Choledocholithiasis characteristics with periampullary diverticulum and endoscopic retrograde cholangiopancreatography procedures:Comparison between two centers from Lanzhou and Kyoto
2022-04-01KeXiangZhuPingYueHaiPingWangWenBoMengJianKangLiuLeiZhangXiaoLiangZhuHuiZhangLongMiaoZhengFengWangWenCeZhouAzumiSuzukiKiyohitoTanakaXunLi
Ke-Xiang Zhu,Ping Yue,Hai-Ping Wang,Wen-Bo Meng,Jian-Kang Liu,Lei Zhang,Xiao-Liang Zhu,Hui Zhang,Long Miao,Zheng-Feng Wang,Wen-Ce Zhou,Azumi Suzuki,Kiyohito Tanaka,Xun Li
Ke-Xiang Zhu,Ping Yue,Wen-Bo Meng,Lei Zhang,Xiao-Liang Zhu,Hui Zhang,Long Miao,Zheng-Feng Wang,Wen-Ce Zhou,Xun Li,Department of General Surgery,The First Hospital of Lanzhou University,Lanzhou 730000,Gansu Province,China
Ke-Xiang Zhu,Ping Yue,Hai-Ping Wang,Wen-Bo Meng,Lei Zhang,Xiao-Liang Zhu,Hui Zhang,Long Miao,Zheng-Feng Wang,Wen-Ce Zhou,Xun Li,Key Laboratory of Biological Therapy and Regenerative Medicine Transformation Gansu Province,The First Hospital of Lanzhou University,Lanzhou 730000,Gansu Province,China
Jian-Kang Liu,Cardiovascular Division,Brigham and Women’s Hospital,Harvard Medical School,Boston,MA 02451,United States
Azumi Suzuki,Kiyohito Tanaka,Department of Gastroenterology,Kyoto Second Red Cross Hospital,Kyoto 602-8026,Japan
Abstract BACKGROUND Most of study regarding periampullary diverticulum(PAD)impact on endoscopic retrograde cholangiopancreatography(ERCP)therapy for choledocholithiasis based on data from one endoscopy center and lacked to compare the clinical characteristic of choledocholithiasis with PAD from different geographical patients.AIM To compare the choledocholithiasis clinical characteristics between two regional endoscopy centers and analyze impacts of clinical characteristics on ERCP methods for choledocholithiasis patients with PAD.METHODS Patients seen in two endoscopy centers(The First Hospital of Lanzhou University,Lanzhou,Gansu Province,China,and Kyoto Second Red Cross Hospital,Kyoto,Japan)underwent ERCP treatment for the first time between January 2012 and December 2017.The characteristics of choledocholithiasis with PAD were compared between the two centers,and their ERCP procedures and therapeutic outcomes were analyzed.RESULTS A total of 829 out of 3608 patients in the Lanzhou center and 241 out of 1198 in the Kyoto center had choledocholithiasis with PAD.Lots of clinical characteristics were significantly different between the two centers.The common bile duct(CBD)diameter was wider,choledocholithiasis size was lager and multiple CBD stones were more in the Lanzhou center patients than those in the Kyoto center patients(14.8 ± 5.2 mm vs 11.6 ± 4.2 mm,12.2 ± 6.5 mm vs 8.2 ± 5.3 mm,45.3% vs 20.3%,P < 0.001 for all).In addition,concomitant diseases,such as acute cholangitis,gallbladder stones,obstructive jaundice,cholecystectomy,and acute pancreatitis,were significantly different between the two centers(P = 0.03 to < 0.001).In the Lanzhou center,CBD diameter and choledocholithiasis size were lower,and multiple CBD stones and acute cholangitis were less in non-PAD patients than those in PAD patients(13.4 ± 5.1 mm vs 14.8 ± 5.2 mm,10.3 ± 5.4 mm vs 12.2 ± 6.5,39% vs 45.3%,13.9% vs 18.5%,P = 0.002 to < 0.001).But all these characteristics were not significantly different in the Kyoto center.The proportions of endoscopic sphincterotomy(EST),endoscopic balloon dilatation(EPBD),and EST+EPBD were 50.5%,1.7%,and 42.5% in the Lanzhou center and 90.0%,0.0%,and 0.4% in the Kyoto center,respectively.However,the overall post-ERCP complication rate was not significantly different between the two centers(8.9% in the Lanzhou and 5.8% in the Kyoto.P = 0.12).In the Lanzhou center,the difficulty rate in removing CBD stones in PAD was higher than in non-PAD group(35.3% vs 26.0%,P < 0.001).But the rate was no significant difference between the two groups in Kyoto center.The residual rates of choledocholithiasis were not significantly different between the two groups in both centers.Post-ERCP complications occurred in 8.9% of the PAD patients and 8.1% of the non-PAD patients in the Lanzhou Center,and it occurred in 5.8% in PAD patients and 10.0% in non-PAD patients in the Kyoto center,all P > 0.05.CONCLUSION Many clinical characteristics of choledocholithiasis patients with PAD were significantly different between the Lanzhou and Kyoto centers.The patients had larger and multiple stones,wider CBD diameter,and more possibility of acute cholangitis and obstructive jaundice in the Lanzhou center than those in the Kyoto center.The ERCP procedures to manage native duodenal papilla were different depending on the different clinical characteristics while the overall post-ERCP complications were not significantly different between the two centers.The stone residual rate and post-ERCP complications were not significantly different between choledocholithiasis patients with PAD and without PAD in each center.
Key Words:Clinical characteristics;Periampullary diverticulum;Endoscopic retrograde cholangiopancreatography;Choledocholithisasis
lNTRODUCTlON
Choledocholithiasis is a common disease of the biliary tract system,and its causes are not completely clear,but its occurrence is closely related to periampullary diverticulum(PAD).It was reported that the incidence of bile duct stones reached 51.3%-88.0% among PAD patients[1-4].Our previous study also revealed that PAD is an important factor for the occurrence and reoccurrence of bile duct stones[5].Endoscopic retrograde cholangiopancreatography(ERCP)is regarded as an effective method for the treatment of choledocholithiasis.However,the anatomy of the duodenal junction may change due to the presence of PAD and possibly make ERCP cumbersome in the treatment of choledocholithiasis[6-9].Therefore,many studies have focused on the safety and success of ERCP for PAD patients with choledocholithiasis[6,9-13].However,there were inconsistent results regarding the impact of PAD on the safety and success of ERCP for choledocholithiasis.Some studies have shown that PAD is a challenge in ERCP[6,14].Other studies concluded that PAD was not considered an obstacle to ERCP cannulation[4,7,9].Regarding efficacy,some studies have reported that therapeutic outcomes are not affected by the presence of PAD,and complication rates of ERCP were similar in patients with and without PAD[9].However,other studies suggested that a high rate of ERCP-related complications was associated with PAD[14-15],and it is unknown what caused those differences.Hypothetically,one of the reasons for these inconsistent conclusions may be associated with the discrepancies in the clinical characteristics in different studies regarding PAD patients with choledocholithiasis.
Many previous studies were based on data from only one endoscopy center and lacked a comparison of the clinical characteristics of choledocholithiasis with PAD from different regions.Thus,little is known about the difference in the clinical characteristics of choledocholithiasis with PAD patients from different regions and the impact of the clinical characteristics on ERCP methods.Therefore,in this study,we compared the clinical characteristics of PAD patients with choledocholithiasis and identified the impact of PAD on the methods and efficacy of ERCP,involving two different regional endoscopy centers(The First Hospital of Lanzhou University,a University School of Medicine of Gansu,Lanzhou,Gansu Province,China,and the Kyoto Second Red Cross Hospital,Kyoto,Japan)over the same period.
MATERlALS AND METHODS
This study was performed in two endoscopy centers,the First Hospital of Lanzhou University,a University School of Medicine of Gansu,China,and the Kyoto Second Red Cross Hospital,Japan.PAD patients with choledocholithiasis were enrolled retrospectively from all patients with a naïve papilla who needed therapeutic ERCP between January 2012 and December 2017.Patient information included patient demographics,diagnosis with PAD or without PAD,diameter of the common bile duct(CBD),presence of choledocholithiasis,maximum diameter and number of choledocholithiasis,and concomitant diseases such as acute cholangitis,gallbladder stones,obstructive jaundice,cholecystectomy,and acute pancreatitis.The ERCP procedure,whether there was difficulty cannulating or not,the outcome of therapeutic ERCP for choledocholithiasis with PAD and the difficulty in removing the stones,residual stones in the CBD,and post-ERCP complications were all evaluated.
According to the above mentioned data,the comparative analysis was as follows:(1)comparison of the clinical characteristics of PAD patients with choledocholithiasis between the Lanzhou and Kyoto endoscopy centers and comparison of the clinical characteristics of patients with choledocholithiasis with and without PAD within each endoscopy center;(2)the ERCP procedures for PAD patients with choledocholithiasis between the two endoscopy centers and the ERCP curative efficacy with and without PAD within each center.The difficulty of removing biliary stones was defined by the presence of one or more of the following situations:the need for mechanical lithotripsy or another fragmented method;failure to remove the bile duct stones within 30 min;failure of stone extraction with a standard basket;and more than two endoscopic balloon dilatations(EPBDs).Residual stones in the common bile duct were defined as follows:Some choledocholithiasis was still in the bile duct or stones were suspected to still be in the bile duct through X-ray fluoroscopy at the end of ERCP and choledocholithiasis was again diagnosed within 3 mo after the first ERCP.Patients were placed under conscious sedation with meperidine and midazolam.ERCP was performed by experienced endoscopists who performed over 100 biliary interventions per year.Patients who initially planned to undergo diagnostic ERCP were not enrolled in this study.The follow-up was started as long as the ERCP was performed.
Statistical analysis
Categorical variables were analyzed with the chi-squared or Fisher’s exact test,while continuous variables were expressed as the median and interquartile range and compared with the Wilcoxon rank sum test,or expressed as the mean and standard deviation and compared witht-test.All statistical assessments were 2-sided,and aPvalue less than 0.05 was considered significant.Statistical analysis was performed using the SAS 9.4(SAS Institute Inc.,Cary,NC,USA).
RESULTS
In the cases of choledocholithiasis with PAD,829 of 3608 patients in the Lanzhou center,and 241 of 1198 patients in the Kyoto center were enrolled in consecutive first session ERCP.Comparing the clinical characteristics between the Lanzhou center and the Kyoto center,patient age,diameter of the CBD,stone number and size in the CBD,comorbidities such as acute cholangitis,gallstones,obstructive jaundice,acute pancreatitis,and operation history of the bile duct were all significantly different,except for sex.In detail,compared with an average diameter(11.6 ± 4.2 mm)of the CBD in patients in the Kyoto center,the average diameter of the CBD was 14.8 ± 5.2 mm in patients in the Lanzhou center.Compared with the mean diameter of choledocholithiasis that was 8.2 ± 5.3 mm in patients in the Kyoto center,the mean diameter of choledocholithiasis was 12.2 ± 6.5 mm in Lanzhou.Regarding single or multiple choledocholithiasis,45.3% of the patients had multiple stones and 54.7% of the patients had single stones in the Lanzhou center but 20.3% and 79.7% of patients had single and multiple stones in the Kyoto center,respectively.Each of those comparisons was significantly different(P< 0.001).Some comorbidities were also significantly different between the Lanzhou and Kyoto centers:acute cholangitis(18.5%vs9.5%,P= 0.001);obstructive jaundice(13.8%vs0.4%,P< 0.001);acute pancreatitis(4.7%vs1.7%,P= 0.03);cholecystectomy(38.4%vs3.7%,P< 0.001);and gallbladder stones(4.7%vs12.5%,P< 0.001)(Table 1).
The failure rate of ERCP was not different between the two endoscopy centers,but the difficulty rate of deep cannulation of the bile duct was significantly different:9.7% in Lanzhouvs24.1% in Kyoto(P<0.001).The proportions of endoscopic sphincterotomy(EST),EPBD,and EST+EPBD were 50.5%,1.7%,and 42.5% in the Lanzhou center and 90.0%,0.0%,and 0.4% in the Kyoto center,respectively.ERCP procedures to handle the duodenal papilla were significantly different between the two centers(P<0.001).Regarding ERCP-related complications,the overall complication rate was 8.9% in Lanzhou and 5.8% in Kyoto.The results showed that the overall complications were not significantly different between the Lanzhou and Kyoto centers(P= 0.12)(Table 2).
Comparing PAD with non-PAD in each center,the results were as follows:The mean age of the PAD group was 56 years and was 65 years for non-PAD in Lanzhou,and it was 71 years and 76 with and without PAD in Kyoto,respectively.The mean age of PAD patients was significantly older than those without PAD in each center.In the Lanzhou center,the mean diameter of the CBD was 14.8 ± 5.2 mm in the PAD group and 13.4 ± 5.1 mm in the non-PAD group.The mean diameter of the CBD in the PAD group was significantly wider than that in the non-PAD group(P< 0.001).In the Kyoto Center,the mean diameter of the CBD was 11.6 ± 4.2 mm in the PAD group and 10.9 ± 3.6 mm in the non-PAD group.The mean diameter of the CBD was not significantly different between the two groups in Kyoto.Likewise,the mean diameter of the CBD stones was 12.2 ± 6.5 mm and 10.3 ± 5.4 mm in PAD group and non-PAD group in Lanzhou,respectively,and was 8.2 ± 5.3 mm and 7.5 ± 5.2 mm in PAD group and non-PAD group in Kyoto,respectively.The mean diameter of the CBD stones in the PAD group was higher than that in the non-PAD group in the Lanzhou center,whereas there was no significant difference in the diameter of the CBD stones in the Kyoto Center.The cases of multiple CBD stones were 45.3% and 39% in the PAD group and non-PAD group in the Lanzhou center and 20.3% and 19% in the PAD group and non-PAD group in the Kyoto center,respectively.The percent of patients with PAD with multiple CBD stones was significantly higher in Lanzhou but not in Kyoto.Concomitant diseases such as acute cholangitis,gallstones,and obstructive jaundice were significantly different between PAD and non-PAD patients in the Lanzhou center,but those comorbidities were not different between the PAD and non-PAD groups in the Kyoto center(Table 3).
The rate in the difficulty to cannulate aim tubes was 9.7% and 8.1% in the PAD group and non-PAD group in Lanzhou center,respectively,with no significant difference between the two groups(P= 0.19).Furthermore,in the Kyoto center,the rates were 24.1% and 32.5% in the PAD group and non-PAD group,respectively,with a significant difference between the two groups(P= 0.02)(Table 4).In the Lanzhou center,EST was performed in 57.9% and EST plus EPBD was performed in 33.5% of non-PAD patients,while EST was performed in 50.5% and EST plus EPBD was performed in 42.5% of PAD patients.The ERCP procedures to handle native duodenal papilla were different between the PAD and non-PAD groups in the Lanzhou center.In the Kyoto center,EST was performed in 87.6%,EST plus EPBD was performed in 1.1% of non-PAD patients,EST was performed in 90.0%,and EST plus EPBD was performed in only 0.4% of PAD patients.There were no differences in the ERCP procedures to handle native duodenal papilla between the PAD and non-PAD groups in Kyoto(Table 4).
Regarding the rate of difficulty in removing the stones,in the Lanzhou center,the ratio reached 35.3%and 26.0% in the PAD group and non-PAD group,respectively,with a significant difference between the two groups(P< 0.001),while it accounted for 53.8% and 53.3% in the PAD group and non-PAD group in the Kyoto center,respectively,with no significant difference between the two groups(P= 0.89)(Table 4).
The residual rate of choledocholithiasis in the Lanzhou center was 7.6% and 6.6% in the PAD group and non-PAD group,respectively,and it was 24.6% and 23.4% in the PAD group and non-PAD group in the Kyoto center,respectively.The residual rate of choledocholithiasis was not significantly different between the PAD group and the non-PAD group,both in the Lanzhou center(P= 0.39)and in the Kyoto center(P= 0.73)(Table 4).

Table 1 Comparison clinical characteristics of choledocholithiasis patient with periampullary diverticulum between Lanzhou and Kyoto
Post-ERCP complications occurred in 8.9% of PAD patients and 8.1% of non-PAD patients in the Lanzhou center;furthermore,it was 5.8% in PAD patients and 10.0% in non-PAD patients in the Kyoto center.The post-ERCP complications between PAD and non-PAD patients in each center was not significantly different(Lanzhou,P= 0.48;Kyoto,P= 0.07)(Table 4).
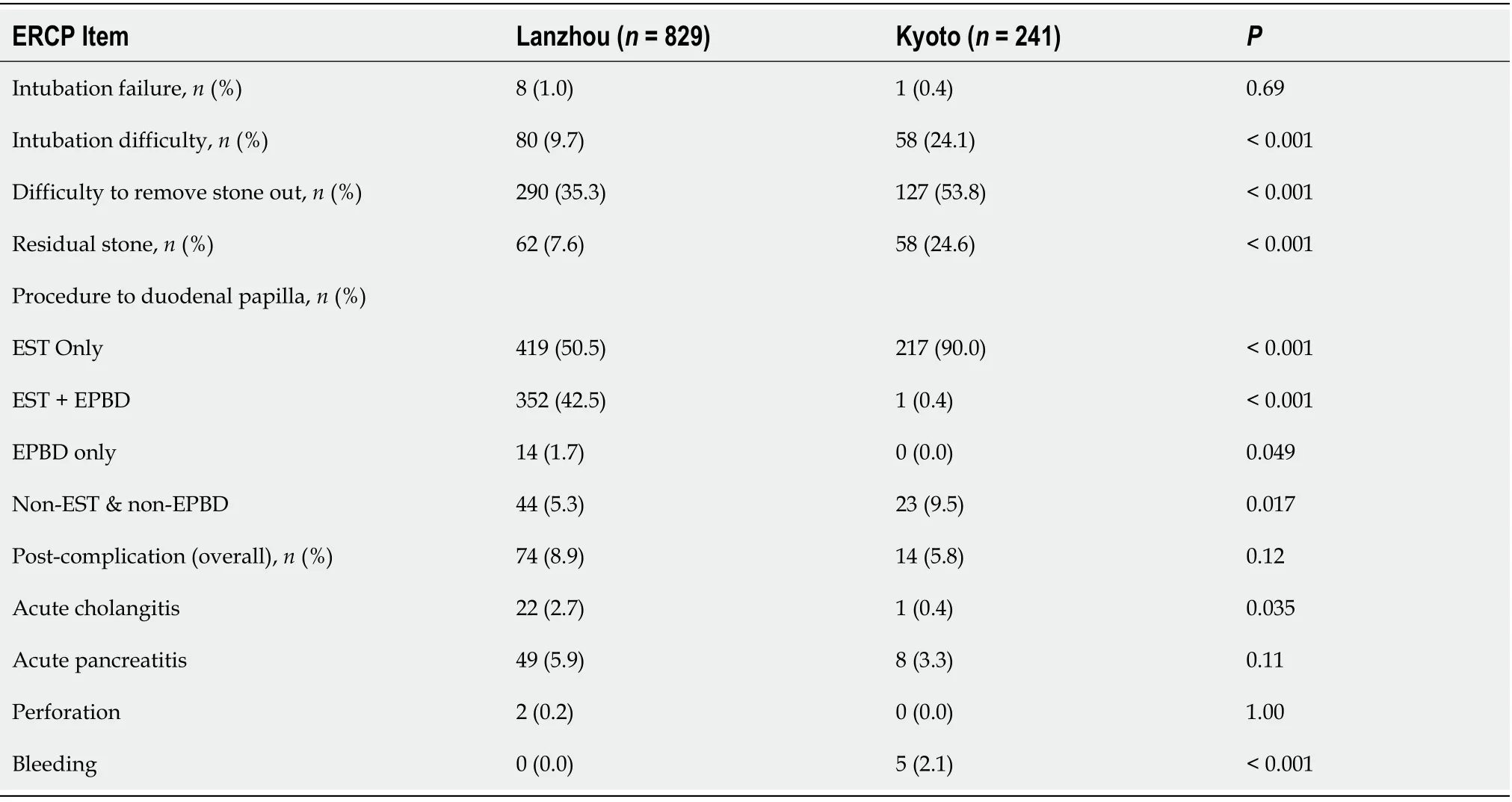
Table 2 Comparison of endoscopic retrograde cholangiopancreatography related contents of choledocholithiasis with periampullary diverticulum between Lanzhou and Kyoto
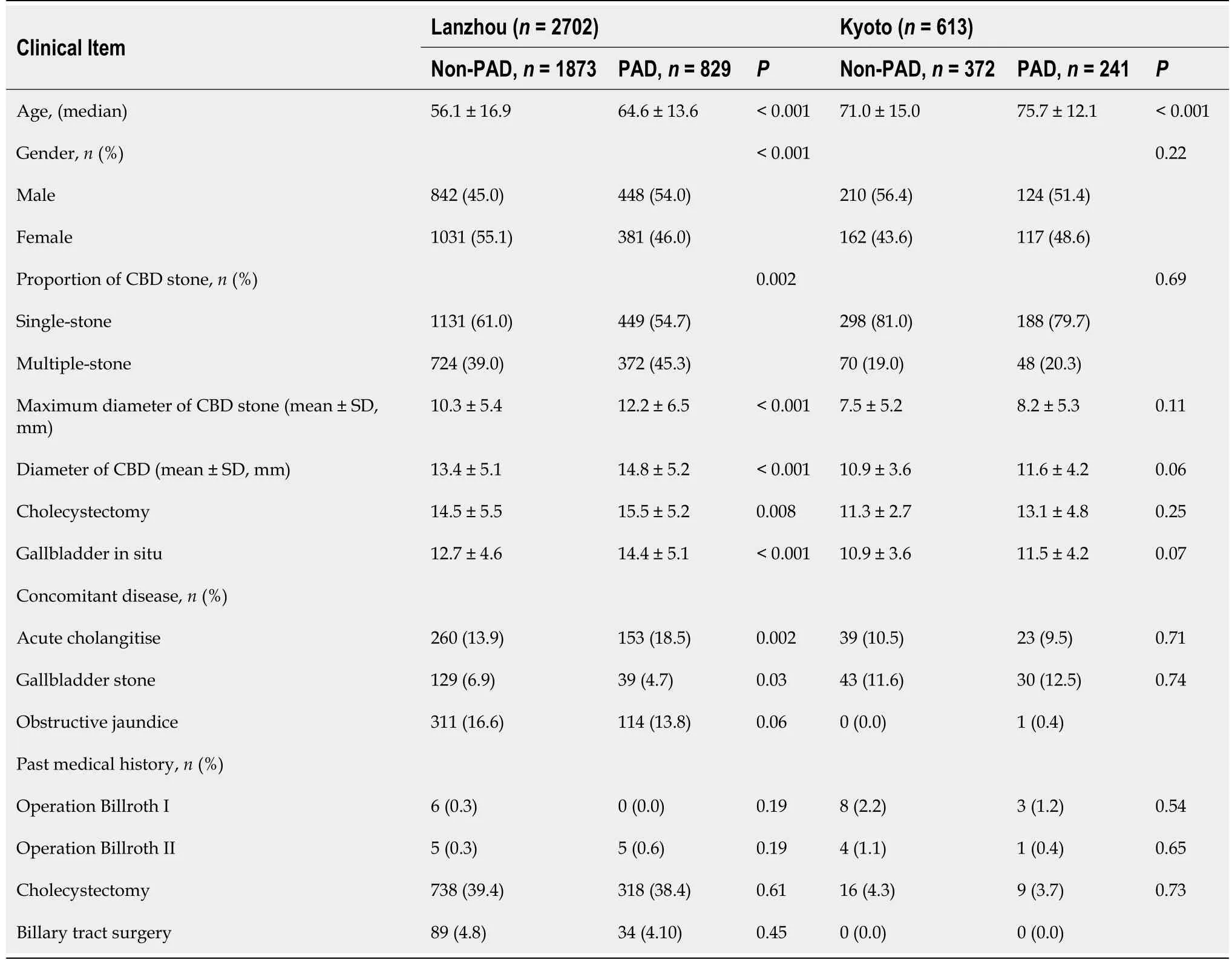
Table 3 Comparison of clinical characteristics of choledocholithiasis patient with and without periampullary diverticulum in Lanzhou or Kyoto
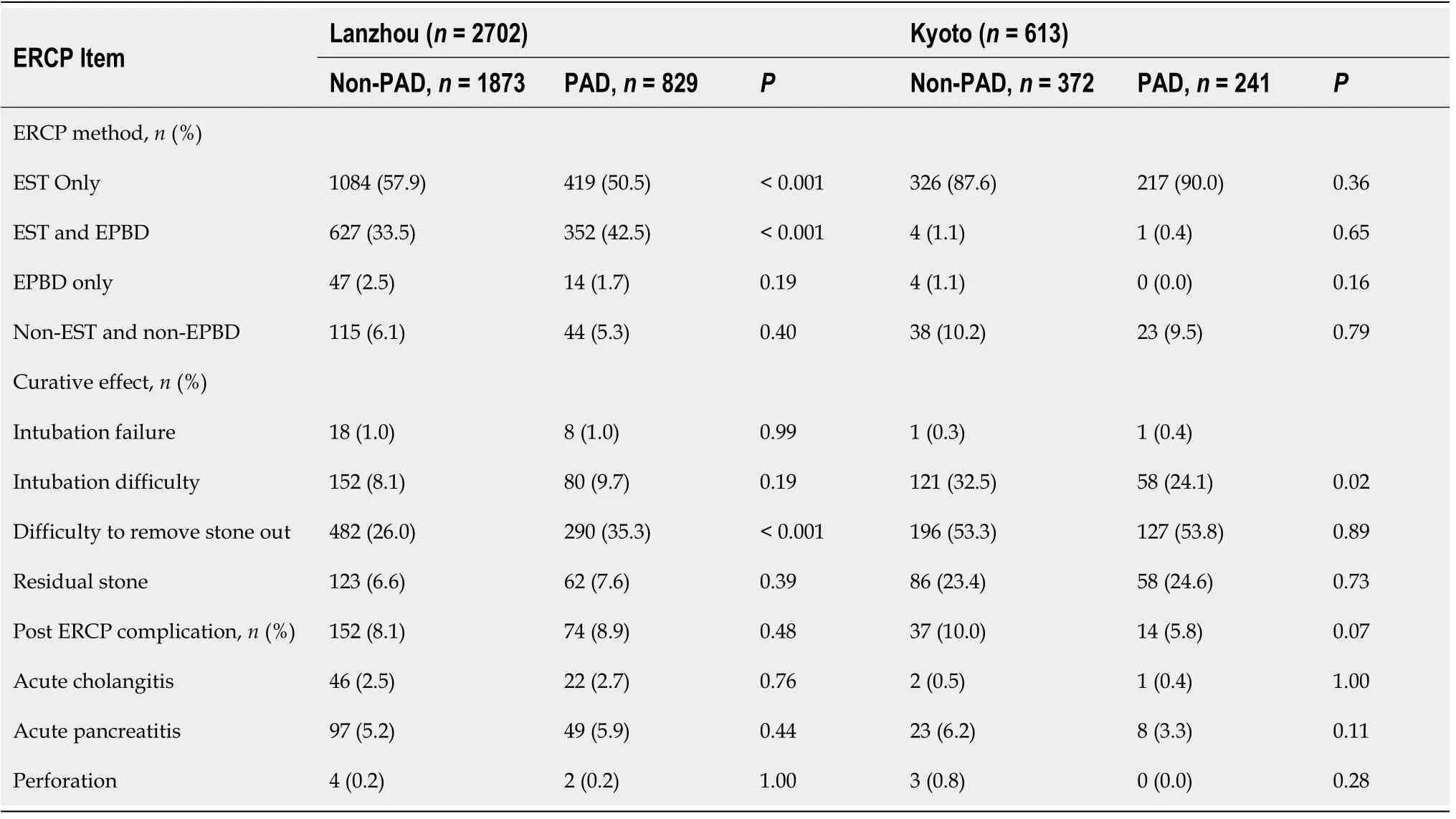
Table 4 Comparison of endoscopic retrograde cholangiopancreatography related contents of choledocholithiasis patient with and without periampullary diverticulum in Lanzhou or Kyoto
DlSCUSSlON
PADs are extraluminal mucosal outpouchings of the duodenum that arise within a radius of 2-3 cm from the ampulla of Vater[6].Patients with PAD often have slow biliary excretion and bile stasis due to mechanical pressure from the PAD to the distal end of the biliary tract.Additionally,PAD is often accompanied by duodenobiliary reflux and subsequent bacterial infection because of sphincter of Oddi dysfunction.These are potential reasons that PADs are clinically associated with biliary stones in many studies[16-20].However,it is unknown what the characteristics of choledocholithiasis with PAD are from different regions.In our study,we found that the clinical characteristics of PAD patients with choledocholithiasis were significantly different between the Lanzhou center and Kyoto center.
The results showed that comorbid diseases,such as acute cholangitis,obstructive jaundice,and acute pancreatitis,were more common in the Lanzhou center than in the Kyoto center for PAD patients with choledocholithiasis.Our study showed that the average diameter of the CBD was 14.8 ± 5.2 mm in Lanzhou and 11.6 ± 4.2 mm in Kyoto,with a significant difference(P< 0.001),and the reasons are not entirely clear.However,one of the reasons for these different kinds of characteristics may be attributed to the larger stone size and multiple stone numbers in the CBD in patients in the Lanzhou centercompared to the Kyoto center.Actually,the results revealed that the mean diameter of the stone size was 12.2 ± 6.5 mm in Lanzhou and 8.2 ± 5.3 mm in Kyoto,and the rate of multiple stones was 45.3% in Lanzhou,and only 20.3% in Kyoto,both withP< 0.001.Therefore,larger and multiple stones in the CBD would contribute to a dilated CBD,acute cholangitis and obstructive jaundice,and even to acute pancreatitis.Also,the reasons why the CBD stones were more abundant and larger in Lanzhou Center than in Kyoto Center are unknown.However,biliary duct stones are usually associated with the environment and metabolic diseases such as being overweight,obesity,diabetes and hyperlipidemia[21-23].There are many different characteristics in dietary habits and geographical environments,even in metabolic diseases,between the Lanzhou center in China and the Kyoto center in Japan.
Non-PAD choledocholithiasis was used as a control,and the characteristics of choledocholithiasis with PAD within each center were further analyzed.We noticed that in the Lanzhou center,the clinical characteristics,including mean age,sex,mean size of the choledocholithiasis,single or multiple choledocholithiasis,diameter of the CBD,and concomitant diseases,such as acute cholangitis,obstructive jaundice,and gallbladder stones,differed significantly between the choledocholithiasis cases with PAD and without PAD.However,in the Kyoto center,excluding the mean age,the abovementioned clinical characteristics were not significantly different between choledocholithiasis cases with PAD and without PAD.These results indicated that PADs were associated with different clinical characteristics in patients with CBD stones in the Lanzhou center,but these characteristics were not seen in the Kyoto center.It was difficult to explain the outcome,but it confirmed that there is actually a difference in the characteristics of choledocholithiasis patients with PAD and without PAD from different regions.Ham JHet al[24]reported that PAD induces marked postcholecystectomy CBD dilatation.Kim CWet al[25]suggested that acute cholangitis patients with PAD had larger CBD stones and more severe cholangitis than those without PAD.However,Lee JJet al[26]demonstrated that PAD alone does not lead to abnormal biliary dilatation in age- and sex-matched control groups.Therefore,choledocholithiasis with PAD had different clinical characteristics between Lanzhou and Kyoto.The different geographical environments,lifestyles,dietary habits,and health consciousness may contribute to the clinical characteristics.
ERCP is now a well-established standard method for removing choledocholithiasis,but it carries an 8%-12% risk of early complications,such as bleeding,duodenal perforation,and pancreatitis[17-18].If the duodenal papilla opens intra-PAD or is very close to the PAD,the appearance,shape,and orifice of the duodenal papilla will be changed anatomically[25].This kind of change likely leads to a higher risk and is more difficult to EST because the EST direction may deviate from the long axis of the CBD and the length available for EST is not enough.Under the condition of an insufficient length for the EST,the difficulty rate of removing large choledocholithiasis and residual rate of the stone will increase,and mechanical lithotripsy will probably be needed.In 2003,Ersoz Get al[27]first reported that EST followed by sequential EPBD using a 12-20 mm diameter balloon may be effective for difficult removalsof large bile duct stones,and the rate of early complications was acceptable.Weinberg BMet al[28]reported that an additional EST after EPBD was also required in 10%-19% of patients because the biliary opening was not sufficiently enlarged.After that report,several studies established that procedure as an effective and safe treatment for removing difficult-to-extract bile duct stones[29-31].Kim HWet al[32]reported that the overall successful stone removal rate and the complication rate did not differ significantly between the PAD and control groups when applying limited EST plus large balloon dilation.Our previous study,a multicenter,randomized controlled trial,suggested that a balloon dilation time of 30 s for combined EST reduced the frequency of post-ERCP pancreatitis[33].In addition,the Guideline of the European Society of Gastrointestinal Endoscopy strongly recommends EPBD as an alternative to EST for extracting choledocholithiasis < 8 mm in patients,especially in the presence of altered anatomy[34].Therefore,there are now at least three methods(EST,EPBD,and EST plus EPBD)available to treat choledocholithiasis with PAD.
In our research,EST(50.5%),EST+EPBD(42.5%),and EPBD(1.7%)were adopted in the Lanzhou center,while EST(90.0%),EST+EPBD(0.4%),and EPBD(0.0%)were applied in the Kyoto center.Thus,the ERCP procedures were significantly different between the two centers.One of the main reasons for this distinction is the different clinical characteristics of choledocholithiasis with PAD mentioned above between Lanzhou and Kyoto.In other words,different ERCP methods are naturally based on patients’clinical characteristics.
Because of the different ERCP procedures between the Lanzhou and Kyoto centers,the efficacy of ERCP in each center needed to be compared.In the Kyoto center,owing to its own lack of different characteristics,such as the mean size of CBD stones(7.5 ± 5.2 mm,non-PAD;8.2 ± 5.3 mm,PAD;P=0.11),multiple stones(19.0%,non-PAD;20.3% PAD;P= 0.69),there was no significant difference in efficacy between the patients with and without PAD(rate to remove choledocholithiasis difficulty,P=0.89;residual rate of bile duct stones,P= 0.73).However,in the Lanzhou center,with differences in the clinical characteristics,such as the mean size of the CBD stones(10.3 ± 5.4 mm,non-PAD;12.2 ± 6.5 mm,PAD;P< 0.001),multiple stones(39.0%,non-PAD;45.3% PAD;P= 0.002),the difficulty rate of removing choledocholithiasis was significantly different(P< 0.001).However,if EST+EPBD was adopted,the residual rate of bile duct stones was not significantly different(P= 0.39)between choledocholithiasis patients with and without PAD.Therefore,to reach an appropriate efficacy,the ERCP procedure depends on the different clinical characteristics of choledocholithiasis patients with PAD.Interestingly,although different therapeutic ERCP procedures were employed in the Lanzhou and Kyoto centers,the overall post-ERCP complications were not significantly different for choledocholithiasis with PAD not only between Lanzhou and Kyoto centers(P= 0.12)but also within each center(Lanzhou,P= 0.48;Kyoto,P= 0.07).Thus,we confirmed that PAD did not increase ERCP-related complications when using an experienced endoscopist.
CONCLUSlON
In conclusion,many clinical characteristics of choledocholithiasis patients with PAD were significantly different between the Lanzhou center and Kyoto center.Choledocholithiasis with PAD had more complexity with larger and multiple stones,wider diameter of the CBD,and more biliary duct comorbidities in the Lanzhou center compared to the Kyoto center.In the internal center analysis,the clinical characteristics mentioned above were also different between the PAD and non-PAD groups in the Lanzhou center but not in the Kyoto center.Different ERCP procedures to manage native duodenal papilla were adopted naturally depending on the clinical characteristics of choledocholithiasis with PAD to approve efficacy between the Lanzhou and the Kyoto centers.Although there was increased difficulty removing stones in the Lanzhou Center and an increased difficulty in removing deep cannulates in the Kyoto centers,the stone residual rate was not significantly different within each center for choledocholithiasis with PAD,and post-ERCP complications were also not significantly different between the two centers or within each center.Nevertheless,there are some shortcomings in this study,such as the role of different ERCP procedures in the recurrence of choledocholithiasis,which needs to be confirmed by further subsequent research.
ARTlCLE HlGHLlGHTS
Research background
Most of study regarding periampullary diverticulum(PAD)impact on endoscopic retrograde cholangiopancreatography(ERCP)therapy for choledocholithiasis based on data from one endoscopy center and there were inconsistent conclusions of the PAD impacts on safety and post ERCP complications for choledocholithiasis.
Research motivation
What did cause the different conclusions of PAD impacts on post ERCP complications and safety for choledocholithiasis? UP to now,the real reason is little known and lacked to compare the clinical characteristic of choledocholithiasis with PAD from different geographical endoscopy centers.
Research objectives
To compare the clinical characteristics of choledocholithiasis with PAD between two regional endoscopy centers and analyze the efficacy of clinical characteristics on ERCP procedures for choledocholithiasis patients with PAD.
Research methods
Patients underwent ERCP treatment at first time between January 2012 and December 2017 were Involved.The clinical characteristics and ERCP related contents of choledocholithiasis with PAD were compared between Lanzhou center and Kyoto center.Furthermore,Choledocholithiasis without PAD as control,analyzed the clinical characteristic and ERCP therapy of Choledocholithiasis with PAD internal each center.
Research results
829 out of 3608 patients in Lanzhou center and 241 out of 1198 in Kyoto center suffered from
choledocholithiasis with PAD.The overall clinical characteristics were significantly different excepting the gender between the two centers.Non-PAD choledocholithiasis as control,in Lanzhou center,many clinical characteristics of patients were significant difference between non-PAD and PAD(P= 0.03 -<0.001),but were no difference in Kyoto center(each withP> 0.05).
For choledocholithiasis with PAD patients,ERCP procedures to handle the duodenal papilla were significant different Lanzhou center and Kyoto center(P< 0.001).But the overall post-complication was no significant different between two centers(8.9% in Lanzhou center,5.8% in Kyoto center.P= 0.12).
The difficult rate to remove stone,in Lanzhou center,was 35.3% and 26.0% in PAD group and non-PAD group,with a significant difference between two groups(P< 0.001),while it accounted for 53.8%and 53.3% in PAD group and non-PAD group in Kyoto center,with no significant difference between two groups.However,residual rate of choledocholithisasis was no significant difference between two groups in each center.Meanwhile,there were also no significant differences of post-ERCP complications between PAD and non-PAD patients within each center.
Research conclusions
Many clinical characteristics of choledocholithiasis patients with PAD were significant difference between Lanzhou and Kyoto.Patients carried characteristics with larger and multiple stones,wider diameter of CBD,and more possibility of acute cholangitis and obstructive jaundice in Lanzhou center than those in Kyoto.ERCP procedures to cope with native duodenal papilla were different between Lanzhou and Kyoto,depended on its own different clinical characteristics of choledocholithiasis with PAD.The efficacy and post-ERCP complications were no significant differences for choledocholithiasis with PAD in each own center.The overall post-ERCP complication was no statistics difference between two centers as well.
Research perspectives
The control study of multiple endoscopy centers from different region is worthy of conducting to uncover the characteristics of choledocholithiasis patients with PAD and their influences on therapy ERCP.The role of different ERCP procedures for recurrence of choledocholithiasis need to be confirmed through further subsequent research or prospective studies.
FOOTNOTES
Author contributions:Zhu KX,Yue P,Suzuki A,Tanaka K,Li X designed the research protocol;Zhu KX,Yue P,Meng WB,Zhang L,Zhu XL,Zhang H,Miao L,Wang ZF,Zhou WC,Suzuki A,Tanaka K,Li X were responsible for patient enrollment and data acquisition;Zhu KX,Yue P,Wang HP,Tanaka K contributed to data analysis and interpretation;Zhu KX,Yue P wrote the original manuscript;Zhu KX,Yue P,Meng WB,Liu JK,Li X contributed to critical revision of the manuscript for important content;Wang HP,Liu JK contributed to statistical analysis for this study;Li X contributed to final approval of the article.
lnstitutional review board statement:The study was reviewed and approved by the First Hospital of Lanzhou University Institutional Review Board(Approval No.LDYYLL 2021-192).
Conflict-of-interest statement:The authors declare that they have no conflicts of interest to disclose.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See:https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Ke-Xiang Zhu 0000-0003-4272-5221;Ping Yue 0000-0001-8736-949X;Hai-Ping Wang 0000-0003-2055-8936;Wen-Bo Meng 0000-0002-9355-0225;Jian-Kang Liu 0000-0003-2454-8209;Lei Zhang 0000-0001-9320-304X;Xiao-Liang Zhu 0000-0002-5697-9583;Hui Zhang 0000-0003-0728-9188;Long Miao 0000-0002-7861-6134;Zheng-Feng Wang 0000-0002-4556-9247;Wen-Ce Zhou 0000-0002-0529-7777;Azumi Suzuki 0000-0002-6041-7719;Kiyohito Tanaka 0000-0002-9189-1755;Xun Li 0000-0001-6862-7692.
S-Editor:Chang KL
L-Editor:A
P-Editor:Chang KL
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Surgery for Cronkhite-Canada syndrome complicated with intussusception:A case report and review of literature
- Status of bariatric endoscopy–what does the surgeon need to know?A review
- lmpact of parenchyma-preserving surgical methods on treating patients with solid pseudopapillary neoplasms:A retrospective study with a large sample size
- Laparoscopic vs open total gastrectomy for advanced gastric cancer following neoadjuvant therapy:A propensity score matching analysis
- Nomograms predicting prognosis of patients with pathological stages T1N2-3 and T3N0 gastric cancer
- Long-term outcomes of postgastrectomy syndrome after total laparoscopic distal gastrectomy using the augmented rectangle technique
