Prevalence of hypothyroidism and effect of thyroid hormone replacement therapy in patients with non-alcoholic fatty liver disease:A population-based study
2022-04-02AshrafAlmomaniAsifAliHitawalaPrabhatKumarSuraAlqaisiDanaAlshaikhMotasemAlkhayyatImadAsaad
Ashraf Almomani,Asif Ali Hitawala,Prabhat Kumar,Sura Alqaisi,Dana Alshaikh,Motasem Alkhayyat,Imad Asaad
Ashraf Almomani,Prabhat Kumar,Sura Alqaisi,Motasem Alkhayyat,Department ofInternal Medicine,Cleveland Clinic Foundation,Cleveland,OH 44111,United States
Asif Ali Hitawala,Liver Disease Branch,National Institute of Diabetes and Digestive and Kidney Diseases/National Institutes of Health,Bethesda,MD 20892,United States
Dana Alshaikh,Mutah University,Amman 00962,Jordan
lmad Asaad,Department of Digestive Disease and Surgery Institute,Cleveland Clinic Foundation,Cleveland,OH 44195,United States
Abstract BACKGROUND Non-alcoholic fatty liver disease(NAFLD)is currently considered as the most common cause of chronic liver disease worldwide.Risk factors for NAFLD have been well-described,including obesity,type 2 diabetes mellites(T2DM),dyslipidemia(DLP)and metabolic syndrome.Hypothyroidism has been identified as an independent risk factor for the development of NAFLD,although the literature is inconsistent AIM To evaluate the prevalence of hypothyroidism in patients with NAFLD,assess if it is an independent risk factor and explore the effect of thyroxine replacement therapy.METHODS Our cohort’s data was obtained using a validated,large,multicenter database(Explorys Inc,Cleveland,OH,United States)aggregated from pooled outpatient and inpatient records of 26 different healthcare systems,consisting of a total of 360 hospitals in the United States,and utilizing Systematized Nomenclature of Medicine-Clinical Terms for coding.We evaluated a cohort of patients with hypothyroidism and NAFLD.Multivariate analysis was performed to adjust for confounding risk factors including hypertension(HTN),T2DM,DLP,obesity and metabolic syndrome.SPSS version 25,IBM Corp was used for statistical analysis,and for all analyses,a 2-sided P value of < 0.05 was considered statistically significant.Exclusion criteria were limited to age < 18 years.RESULTS Among the 37648180 included individuals in this database who are above the age of 18 years,there were a total of 2320 patients with NAFLD(6.16 per 100000)in the last five years(2015-2020),amongst which 520 patients(22.4%)had hypothyroidism.Baseline characteristics of patients in this database are described in Table 1.Patients with NAFLD were also more likely to have obesity,T2DM,DLP,HTN,and metabolic syndrome(Table 2).While males and females were equally affected,patients in the age group 18-65 years as well as Caucasians seem to be at a higher risk.There was an increased risk of NAFLD among patients with hypothyroidism(OR=1.587).Furthermore,thyroid hormone replacement was not associated with a decreased risk for developing NAFLD(OR=1.106,C=0.952-1.285,P=0.303).CONCLUSION Hypothyroidism seems to be an independent risk factor for the development of NAFLD.Thyroid hormone replacement did not provide a statistically significant risk reduction.Further studies are needed to evaluate the effect of thyroid hormone replacement and assess if being euthyroid while on thyroid replacement therapy affects development and/or progression of NAFLD.
Key Words:Hypothyroidism;Non-alcoholic fatty liver disease;Thyroid hormone replacement therapy;Independent risk factor
lNTRODUCTlON
Non-alcoholic fatty liver disease(NAFLD)is currently considered as the most common cause of chronic liver disease worldwide and the second most common indication for liver transplantation in the United States after chronic hepatitis C with a histological disease spectrum ranging from steatosis to nonalcoholic steatohepatitis(NASH)and eventually cirrhosis.Its international prevalence is steadily increasing(15% in 2005 to 25% in 2010),and it is expected to emerge as the leading cause of end-stage liver disease in the near future[1].Several genetic and environmental risk factors for NAFLD have been described in the literature,including obesity,unhealthy eating habits,low physical activity levels,type 2 diabetes mellitus(T2DM),dyslipidemia(DLP),hypertension(HTN)and metabolic syndrome[1-3].
Thyroid hormone plays a major role in regulating the metabolism of lipids and carbohydrates which are affected in patients with NAFLD.Furthermore,hypothyroidism in particular shares similar risk factors to those of NAFLD including insulin resistance,DLP,obesity and metabolic syndrome[4,5].Liangpunsakulet al[4]was the first to describe the potential relationship between hypothyroidism and NAFLD,and found a significantly higher hypothyroidism prevalence among patients with NAFLD.This association was further replicated in later retrospective studies[5].However,these studies were limited by the smaller sample size and the inconsistency of the literature to some degree.Our aim is to conduct a population-based study to estimate the prevalence of hypothyroidism in patients with NAFLD,and statistically adjust for all known confounders to assess whether hypothyroidism is an independent risk factor for NAFLD,and to further assess the effect of thyroid hormone replacement therapy.
MATERlALS AND METHODS
Database
Our cohort’s data was obtained using a validated,multicentered and daily-updated database(Explorys Inc,Cleveland,OH,United States)developed by IBM Corporation,Watson Health[6].Explorys consists of electronic health records of 26 different healthcare systems across the United States and a total of 360 hospitals with more than 50 million patients.Explorys utilizes Systematized Nomenclature of Medicine Clinical Terms(SNOMED-CT)for the definition of the diseases and pools large outpatient and inpatient daintified data that can be formulated into numerous cohorts according to the clinical element being studied.Explorys further allows for the identification of the timeline of events in reference to the index clinical event of interest,and hence the ability to study the temporal relationship between different variables.The Institutional Review Board approval is not required since Explorys is a Health Insurance Portability and Accountability Act-compliant platform.
Methodology and patient selection
We retrospectively evaluated an initial cohort of patients with a SNOMED-CT of “Hypothyroidism”between the years 2015 to 2020.Our exclusion criteria were limited to patients less than 18 years old.Baseline characteristics of patients with hypothyroidism are shown in Table 1.A second cohort of patients with a SNOMED-CT of “Non-Alcoholic Fatty Liver” was identified.Age,gender and racebased data were collected.Potential confounders that were analyzed included:hypothyroidism,HTN,T2DM,DLP,obesity and metabolic syndrome.Among those with hypothyroidism,weather the patient was on thyroxine replacement therapy was also analyzed.
Statistical analysis
Demographics and related diseases were characterized by descriptive statistics.The overall prevalence of NAFLD was calculated by dividing the total number of individuals with NAFLD by the total number of individuals in the database(2015-2020),hence making sure that all patients in the denominator had an equal opportunity of being diagnosed with NAFLD.Multivariate analysis was performed to adjust for the confounders in the later cohort(Table 2).SPSS version 25,IBM Corp was used for statistical analysis,and for all analyses,a 2-sidedPvalue of < 0.05 was considered statistically significant.
RESULTS
Baseline characteristics of patients in this database are described in Table 1.Among the 37648180 included individuals in this database who are above the age of 18 years,there were a total of 2320 patients with NAFLD in the period from 2015 to 2020.The 5-year period prevalence rate of NAFLD was 6.16 per 100000.Amongst those with NAFLD,520 patients(22.4%)had hypothyroidism.Patients with NAFLD were also more likely to have obesity(OR,3.616,95%CI:3.318-3.940),type 2 diabetes mellitus(OR,2.178,95%CI:1.994-2.379),dyslipidemia(OR,2.346,95%CI:2.121-2.596),hypertension(OR,1.326,95%CI:1.201-1.465),and metabolic syndrome(OR,4.782,95%CI:4.782-5.460)(Table 2).Males(OR,1.008,95%CI:0.934-1.088)and females were equally affected,but the results were statistically insignificant.Patients in the age group 18-65 years(OR,1.658,95%CI:1.524-1.804)as well as Caucasians(OR,1.63,95%CI:1.489-1.799)seem to be at a higher risk.There was an increased risk of NAFLD among patients with hypothyroidism(OR,1.587,95%CI:1.388-1.815).Furthermore,thyroid hormone replacement was not associated with a decreased risk for developing NAFLD(OR,1.106,95%CI:0.952-1.285,P=0.303).Characteristics of patients with NAFLD and hypothyroidism are shown in Figure 1.
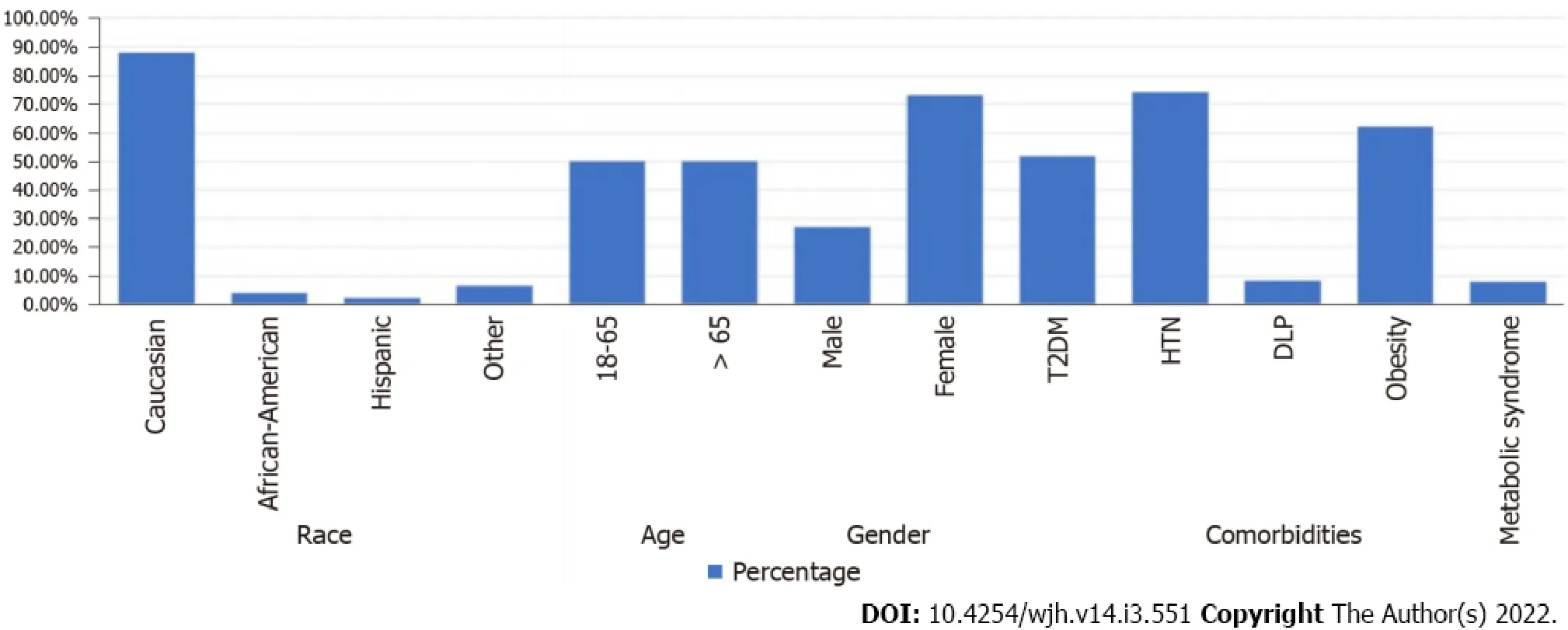
Figure 1 Characteristics of patients with non-alcoholic fatty liver disease and hypothyroidism.HTN:Hypertension;T2DM:Type 2 diabetes mellitus;DLP:Dyslipidemia.

Table 1 Baseline characteristics of patients with hypothyroidism in explorys database

Table 2 Multivariate analysis for risk factors in individuals with non-alcoholic fatty liver disease
DlSCUSSlON
Discussion and review of literature
Over the last couple of decades,NAFLD has emerged as one of the most common causes of chronic liver disease,including cryptogenic cirrhosis across the globe[7-9].Risk stratification for NAFLD has become a focus of research because of the close relationship with different metabolic syndromes like T2DM,DLP,obesity,polycystic ovarian syndrome,and thyroid disorders.Albeit the overlap of complex metabolic pathophysiology of NAFLD and thyroid function remains controversial,many studies have suggested a strong association between the two[10-12].
The underlying pathophysiological mechanism of NAFLD has not been well explained.Still,the most commonly accepted theory implicates insulin resistance as the central role in developing hepatic steatosis and perhaps steatohepatitis[13,14].Thyroid hormone has a vital role in cell metabolism and energy hemostasis.Thyroid dysfunction is associated with many diseases,for instance,cardiovascular disease,obesity,dementia,fracture,and recently NAFLD[15].Thyroid hormones impact various metabolic pathways,and evidence corroborates the association of thyroid dysfunction and thepathogenesis of NAFLD.The two most telltale signs of the NAFLD disease spectrum are insulin resistance and hepatic lipid dysregulation[16].Thyroid hormones(T3 and T4)use intracellular receptor signaling pathways in the liver to induce lipid metabolism.Even though molecular pathways leading to insulin resistance are complex and have not been completely elucidated,the association between thyroid dysfunction,both overt and subclinical hypothyroidism,and NAFLD has been extensively reported.
For example,a population-based study by Chunget al[12]showed that the prevalence of NAFLD and elevated liver enzymes were higher in a patient with hypothyroidism(OR:1.38;95%CI:1.17-1.62)and confirmed a relevant dose-dependent clinal relationship between NAFLD and thyroid hormones.Moreover,thyroid hormones level has been shown to exert an effect in all the spectrum of steatosis.For instance,the exciting case-control comparative study by Pagadalaet al[5]for the prevalence of hypothyroidism in NAFLD and NASH showed that hypothyroidism was more common in patients with NASH than patients with NAFLD(25%vs12.8%,P=0.03).
Another study from the western region of India by Parikhet al[17]reported a prevalence of 16.8%hypothyroidism in NAFLD patients with a strong clinically significant association amongst two diseases(OR,14.94,95%CI:3.5-62.6).Authors also concluded that steatohepatitis was found to be more common in hypothyroid individuals as compared to controls(OR 3.9,95%CI:1.2-11.1).Ludwiget al[18]did a population-based cross-sectional study of 1276 participants which showed an increased prevalence of hepatic steatosis in subjects with reduced thyroid hormones(P=0.0143;P≤ 0.0001).
Since hypothyroidism and NAFLD share numerous characteristics,including weight gain,whether hypothyroidism is a risk factor for NAFLD remains difficult to answer in retrospective studies(AA1).To provide stronger evidence of the causality relationship,Banoet al[19]conducted a prospective cohort study of 9419 patients followed over ten years and observed the effects of hypothyroidism in NAFLD patients,and found a 1.24-fold higher NAFLD risk(95%CI:1.01-1.53)in patients with hypothyroidism.Another recent descriptive cross-sectional study by Martínez-Escudéet al[20]reported a significantly higher prevalence of NAFLD and liver fibrosis in subjects with TSH ≥ 2.5(μIU/mL).Also,in a comparative study of 1773 euthyroid participants,both TSH and levels Free T3 Level were found to be positively associated with the risk of NAFLD when diagnosed by ultrasound and fatty liver index,respectively[21].Finally,a recent metanalysis found that overall hypothyroidism has a positive association with the risk of NAFLD[22].
Along with these well-crafted studies,some substantial evidences have questioned the exact association between NAFLD and thyroid regulation.A recent Spanish study reported no association between hypothyroidism and NAFLD[23].The authors observed that thyroid hormone level was not associated with a higher prevalence of NAFLD.Similarly,in a study by Leeet al[23],the authors found no relationship of increased incidence of NAFLD in patients with the subclinical or overt types of hypothyroidism.
Many of the studies describing the relationship between these two entities were largely limited by the sample size.To fill this gap,we conducted one of the largest nationwide multicenter studies which screened 37648180 individuals,among which 520 individuals had concomitant NAFLD and hypothyroidism.Our retrospective cohort study has shown that hypothyroidism is an independent risk factor for NAFLD,and that about 1 in every 5 patients with NAFLD have concomitant hypothyroidism(22.4%).Overall,this is one of the highest prevalence rates for NAFLD in hypothyroidism patients.Secondly,the effect of thyroid hormone replacement in hypothyroidism patients and its effect on NAFLD prevention has not been well explored.In a post hoc analysis of a randomized controlled trial for patients with subclinical hypothyroidism,the prevalence of NAFLD was reduced from 48.5% to 24.2%(P=0.041)after 15 mo of thyroid hormone replacement,whereas the prevalence of NAFLD remained stable in the untreated group[24],however;this trial was limited by the small sample size of~360 patients(AA2).Moreover,those who received thyroid hormone replacement therapy had higher weight loss,which can itself explain the prevalence change in the treated population.Our study failed to show a statistically significant NAFLD risk reduction among patients with hypothyroidism who are placed on thyroid hormone replacement(OR,1.106,95%CI:0.952-1.285,P=0.303)but the weight changes were difficult to assess.Without adequately powered prospective trials that also adjusts for weight changes,the question whether thyroid hormone replacement has a direct protective effect against NAFLD remains difficult to answer,and the appropriate duration for effective replacement therapy and the goals of treatment remain unclear(AA3).
Limitations
One of the limitations in our study is that we could not analyze the diagnostic method used for assessing NAFLD and set cut-off values for diagnosing hypothyroidism,since these are SNOMED-CT coded diagnoses on identified patient’s charts.We also could not specify the exact degree at which hypothyroidism becomes a NAFLD risk factor(AA4).Also,we could not evaluate for how long have these patients with hypothyroidism been on thyroid hormone replacement therapy,and whether they have achieved the euthyroid state or not.More prospective trials are needed to answer this question.
CONCLUSlON
Hypothyroidism seems to be an independent risk factor for the development of NAFLD demonstrated in retrospective and prospective studies.Some studies have suggested that thyroid hormone replacement can potentially prevent or reverse NAFLD,which is potentially caused by weight loss.However,our study showed that thyroid hormone replacement did not provide a statistically significant risk reduction.Further prospective studies are needed to assess the role of thyroid hormone replacement therapy in patients with NAFLD,the duration for effective treatment and the treatment goals.
ARTlCLE HlGHLlGHTS
Research background
Non-alcoholic fatty liver disease(NAFLD)is the most common cause of chronic liver disease worldwide,and hypothyroidism has been identified as an independent risk factor.The available data are limited by small sample size and the effect of thyroid hormone replacement therapy is not well studied.
Research motivation
The main topics of this article is to give a focused analysis on the hypothyroidism and to assess whether it is an independent risk factor for the development of NAFLD by filling the small sample size gap in the literature,provide a review of the current medical literature in this field,and -most importantly- to evaluate the role of thyroid hormone replacement therapy in the prevention of the disease.
Research objectives
The objective of this case control study is to assess whether hypothyroidism is an independent risk factor for the development of NAFLD,to review the updated medical literature,and to assess the role of thyroid hormone replacement therapy in the prevention of the disease.
Research methods
We used a validated multicenter database(Explorys Inc.)from pooled outpatient and inpatient records of 26 different healthcare systems,consisting of a total of 360 hospitals in the United States to collect our data.We evaluated a cohort of patients with hypothyroidism and NAFLD.Multivariate analysis was performed to adjust for confounding risk factors including hypertension(HTN),type 2 diabetes mellites(T2DM),dyslipidemia(DLP),obesity and metabolic syndrome.We evaluated a cohort of patients with hypothyroidism and NAFLD.Multivariate analysis was performed to adjust for confounding risk factors including HTN,T2DM,DLP,obesity and metabolic syndrome.
Research results
Among 37648180 in the database who are above the age of 18 years,a total of 2320 patients with NAFLD in the period from 2015 to 2020 were included.NAFLD prevalence was 6.16 per 100000,among which 520 patients(22.4%)had hypothyroidism.Patients with NAFLD were also more likely to have obesity,type 2 diabetes mellitus,dyslipidemia,hypertension,and metabolic syndrome.Males and females were equally affected,but the results were statistically insignificant.Patients in the age group 18-65 years as well as Caucasians seem to be at a higher risk.There was an independent increase in the risk of NAFLD among patients with hypothyroidism,and thyroid hormone replacement was not associated with a decreased risk for developing NAFLD.Prospective studies are needed to better delineate the role of thyroid hormone replacement therapy in these individual.
Research conclusions
There was an independent increase in the risk of NAFLD among patients with hypothyroidism,and thyroid hormone replacement is not associated with a decreased risk for developing NAFLD.Other studies have shown a potential protective effect of thyroid hormone replacement therapy.Based on the conflicting results with the existing literature,further studies are needed to better investigate the relationship between thyroid hormone replacement therapy and NAFLD.
Research perspectives
Future research should focus on assessing the degree of hypothyroidism that leads to NAFLD,and the role of thyroid hormone replacement therapy including the duration of treatment and the end-point goals.
FOOTNOTES
Author contributions:Almomani A and Kumar P wrote the manuscript;Hitawala AA designed the study;Alkhayyat M performed the statistical analysis;Alqaisi S,Alshaikh D collected the data;Asaad I is the corresponding author.
lnstitutional review board statement:No Institutional Review Board approval was required for this study since the database is de-identified.
Conflict-of-interest statement:No conflict of interest.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See:https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:United States
ORClD number:Ashraf Almomani 0000-0003-1648-0005;Asif Ali Hitawala 0000-0002-2888-0172;Prabhat Kumar 0000-0001-9768-4223;Sura Alqaisi 0000-0001-6548-8498;Dana Alshaikh 0000-0003-1471-0647;Motasem Alkhayyat 0000-0002-7603-8705;Imad Asaad 0000-0002-0648-6625.
Corresponding Author's Membership in Professional Societies:American College of Gastroenterology;American Association for the Study of Liver Diseases.
S-Editor:Zhang H
L-Editor:A
P-Editor:Zhang H
杂志排行
World Journal of Hepatology的其它文章
- Hepatitis E in immunocompromised individuals
- Small duct primary sclerosing cholangitis:A discrete variant or a bridge to large duct disease,a practical review
- New progress in understanding roles of nitric oxide during hepatic ischemia-reperfusion injury
- Renal manifestations of hepatitis E among immunocompetent and solid organ transplant recipients
- Safety of direct acting antiviral treatment for hepatitis C in oncologic setting:A clinical experience and a literature review
- Fertaric acid amends bisphenol A-induced toxicity,DNA breakdown,and histopathological changes in the liver,kidney,and testis