Peroral endoscopic longer vs shorter esophageal myotomy for achalasia treatment:A systematic review and meta-analysis
2022-04-01ChunYanWengChengHaiHeMingYangZhuangJingLiXuBinLyu
Chun-Yan Weng,Cheng-Hai He,Ming-Yang Zhuang,Jing-Li Xu,Bin Lyu
Chun-Yan Weng,Department of Gastroenterology,The First Clinical Medical College of Zhejiang Chinese Medical University,Hangzhou 310053,Zhejiang Province,China
Cheng-Hai He,Department of Gastroenterology,The Affiliated Hospital of Hangzhou Normal University,Hangzhou 310006,Zhejiang Province,China
Ming-Yang Zhuang,Internal Medicine of Chinese Medicine,The First Clinical Medical College of Zhejiang Chinese Medical University,Hangzhou 310053,Zhejiang Province,China
Jing-Li Xu,Department of Surgery,The First Clinical Medical College of Zhejiang Chinese Medical University,Hangzhou 310053,Zhejiang Province,China
Bin Lyu,Department of Gastroenterology,The First Affiliated Hospital of Zhejiang Chinese Medicine University,Hangzhou 310006,Zhejiang Province,China
Abstract BACKGROUND Peroral endoscopic myotomy(POEM)has been demonstrated to be safe and effective in the treatment of achalasia.Longer myotomy is the standard POEM procedure for achalasia but when compared with shorter myotomy,its effectiveness is not as well known.AIM To compare the clinical effectiveness of longer and shorter myotomy.METHODS PubMed,EmBase,Cochrane Library,web of science and clinicaltrials.gov were queried for studies comparing shorter and longer POEM for achalasia treatment.The primary outcome was clinical success rate.Secondary outcomes comprised of operative time,adverse events(AEs)rate,gastroesophageal reflux disease(GERD)and procedure-related parameters.The Mantel-Haenszel fixed-effects model was primarily used for the analysis.Publication bias was assessed.RESULTS Six studies were included in this analysis with a total of 514 participants.During the follow-up period of 1-28.7 mo,longer and shorter myotomy in treating achalasia showed similar excellent effectiveness[overall clinical success(OR = 1,95%CI:0.46-2.17,P = 1,I2:0%;subgroup of abstract(OR = 1.19,95%CI:0.38 to 3.73;P = 0.76;I2:0%);subgroup of full text(OR = 0.86 95%CI:0.30 to 2.49;P = 0.78;I2:0%)].Shorter myotomy had significantly reduced mean operative time compared with the longer procedure.There were no statistically significant differences in AEs rates,including GERD(overall OR = 1.21,95%CI:0.76-1.91;P = 0.42;I2:9%;subgroup of abstract OR = 0.77,95%CI:0.40-1.47;P = 0.43;I2:0%;subgroup of full text OR = 1.91,95%CI:0.98-3.75;P = 0.06;I2:0%),hospital stay(overall MD = -0.07,95%CI:-0.30 to 0.16;P = 0.55;I2:24%;subgroup of abstract MD = 0.20,95%CI:-0.25 to 0.65;P = 0.39;I2:0;subgroup of full text MD = -0.16,95%CI:-0.42 to 0.10;P = 0.23;I2:42%),and major bleeding(overall OR = 1.25,95%CI:0.58-2.71;P = 0.56;I2:0%)between the two procedures.These differences remained statistically non-significant in all sensitivity analyses.CONCLUSION POEM was effective in treating achalasia.Shorter and longer myotomy procedures provided similar therapeutic effects in terms of long-term effectiveness.In addition,shorter myotomy reduced the operative time.
Key Words:Endoscopy;Meta-analysis;Myotomy;Peroral endoscopic myotomy;Gastroesophageal reflux disease
INTRODUCTION
Achalasia is a rare esophageal motor disease with a prevalence of approximately 1 case/100000 adults.The pathophysiology of achalasia disorder involves incomplete relaxation of the lower esophageal sphincter(LES)and impaired esophageal peristalsis[1].Its clinical manifestations comprise dysphagia,regurgitation,chest pain and weight loss.Currently,endoscopic botulinum toxin injection or pneumatic dilation and laparoscopic Heller myotomy(LHM)are used to treat achalasia[2].Inoue and colleagues[3]carried out the first peroral endoscopic myotomy(POEM)surgery to treat 17 achalasia patients in 2010 with 100% technical success.POEM is a novel,minimally invasive therapeutic modality for achalasia and related disorders,which was first reported by Inoueet al[3]in 2010.Since then,POEM has been widely used in the treatment of achalasia in many studies and achieves excellent efficacy[4-7].
However,the technique of POEM has changed very little since its introduction[3].During POEM,the variable extent of gastric myotomy and esophageal myotomy range from 2 cm to 3 cm and 6 cm to 10 cm,respectively.Meanwhile,previous studies have demonstrated the significance of the extent of the myotomy on the gastric side[8,9].However,the clinical relevance of myotomy length on the esophagus remains unknown.Some researchers have also adopted shorter myotomy in POEM and achieved similar efficacy in recent years[10].
The existing literature lacks high-quality evidence to compare the clinical outcomes of short-length and long-length POEM for achalasia treatment.Furthermore,for shorter or longer myotomy in POEM,which is more effective remains unknown.In this study,we compared the two myotomy modalities based on clinical outcomes and the incidence of postoperative adverse events.
MATERIALS AND METHODS
Data source and search strategy
The present systematic review and meta-analysis was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses(PRISMA)guidelines.PubMed,EmBase,Web of Science,Cochrane Library and clinicaltrials.gov databases were searched for relevant studies published from January 2010 to October 2020,because POEM was first reported in humans in 2010[3].The searching language of publications was restricted to English.The Medical Subject Headings(MESH)terms employed included Achalasia’s,Esophageal OR Esophageal Achalasia’s OR Cardiospasm OR Cardiospasms OR Achalasia OR Achalasia’s OR Achalasia,Esophageal OR Megaesophagus OR Esophageal Achalasia AND POEM OR Peroral endoscopic myotomy OR esophageal myotomy OR Peroral endoscopic myotomy AND shorter OR longer OR modified.The reference lists of eligible articles were further assessed for additional studies of interest.Two investigators independently performed the search and data extraction,assessed the quality of the articles and the discrepancies were resolved by consensual discussion.The third investigator reviewed the extracted data.Discussion with senior authors solved any arising issues.Randomized clinical trials(RCTs)and retrospective studies were qualified for the search.
Study selection
Article title and abstract eligibility screening was performed in an independent way by two investigators.Open-label double-blinded RCTs,as well as retrospective trials evaluating patients and comparing peroral endoscopic shorter and longer myotomy for the treatment of achalasia were included.Exclusion criteria were:(1)Experimental studies;(2)Publication language other than English;and(3)An editorial,a case report,a review or case series.
The data parameters obtained from each study were:(1)Trial features such as study design,sample size,follow-up duration and publication year;(2)Primary outcome,i.e.clinical success;and(3)Secondary outcomes,including(i)operative time,(ii)GERD(the main indicator was endoscopic reflux esophagitis),(iii)total number of adverse events(AEs)such as major bleeding,and(iv)procedurerelated parameters.
Quality assessment
The Cochrane “risk of bias” tool and the Newcastle-Ottawa Scale(NOS)were employed for assessing methodological quality of included studies[11].Discrepancies between the two investigators were resolved by consensual discussion.
Statistical analysis
Review Manager 5.3(RevMan)was utilized to analyze the extracted data and determine odds ratios(ORs)and 95% confidence intervals(CIs).Heterogeneity was determined by inspection of forest plots,the Cochrane Q test,and the I² statistic.A Q test with P<0.10 was considered significant.According to the Cochrane Handbook for Systematic Reviews of Interventions(https://training.cochrane.org/handbook),I² values were categorized as:< 30%,low heterogeneity;30%-50%,moderate heterogeneity;> 50%,substantial heterogeneity;> 75%,high heterogeneity.
RESULTS
Patient baseline features
Details of the selection process were outlined in Figure 1.Overall,711 articles were initially selected.After ruling out duplicates,reviews,case series,irrelevant and nonstandard records,6 studies were included which involved 3RCTs and 3 retrospective trials[12-17]and covered 545 patients.Their features are summarized in Table 1.The quality assessment of the studies was depicted in Figure 2.No significant differences were found in age,sex,American Society of Anesthesiologists(ASA)classification and previous interventions[18].The detailed study quality evaluation items were presented in Table 2.Compared with the long myotomy(LM)group,the length of esophageal myotomy in the short myotomy(SM)group was significantly reduced.The total incision range of the LM group was 8-25 cm,including 6-20 cm on the esophagus and 2-5 cm on the stomach.For the SM group,the cut range was 3-7cm,including 2-6 cm on the esophagus and 1-3 cm on the stomach.
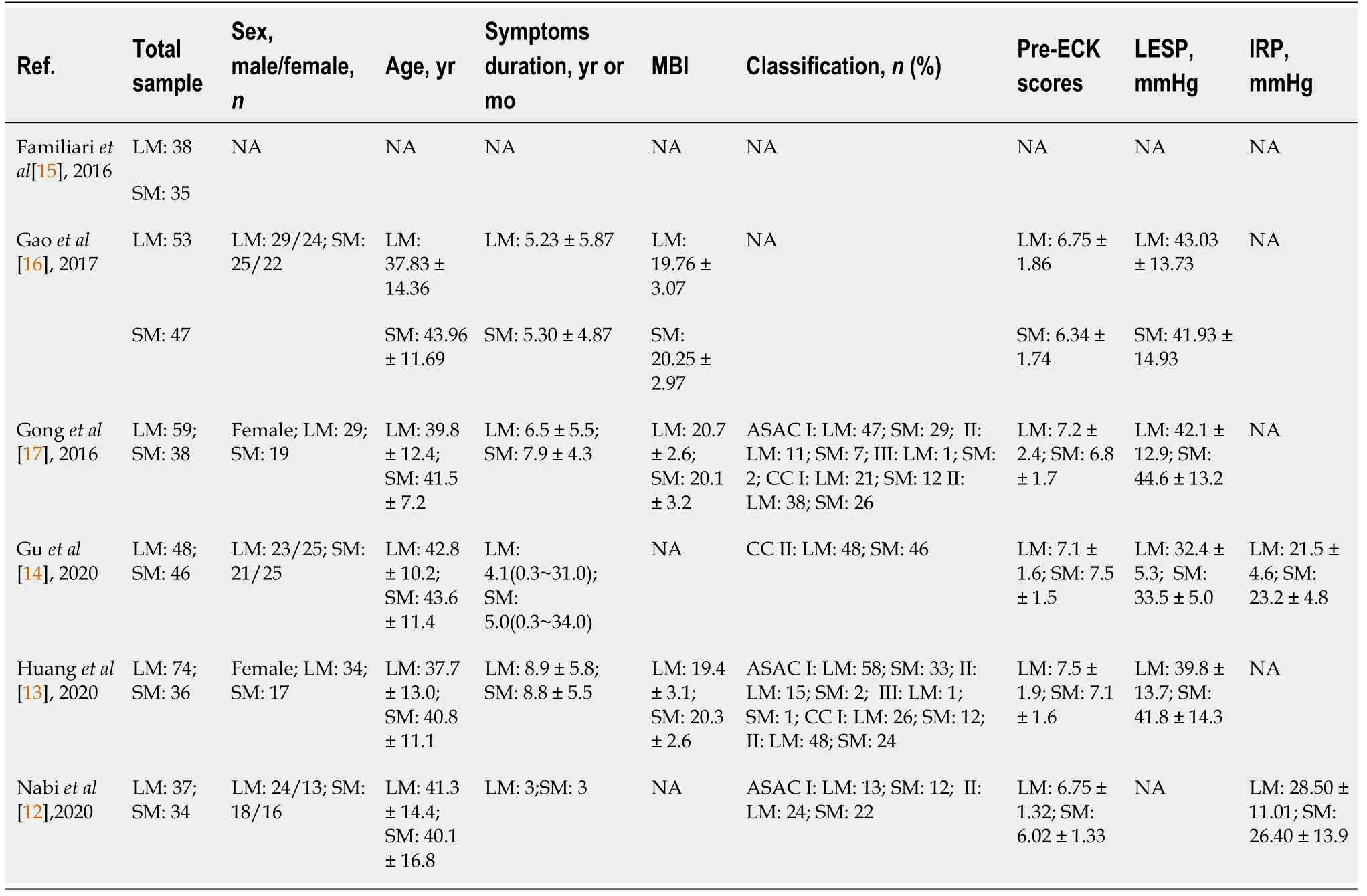
Table 1 Articles’ features
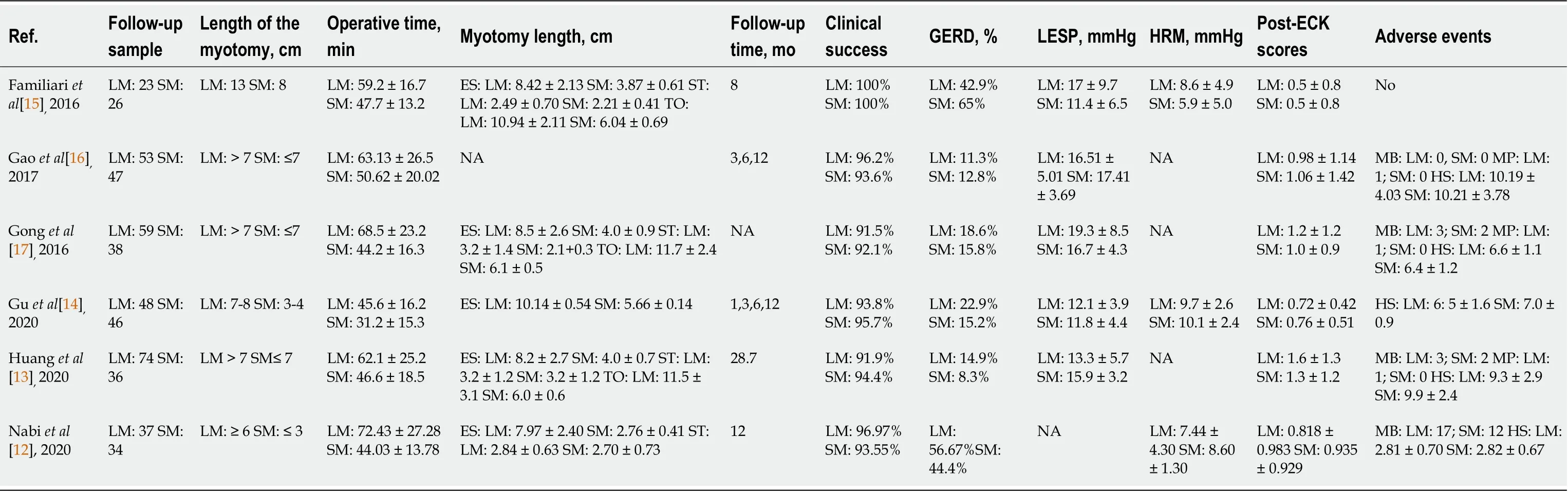
Table 2 The detailed study quality evaluation items
Clinical success
All patients were followed up for clinical success rate and Eckardt score.Data on clinical success after POEM were available in six studies(Figure 3)[overall clinical success(OR = 1,95%CI:0.46-2.17,P= 1,I2:0%;subgroup of abstract(OR = 1.19,95%CI:0.38 to 3.73;P= 0.76;I2:0%);subgroup of full text(OR = 0.86 95%CI:0.30 to 2.49;P= 0.78;I2:0%)].Therefore,clinical success of POEM showed no statistically significant difference between the two groups.Five studies presented pre-POEM Eckardt score as a quantitative variable.The score was 6.75 ± 1.86,7.2 ± 2.4,7.1 ± 1.6,7.5 ± 1.9,6.75 ± 1.32 in the LM group,respectively.In the SM group,the score was 6.34 ± 1.74,6.8 ± 1.7,7.5 ± 1.5,7.1 ± 1.6 and 6.02 ± 1.33,respectively.Six studies provided postoperative Eckardt scores,which were also comparable between the LM and SM group.The postoperative Eckardt score in the LM group was 0.5 ± 0.8;0.98 ± 1.14;1.2 ± 1.2;0.72 ± 0.42;1.6 ± 1.3;0.818 ± 0.983,respectively.Similarly,the score in the SM group was 0.5 ± 0.8;1.06 ± 1.42;1.0 ± 0.9;0.76 ± 0.51;1.3 ± 1.2 and 0.935 ± 0.929,respectively.
Procedure-related outcomes
Operative time:Total procedure duration was available in all six articles including a total of 521 patients.The operative time in the LM group was 59.2 ± 16.7,63.13 ± 26.50,68.5 ± 23.2,45.6 ± 16.2,62.1 ± 25.2 and 72.43 ± 27.28,respectively.For the SM group,the time was 47.7 ± 13.2,50.62 ± 20.02,44.2 ± 16.3,31.2 ± 15.3,46.6 ± 18.5 and 44.03 ± 13.78,respectively.Obviously,the operative times in the SM group were shorter than that in the LM group(Figure 4).
Figure 1 Flow diagram of the study selection process.
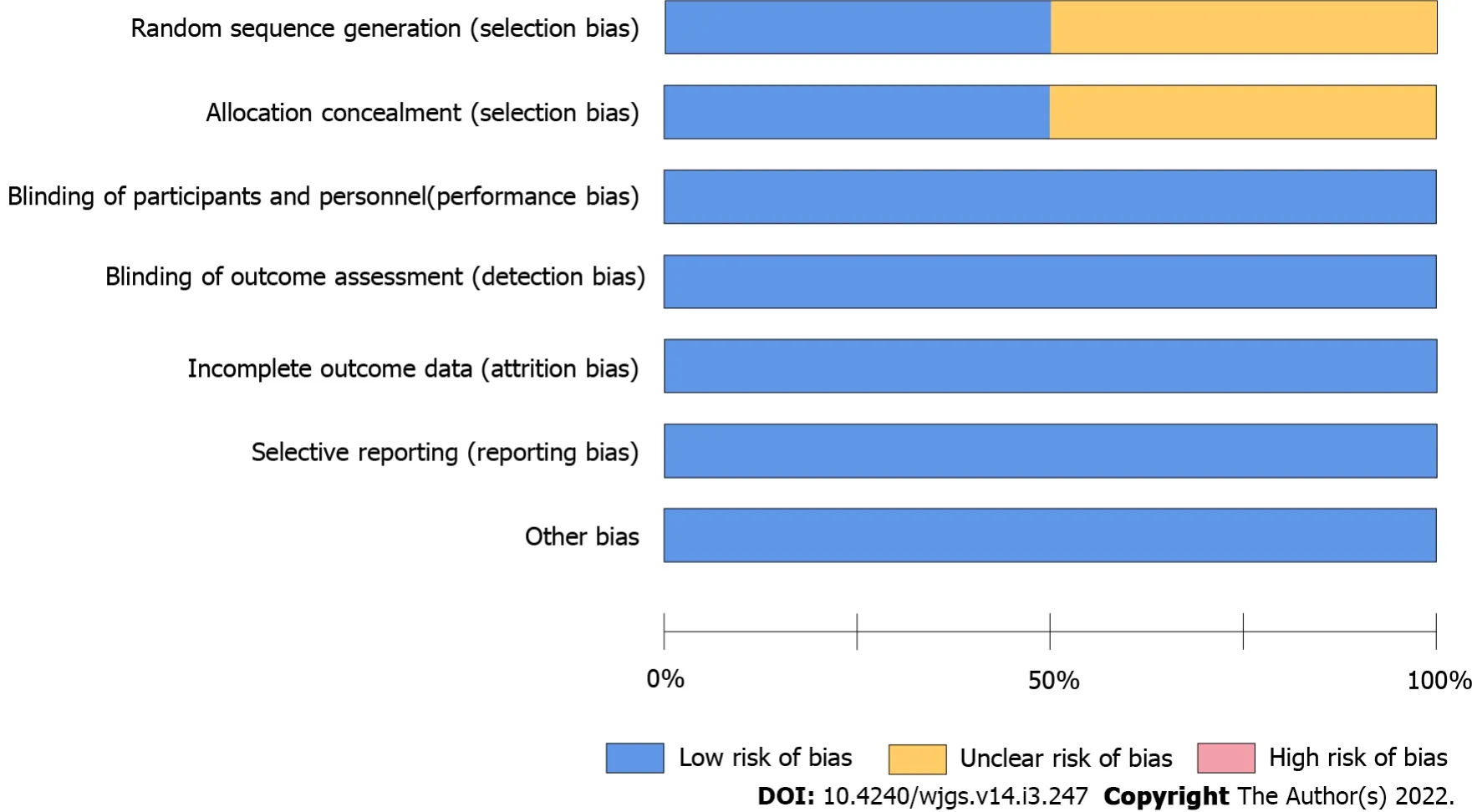
Figure 2 Risk of bias of the enrolled studies.The methodological quality of the included studies was similar.No study had a high risk for confounding variables.
Length of myotomy:A total of 3 RCTs and 2 retrospective studies involving 421 cases were metaanalyzed,with 180 cases in the SM group and 241 cases in the LM group.Myotomy length in POEM included the span of esophageal and gastric myotomy.The total length of myotomy in the LM group was 11.10 ± 2.0,11.5 ± 3.1 and 11.7 ± 2.4 cm,respectively.Among them,the esophageal myotomy length was 8.42 ± 2.13,8.2 ± 2.7,10.14 ± 0.54,7.97 ± 2.40 and 8.5 ± 2.6 cm,respectively,and the gastromyotomy length was 2.49 ± 0.70,3.2 ± 1.4,3.2 ± 1.2 and 2.84 ± 0.63 cm,respectively.The following myotomy values were obtained in the SM group of six studies:total length in three studies,6.04 ± 0.69,6.1 ± 0.5 and 6.0 ± 0.6 cm,respectively;esophageal length in five studies,3.87 ± 0.61,4.0 ± 0.9,5.66 ± 0.14,4.0 ± 0.7 and 2.76 ± 0.41 cm,respectively;and gastric length in four studies,2.21 ± 0.41,2.1 ± 0.3,3.2 ± 1.2 and 2.70 ± 0.73 cm,respectively.
Manometry outcomes:Preoperative LES pressure in POEM was available in four articles with a total of 401 patients,and five articles including 450 individuals assessed postoperative LES pressure.The level of preoperative LES pressure in the LM group was 43.03 ± 13.73,42.1 ± 12.9,32.4 ± 5.3 and 39.8 ± 13.7 mmHg respectively,and the value was 41.93 ± 14.93,44.6 ± 13.2,33.5 ± 5.0 and 41.8 ± 14.3 mmHg,respectively,in the SM group.Postoperative LES pressure level in the LM group was 17 ± 9.7,16.51 ± 5.01,19.3 ± 8.5,12.1 ± 3.9 and 13.3 ± 5.7 mmHg,respectively,and the pressure level was 11.4 ± 6.5,17.41 ± 3.69,16.7 ± 4.3,11.8 ± 4.4 and 15.9 ± 3.2 mmHg,respectively,in the SM group.
Integrated relaxation pressure:Preoperative integrated relaxation pressure(IRP)in POEM was available in two articles with a total of 165 patients,and three articles including 214 individuals assessed postoperative IRP pressure.The levels of preoperative IRP in the LM group were 21.5 ± 4.6 mmHg and 28.50 ± 11.01 mmHg,and in the SM group,the values were 23.2 ± 4.8 mmHg and 26.40 ± 13.9 mmHg.Postoperative IRP level in the LM group was 8.6 ± 4.9,9.7 ± 2.6,and 7.44 ± 4.30 mmHg,respectively,and this pressure level was 5.9 ± 5.0,10.1 ± 2.4 and 8.60 ± 1.30 mmHg,respectively,in the SM group.
Endoscopic reflux esophagitis:This meta-analysis found no difference in endoscopic reflux esophagitis between the two procedures(total OR = 1.21,95%CI:0.76-1.91;P= 0.42;I2:9%;subgroup of abstract OR = 0.77,95%CI:0.40-1.47;P= 0.43;I2:0%;subgroup of full text OR = 1.91,95%CI:0.98-3.75;P= 0.06;I2:0(F%ig),u wrei t5hA l)o.w heterogeneity found.Hence,random- and fixed-effects models yielded identical results
AEs:The incidence rates of AEs in different studies are detailed in Table 2.No procedure-related deaths were recorded.The rate of hospitalization showed no difference between the two procedures(total MD = -0.07,95%CI:-0.30 to 0.16;P= 0.55;I2:24%;subgroup of abstract MD = 0.20,95%CI:-0.25 to 0.65;P= 0.39;I2:0;subgroup of full text MD = -0.16,95%CI:-0.42 to 0.10;P= 0.23;I2:42%),with no heterogeneity detected(Figure 5B).The incidence rate of major bleeding was similar comparing the two groups(total OR = 1.25,95%CI:0.58-2.71;P= 0.56;I2:0%)(Figure 5C).These differences remained statistically significant in all sensitivity analyses.
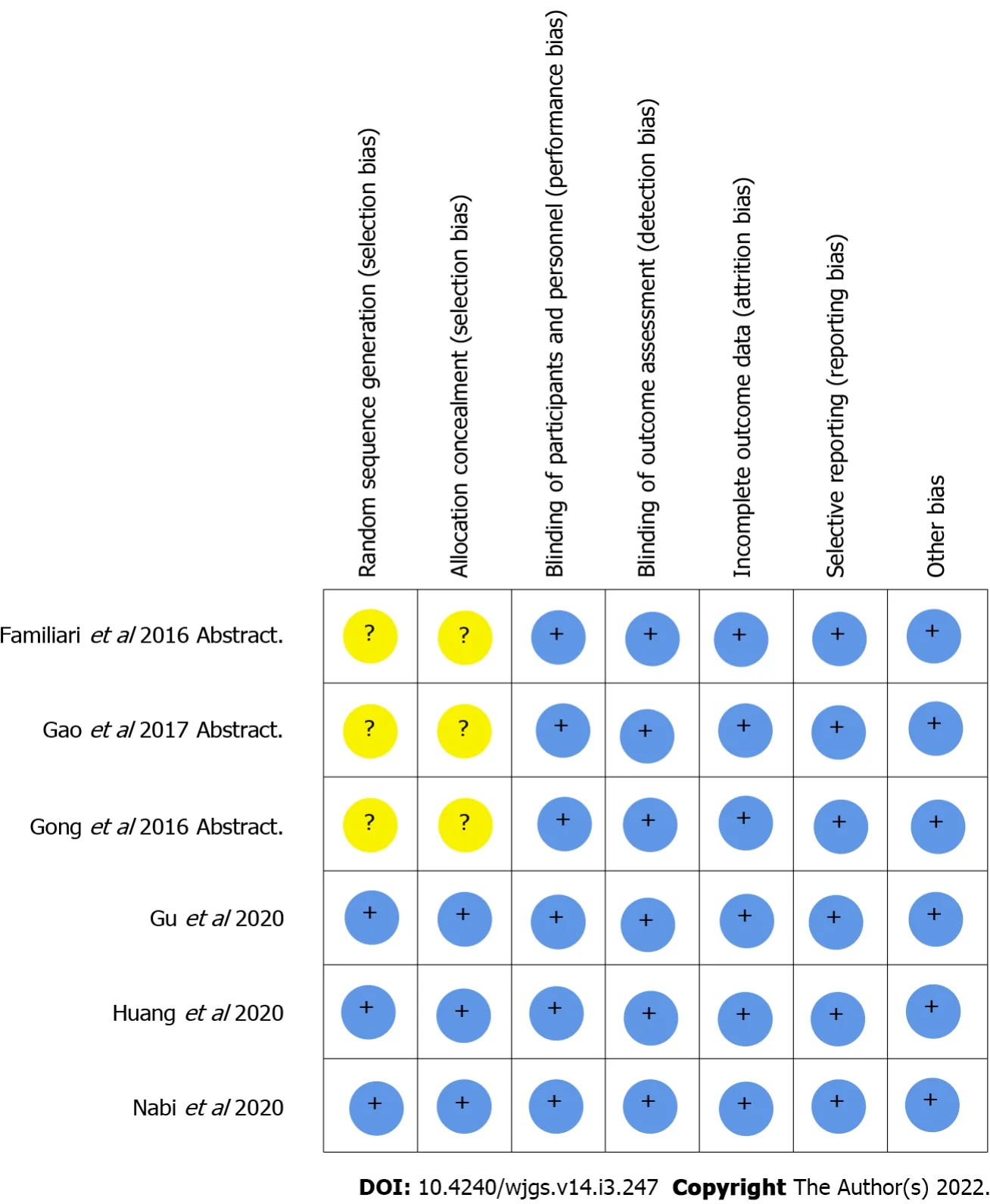
Figure 3 Long vs short myotomy.Meta-analysis of primary outcomes(clinical success rate).
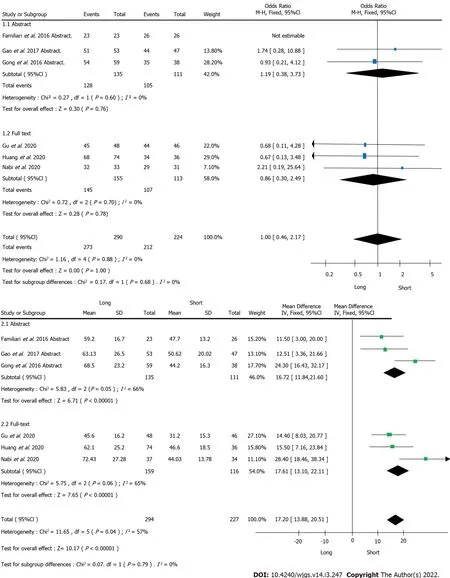
Figure 4 Operative time of long vs short myotomy.
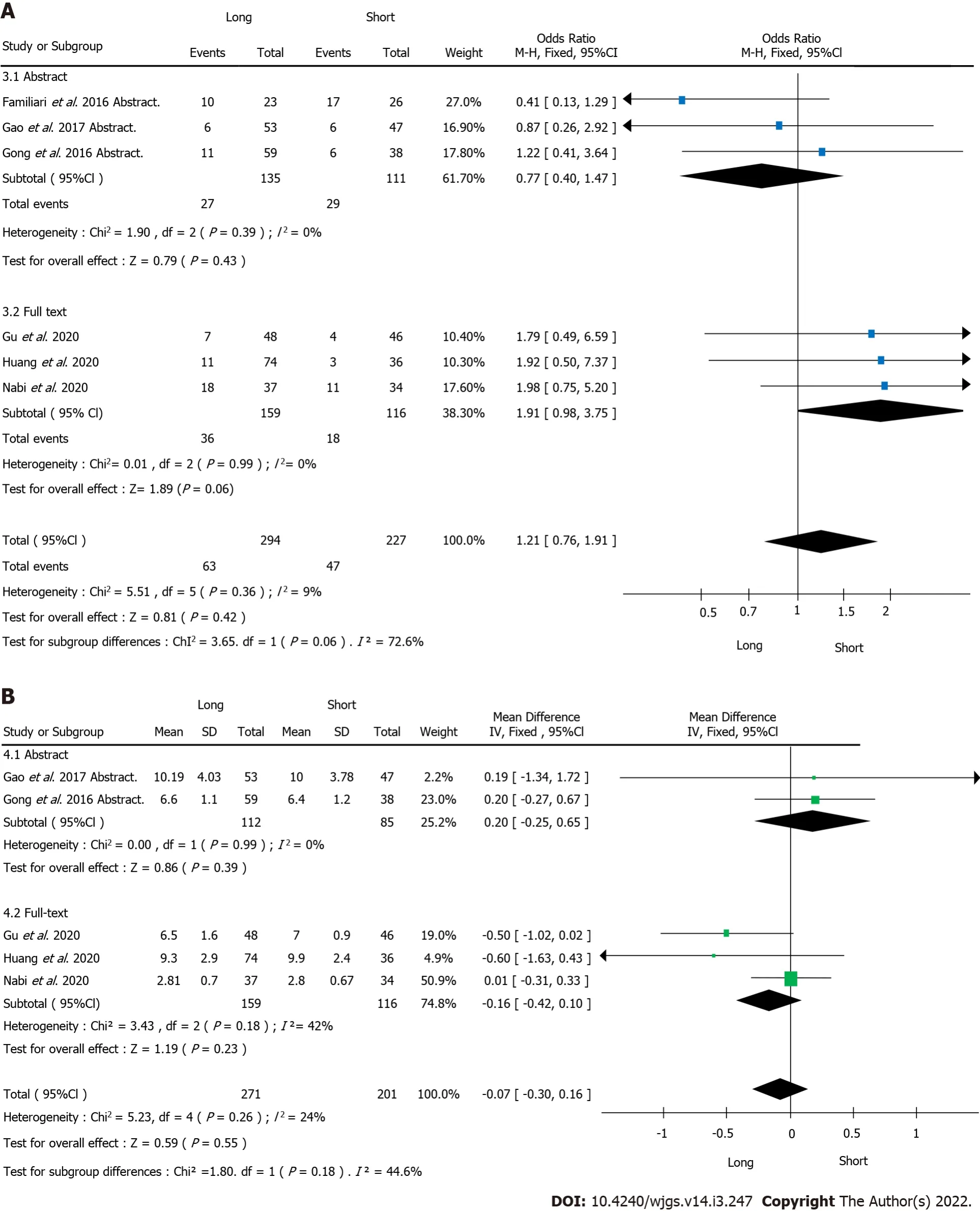
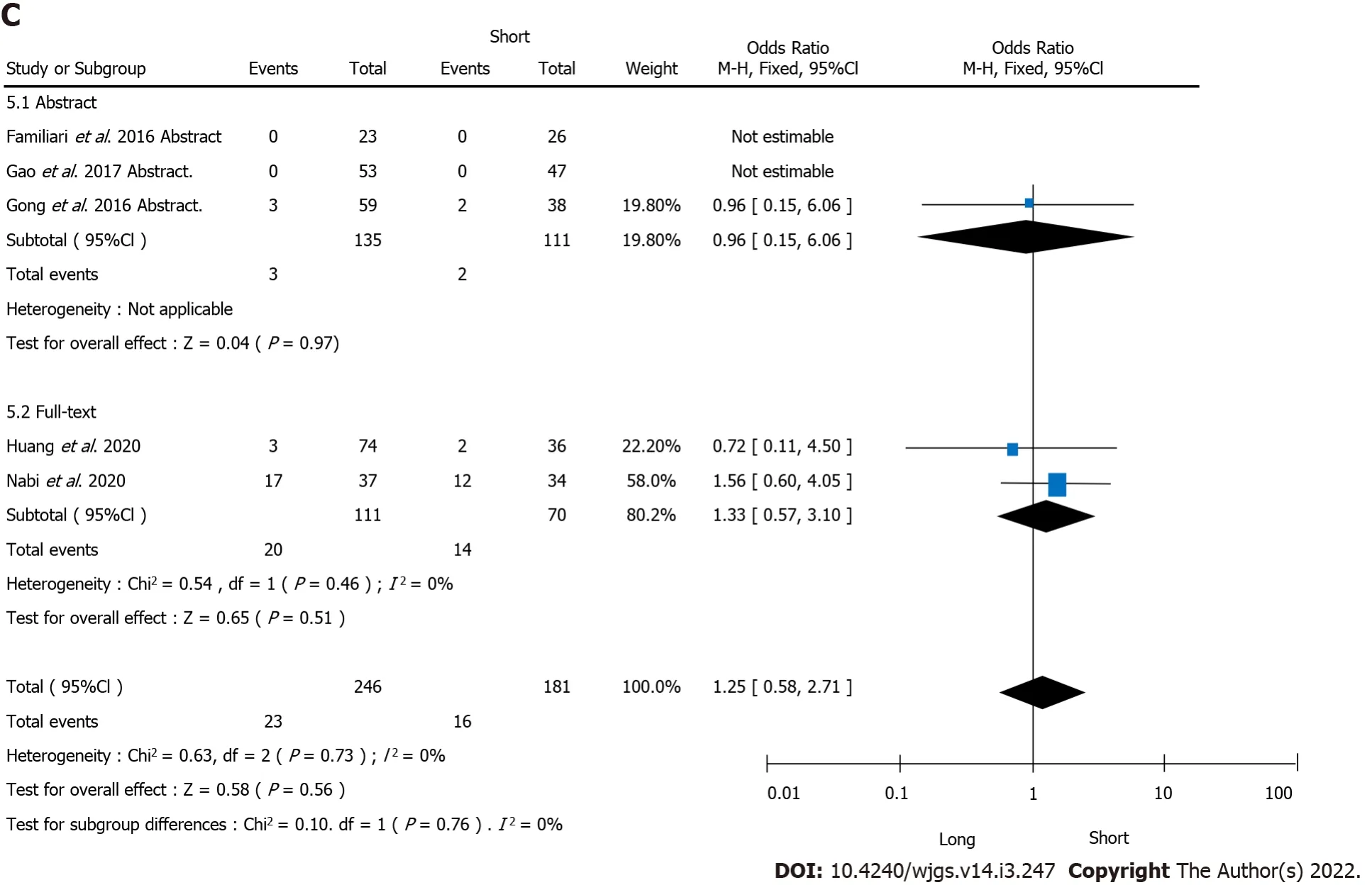
Figure 5 Long vs short myotomy.Meta-analysis of secondary outcomes.A:Endoscopic reflux esophagitis;B:Hospitalization;C:Major bleeding.
DISCUSSION
In this meta-analysis,we critically assessed the available RCTs and retrospective studies comparing SM and LM during POEM for the treatment of achalasia.Our main findings were that both approaches were equally effective yet the shorter procedure required reduced operation time.Heterogeneity across the studies was low and a comprehensive sensitivity analysis was consistent with our primary findings.No publication bias was detected.
The notion of endoscopic myotomy was first put forward by Ortega and collaborators[19],with an electrosurgical knife utilized for dissecting the lower esophageal rosette without manipulating the distal anti-reflux zone.Nevertheless,direct endoscopic myotomy has serious complications,and it has been abandoned.POEM was first reported by Pasricha and collaborators[20]in 2007 with pigs and utilized a submucosal tunnel for LES myotomy.In 2010,Inoue and collaborators[3]first applied POEM clinically using seven individuals who received a relatively shorter myotomy(mean length of 4.9 cm and 1.0 cm on the gastric side)but had worse clinical outcomes compared with the 10 cases undergoing a longer myotomy(mean length of 10.4 cm).With regard to myotomy length in POEM,Inoue and colleagues recommended to use a length of > 10 cm(average 13 cm)as the standard[21].Since then,POEM has been considered as an emerging treatment modality and is the preferred therapeutic option for achalasia and has shown success in all age groups and different types and stages of achalasia[22].In addition,POEM is promising in the treatment for spastic esophageal motility ailments.Avoiding abdominal incisions could reduce surgical invasiveness,improve cosmetic effects and shorten convalescence time[23].Moreover,POEM has been widely used clinically due to its advantages over LHM[24]including no abdominal cut,faster recovery and the possibility of avoiding general anesthesia.In addition,unlike LHM,POEM does not involve GEJ dissection[25].
The major differences in the implementation of POEM worldwide include myotomy orientation(anterior or posterior),thickness(full or partial)and length(shorter and longer).With regard to myotomy length in POEM surgery,Von Renteln and colleagues(Germany),Costamagna and collaborators(Italy),Chiu and co-workers(Hong Kong,China)and Minami and colleagues(Japan),all performed LM to treat achalasia with a mean incision length of 12,10,10.8 or 14.4 cm,and promising efficacy and safety have been achieved[26-29].However,these trials adopted the original LM POEM technique by Inoueet al[21],with a myotomy length of about 10 cm.Meanwhile,the average LES length was only 3.2 cm,ranging from 2.4 to 4.0 cm in healthy and achalasia individuals[30].According to the guidelines of the Society of American Gastrointestinal and Endoscopic Surgeons(SAGES),for cases of achalasia,esophageal myotomy length should be ≥ 4 cm and the gastromyotomy length should be 1-2 cm[31].Therefore,it was hypothesized that a modified POEM procedure with a LM might be as effective as the LM procedure in achalasia treatment as it ensured sufficient LES cutting while ameliorating complications and decreasing operation time.To test this hypothesis,Wanget al[10]enrolled 46 patients who underwent modified POEM with shorter submucosal tunnel(average length 6.8 cm)and endoscopic myotomy of muscle bundles(total average length 5.4 cm).They reported that modified POEM with LM showed great safety and commendable short-term efficacy in treating achalasia.However,for patients with type I and II achalasia,a short esophageal myotomy may be sufficient[10].
The present analysis,which was based on RCTs and a retrospective study,confirmed that POEM offered excellent efficacy with a high clinical success rate.The treatment efficacy was similar between the SM and LM procedures,regardless of the definition used,length of myotomy,publication type and the statistical method employed to pool the data.The meta-analysis of manometric outcomes,where no significant disparities were detected,further endorsed the lack of clinical differences between LM and SM.
Another matter of debate is GERD after POEM[32].Several technical refinements have been attempted to decrease the odds of post-POEM GERD,including a selective myotomy of the inner circular muscle[33],endoscopic fundoplication[34],or limiting the length of gastromyotomy[35].The proper location of the gastroesophageal junction(GEJ)is critical in ensuring the procedure’s effectiveness and may have an impact on GERD[36,37].Many reports showed a lower GERD incidence after POEM due to the preservation of the pharyngoesophageal ligament[38,39].In the present meta-analysis,the incidence rate of GERD was similar between the SM and LM procedures.
Regarding POEM-related AEs,multicenter studies showed that the technique was associated with a low incidence of severe AEs(< 1%)[40,41].Interestingly,we found that the total incidence rate of AEs,including hospitalization and major bleeding,were comparable between the two groups.Procedurerelated outcomes were also evaluated.As expected from our clinical experience,the SM took much less time compared with the LM but the treatment effects were similar.
This meta-analysis had some limitations.First,the number of studies was very small and three RCTs were only retrieved as abstracts.Although we conducted subgroup analysis based on abstract and fulltext,more studies were still needed to analyze the results.Second,only three articles evaluated IRP after POEM treatment.Third,a longer myotomy is thought to be more effective on controlling symptoms caused by the esophageal spasm of type III achalasia.However,in this meta-analysis,due to the small number of patients with type III achalasia and recent literature[18],our conclusions might not apply to type III achalasia treatment and a short myotomy could not be recommended.We expected more RCTs to examine the effect of shorter or longer in the treatment of type III achalasia.Due to the lack of relevant research articles,we did not evaluate the postoperative efficacy of POEM for achalasia subtypes.Fourth,the follow-up duration was relatively short so this study was unable to compare the long-term efficacy and AES between LM and SM procedures.
CONCLUSION
In conclusion,short myotomy has the advantage of reduced procedure time in the treatment of achalasia compared to long myotomy,but the clinical success rate,AEs,and reflux rate were comparable.Thus,peroral endoscopic shorter myotomy could have a great clinical application prospect.Our results are restricted by the small number of patients,short follow-up duration,and a lack of specific definition of short myotomy.Future studies with a larger sample size and longer follow-up duration are warranted to evaluate the long-term efficacy and safety of these two procedures in POEM.
ARTICLE HIGHLIGHTS
Research background
For a long time,peroral endoscopic myotomy(POEM)has been demonstrated to be safe and effective in the treatment of achalasia.
Research motivation
Longer myotomy is the standard POEM procedure for achalasia,but its effectiveness compared with shorter myotomy is not well known.Thus,we want to provide an analysis to assess the clinical outcomes of shorter and longer myotomy.
Research objectives
To conduct a meta-analysis to compare the clinical effectiveness of the two procedures.
Research methods3
The PubMed,Web of Science,Cochrane Library,clinicaltrials.gov,and EMBASE databases were used to search for relevant studies to compare shorter and longer myotomy in POEM for achalasia treatment.
Research results
Longer and shorter myotomy groups in treating achalasia had similar excellent effectiveness.Shorter myotomy had significantly reduced mean operative time compared with the longer procedure.There were no statistically significant differences in AE’s rates,including gastroesophageal reflux diseases,hospital stay and major bleeding between the two procedures.
Research conclusions
Short myotomy has the advantage of shorter procedure time in the treatment of achalasia compared to long myotomy,but the clinical success rate,adverse events ,and reflux rate were comparable.
Research perspectives
Future randomized clinical trials should determine whether the benefits remain comparable after years of follow-up.
FOOTNOTES
Author contributions:Weng CY and He CH collected data;Zhuang MY analyzed the data and wrote the first draft of the manuscript;Xu JL and Lyu B were major contributors in editing the manuscript;All authors read and approved the final manuscript.
Supported bythe National Natural Science Foundation of China,No.8177030774.
Conflict-of-interest statement:The authors declare they have no competing financial and non-financial interests.
PRISMA 2009 Checklist statement:The authors have read the CARE Checklist(2016),and the manuscript was prepared and revised according to the CARE Checklist(2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See:https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Chun-Yan Weng 0000-0003-3618-9629;Cheng-Hai He 0000-0001-8322-2669;Ming-Yang Zhuang 0000-0001-6392-716X;Jing-Li Xu 0000-0002-2264-8591;Bin Lyu 0000-0002-6247-571X.
S-Editor:Wang LL
L-Editor:Filipodia
P-Editor:Wu RR
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Is it sufficient to evaluate only preoperative systemic inflammatory biomarkers to predict postoperative complications after pancreaticoduodenectomy?
- Successful treatment with laparoscopic surgery and sequential multikinase inhibitor therapy for hepatocellular carcinoma:A case report
- New common bile duct morphological subtypes:Risk predictors of common bile duct stone recurrence
- Does cranial-medial mixed dominant approach have a unique advantage for laparoscopic right hemicolectomy with complete mesocolic excision?
- Fast-track protocols in laparoscopic liver surgery:Applicability and correlation with difficulty scoring systems