [24] conducted a prospective double-blind randomized clinical trial to study the symptoms of PRP injection in the treatment of knee osteoarthritis, and the results showed that PRP treatment could significantly relieve the pain of advanced knee osteoarthritis and improve the daily living activities and quality of life of patients,compared with corticosteroid treatment. It was proved that PRP injection improved knee function more effectively than other PRP injection. In addition, Poupak et al. reviewed the effects of intraarticular injection of PRP or bloodletting therapy (PRL) on KOA pain score and function. The results showed a significant decrease in total WOMAC scores in patients treated with PRP or PRL. Moreover, PRP injection is more effective than PRL in treating KOA. In another 2019 study by Babita et al. [22], 20 patients who received PRP injection or saline injection showed a significant reduction in knee stiffness and improved mobility in the PRP group at the end of the 6-month follow-up. All of the studies we included in this systematic review were double-blind, randomized clinical trials with good quality assessments, suggesting that the results of the analyses are more reliable.
Most of the previous basic studies have proved the effectiveness of PRP and revealed the mechanism of PRP in treating KOA.Injection of PRP can provide adequate nutrition to cartilage and avoid inflammatory response without increasing the risk of infection,and has been proven to be effective and safe [39]. In addition, other studies [40] have shown that the role of PRP in the treatment of KOA benefits from different biological mechanisms and the activity of signal molecules. PRP treatment can improve the viscoelasticity of synovial fluid, reduce inflammatory response and promote the production of growth factors. Although many studies have confirmed that PRP plays an important role in cartilage synthesis and metabolism through various factors. We still need a lot of time and a lot of research to discover the specific mechanism by which PRP improves chondrocyte function. Several previous systematic reviews have suggested that the effectiveness of PRP in PATIENTS with KOA, heterogeneity may be caused by a number of objective factors,including sample size, injection dose, degree of joint degeneration (I to ⅳ), and interventions, all of which contribute to varying degrees of heterogeneity and different clinical responses [41]. Therefore,in this study, we included all available high-quality double-blind randomized trials on the efficacy of PRP in the treatment of KOA,excluding all trials with inappropriate selection strategies, in order to ensure more reliable conclusions for the best clinical evidence.
The advantage of this study is that it is the first systematic evaluation of the high quality efficacy of PRP on pain and functional levels in PATIENTS with KOA. All trials included were randomized,double-blind and had a good quality assessment. It is clear from the results that PRP is a more effective treatment for KOA than other conservative treatments, which could help provide guidance for clinical application. However, this meta-analysis still has limitations. Different injection dose, follow-up period, and degree of degeneration may affect the results and degree of heterogeneity.In addition, only 7 literatures were included and the sample size was too small to objectively evaluate the methodological quality. The lack of funnel plots limits the bias risk outcome, which may increase heterogeneity and influence our conclusions.
Taken together, the results of this systematic review and metaanalysis showed that PRP injection significantly improved WOMAC and VAS scores at 3, 6, and 12 months, and significantly improved KOOS(quality of life and function) at 6 months, compared with other conservative treatments. However, PRP injection has no clinical prognostic advantage in terms of the incidence of adverse events.Overall, PRP injections appear to be superior to other nonsurgical treatments in reducing pain and improving KOA function.
Author's contribution
Xie Rong was responsible for the design, implementation, data analysis and interpretation of the study, as well as the writing and revision of the final paper.
Zhu Liguo and Wang Shangquan are responsible for guiding the research topic selection and providing research funding support.
Wei Xu and Yu Jie are responsible for reviewing the content of the article and providing administrative support.
Linghui Li and Jiawen Zhan were responsible for providing technical support and guidance during the implementation of the study.
Xie Rui and Chang Xiaojuan participated in data collection and analysis.
杂志排行
Journal of Hainan Medical College的其它文章
- Study on prescription and medication rules of Hua Baojin for treatment of colorectal cancer based on data mining
- Molecular mechanism of treatment of pneumonia in children with Mori cortex - Lycii cortex based on network pharmacology
- Analysis of risk factors and establishment of predictive model for elevated ALT in adult patients with nonalcoholic fatty liver disease
- Mechanism of Resveratrol on autophagy mediated by Mst1/Sirt3 signaling pathway in diabetic cardiomyopathy
- Effect of synoviectomy combined with postoperative radiotherapy on pigmented villonodular synovitis in knee: A meta-analysis
- Identification and analysis of core target genes of miR-29b-3p in glioma
