The L-shaped association between superoxide dismutase levels and blood pressure in older Chinese adults: community-based,cross-sectional study
2022-02-26YingHUANGWeiLAIHongCHENQiFanLIUJuXiangLIJinZhuHU
Ying HUANG, Wei LAI, Hong CHEN, Qi-Fan LIU, Ju-Xiang LI✉, Jin-Zhu HU✉
Department of Cardiovascular Medicine, the Second Affiliated Hospital of Nanchang University, Nanchang of Jiangxi,China
*The authors contributed equally to this manuscript Correspondence to: jx912@126.com; hujinzhu1983@sina.com https://doi.org/10.11909/j.issn.1671-5411.2022.01.002
ABSTRACT
Hypertension is the most important risk factor for death from cardio-cerebral vascular diseases, accounting for 2.54 million deaths among Chinese residents in 2017.[1,2]Although many risk factors for hypertension, including genetics, age, overweight/obesity, high salt intake, smoking, excessive alcohol consumption, insufficient physical activity, chronic mental stress and air pollution, have been identified,[3,4]the incidence rate of hypertension is increasing year by year,suggesting that some potential risk factors are still unknown.Therefore, continuing to find modifiable risk factors or predictors has important clinical value for the early prevention of hypertension.
The role of reactive oxygen species (ROS) in the development of hypertension has been previously investigated.When the vascular structure changes,it can promote the tension of blood vessels to change,affect the development of the whole course of hypertension and lead to irreversible pathological changes.[5]ROS can induce the transition of vascular smooth muscle cells (VSMCs) to a proliferative phenotype, which is characterized by a decrease in the vascular lumen, an increase in medium thickness, an increase in stiffness and a decrease in expandability.[6]ROS also promote inflammatory gene expression and mediate multiple signaling pathways leading to vascular remodeling.[7,8]Cells have multiple integrated enzymatic and nonenzymatic antioxidant systems to resist oxidative stress.Superoxide dismutase (SOD) was discovered by McCord and Fridovich in 1969 and has a scavenging effect on ROS.[9]Oxidative stress occurs in the kidney and its vascular system during Ang II infusion and high salt intake, which reduces the expression of SOD.[10,11]SOD plays an important role in endothelial dysfunction in essential hypertension by competing with nitric oxide for superoxide.[12]The pathogenesis of hypertension is related to oxidative stress and endothelial dysfunction, accompanied by changes in serum SOD levels.
Although several previous studies have reported a decreased level and/or low activity of SOD in animal models and/or humans with hypertension,[12,13]the concrete relationship between SOD level and hypertension is still uncertain.Given the increasing aging of the population and the continuing rise in the prevalence of hypertension, we aimed to investigate whether serum concentrations of SOD contributed to a changed risk of hypertension in a Chinese elderly population.
METHODS
Study Design and Participants
The data for this study were from the Chinese Longitudinal Healthy Longevity Survey (CLHLS),which covers 22 provinces, municipalities and autonomous regions across the country.The subjects were people aged 65 and above.Overall, the national cohort was conducted among an elderly population, with high-quality demographic and socioeconomic characteristics, social and behavioral risk factors, and various biochemical indicators, such as blood and urine tests, for health indicators.The baseline wave was conducted in 1998, followed by follow-up waves in 2000, 2002, 2005, 2008-2009,2011-2012 and 2014, and a multistage cluster sampling method was used.Details of the study have also been described elsewhere[14].
In the first stage, samples were randomly selected from the included provinces (Hebei, Heilongjiang, Henan, Jilin, Shandong, Liaoning, Shaanxi,Shanxi, Sichuan, Hubei, Anhui, Jiangxi, Jiangsu,Fujian, Zhejiang, Hunan, Guangdong, Guangxi,Beijing, Tianjin, Chongqing and Shanghai).The total population of these cities and counties accounts for 85% of the total Chinese population.In the second stage, the response rate was 97.7% for all participants who lived in the sampled counties and cities and were willing to participate in the cohort.A trained staff member from the county centers for disease control and prevention conducted interviews using a structured questionnaire for acquisition of information.The questionnaire data came from participants or surrogate interviewees who were usually close relatives and family members.More details on the research design, research procedures and data quality assessment are described elsewhere.[14-16]Participants in the national cohort did not participate in the design of the self-reporting questionnaire in the CLHLS study at the same time.These participants were also not involved in the implementation of our study.All participants or their relatives were informed of the results of systolic BP (SBP) and diastolic BP (DBP) used the data for the CLHLS study.
In this study, we used data from the 2011-2012 wave of the cohort.During the wave, the biomarker sub-study of CLHLS was conducted for various serum indexes including SOD and others.Our study had a sufficient analysis among adults aged 65 and older in the wave with complete information on BP, SOD and other covariates.In total, 1,630 participants were initially included in our study.As shown in Figure 1, we excluded 809 participants due to missing data.
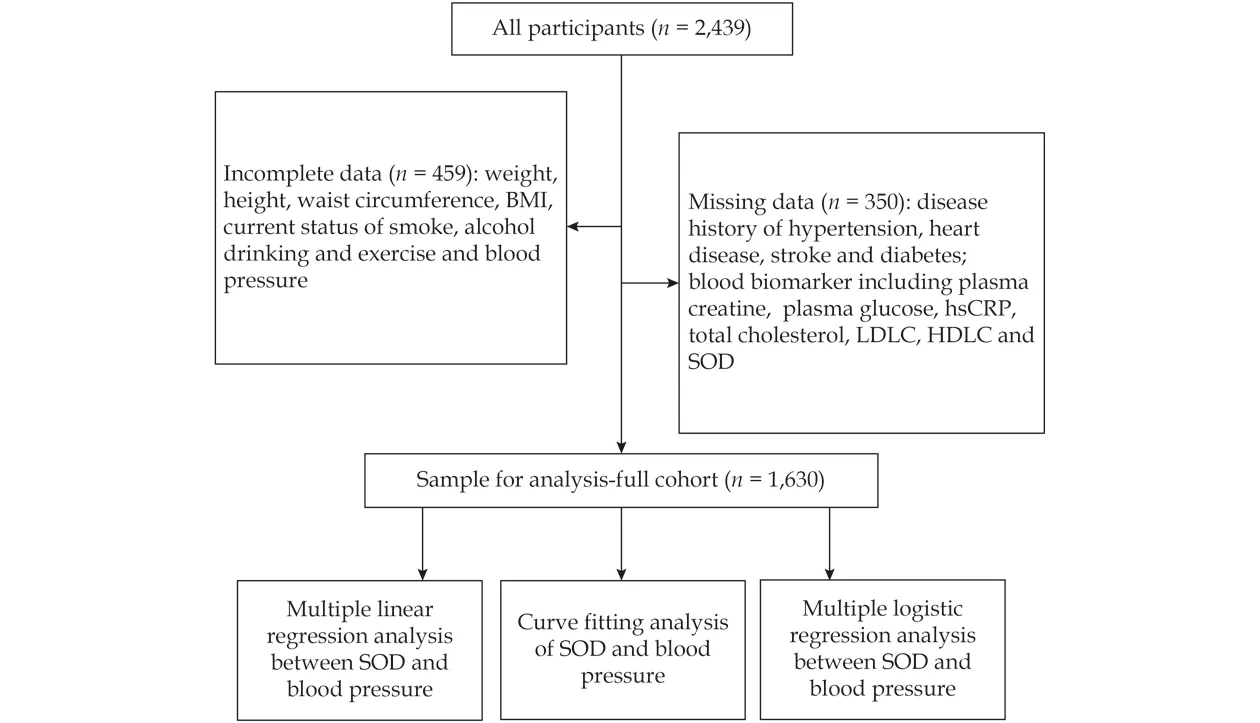
Figure1 Flow chart of included participants.BMI: body mass index; HDLC: high density lipoprotein cholesterol; hs-CRP: hypersensitive-C-reactive-protein LDLC: low density lipoprotein cholesterol; SOD: serum superoxide dismutase.
Measurement and Calculation of Blood Pressure
All participants rested for at least 5 min, and trained research assistants used a mercury sphygmomanometer (upper arm type; Yuyue, Jiangsu,China).SBP was measured by Korotkoff phase I and DBP was measured by phase V.The BP of bedridden patients was measured in the recumbent position.The average value of BP was calculated from two measurements for further analysis.The mercury sphygmomanometer must be calibrated before each measurement.For research purposes,DBP ≥ 90 mmHg was defined as diastolic hypertension and SDP ≥ 140 mmHg was defined as systolic hypertension.
Covariates
The covariates were obtained by structured questionnaire.Sociodemographic characteristics included age, sex, residence and marital status.Other health features included smoking, drinking, activities of daily living, body mass index (BMI), waist circumference, and physician-diagnosed self-reported diseases such as heart disease, stroke, diabetes, and other cardiovascular diseases (CVDs).
Residence is divided into “urban (city or town)”or “rural (rural housing)”.Current smokers and current drinkers were reported by themselves, using “Are you smoking at the moment?” and “are you drinking now?” Current smokers were divided into “current smokers” and “noncurrent smokers”.At present, drinkers were divided into “current drinkers” and “noncurrent drinkers”.Daily life activities can be divided into the following two categories: “regular exercise” and “irregular exercise”.Self-reported diseases can be divided into the following two categories: “yes” and “no”.The waist circumference of lightweight participants were measured with an non-stretchable tape.Measure the distance between the lowest rib and the iliac crest.In the case of our study, if the waist circumference of a participant was at least 80 cm for a woman and at least 85 cm for a man, she or he was defined as overweight.BMI was calculated as weight (kg)divided by height squared (m2).BMI ≥ 25 kg/cm2,was defined as overweight.
Statistical Analysis
The Kolmogorov-Smirnov test was used to analyze the normality of the data.Non-normally distributed were analyzed by the Mann-WhitneyUtest and then expressed as the median (interquartile range [IQR]).Normally distributed data were analyzed by the independentt-test and presented as the mean ± SD.The chi-square test was used to analyze categorical variables and is expressed asn(%).
First, we implemented a smooth curve to estimate the relationships of serum SOD levels with SBP and DBP.Second, multiple linear regression analysis was performed to evaluate the associations between serum SOD and SBP and DBP.Third, multiple logistic regression analysis was also performed to evaluate the relationships between SOD and systolic hypertension (SBP ≥ 140 mmHg) and diastolic hypertension (DBP ≥ 90 mmHg).Additionally, we implemented a multiple logistic regression analysis to estimate the relationship between SOD and systolic hypertension (SBP ≥ 140 mmHg) and diastolic hypertension (DBP ≥ 90 mmHg) stratified by sex,overweight, category of residence, CVDs and SOD levels (inflection point = 58 IU/mL).Additionally,stratified analysis performed by gender, BMI, waist circumference, category of residence, disease history and inflection point of serum SOD.We used four models.Model 1: adjusted for age and gender.Model 2: adjusted for age, sex, current status of smoking, alcohol consumption and exercise.Model 3:adjusted for age, sex, current status of smoking, alcohol consumption, exercise and disease history(diabetes stroke and heart disease).Model 4: adjusted for age, sex, current status of smoking, alcohol consumption, exercise, disease history (diabetes,stroke and heart disease), BMI and blood biomarkers (total cholesterol, low density lipoprotein cholesterol (LDLC), high density lipoprotein cholesterol(HDLC), hypersensitive-c-reactive-protein (hs-CRP), creatine and plasma glucose).All of the analyses were performed using EmpowerStats 3.0.APvalue ≤ 0.05 was considered to be statistically significant.
RESULTS
Characteristics of Participants
The present study included 1,630 participants,with an average age of 84, and 839 participants were female (51.5%).The median SBP and DBP were 140.0 mmHg and 80 mmHg, respectively.The median serum SOD levels of the included participants were 57.51 IU/mL in Table 1.
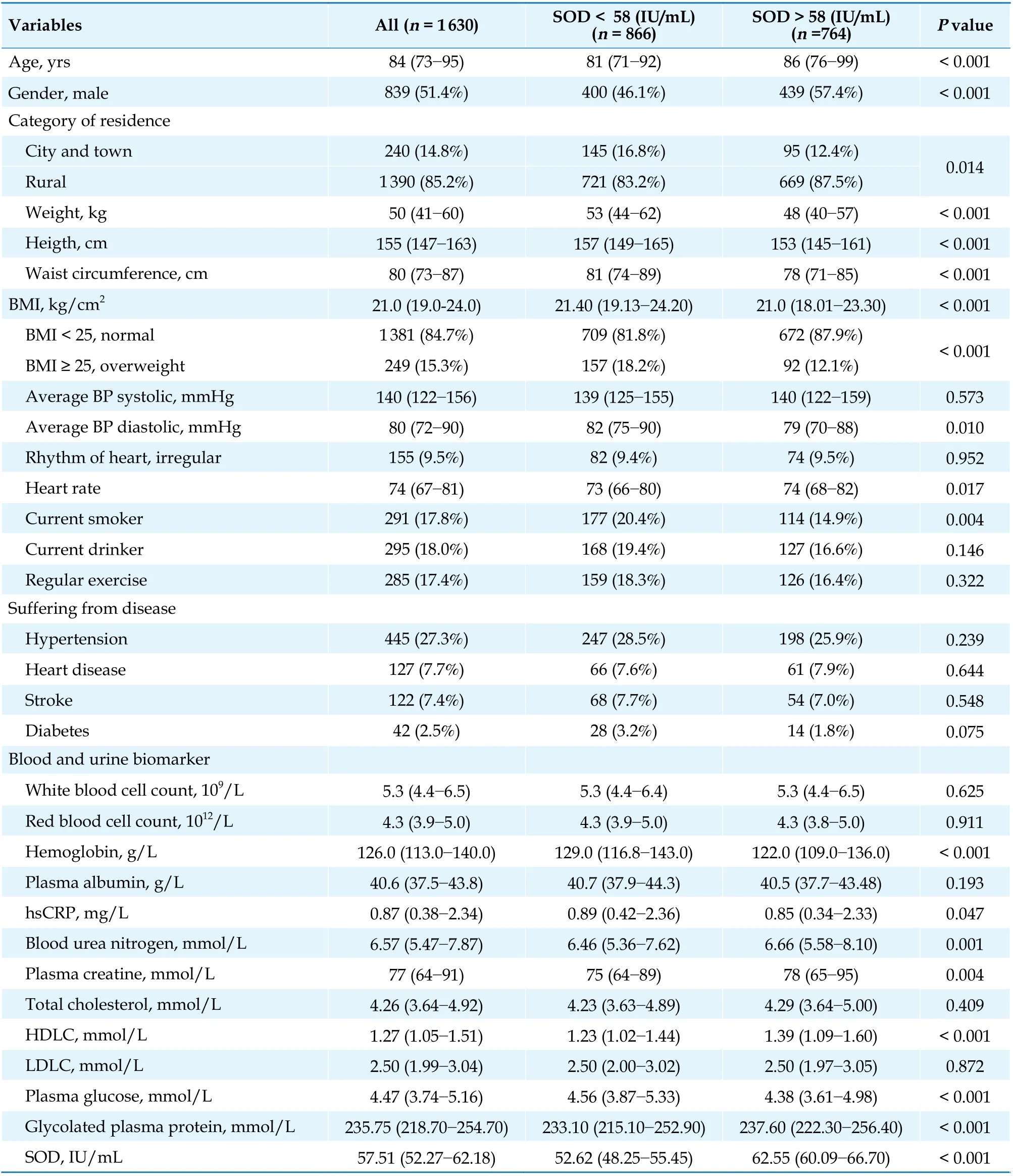
Table1 Characteristics of participants.
Nonlinear associations were identified between serum SOD and DBP before adjustment for any confounding factors.The smooth curve supported an L-shaped relationship between serum SOD levels and DBP (Figure 2A,P< 0.001) but not with SBP (Figure 2B,P> 0.05).DBP decreased with increasing serum SOD levels up to the turning point(SOD = 58 IU/mL).However, DBP was not correlated with SOD levels when SOD > 58 IU/mL.Similarly, there was an L-shaped relationship between serum SOD levels and the risk of diastolic hypertension (Figure 2C,P< 0.001) but not with the risk of systolic hypertension (Figure 2D,P> 0.05).The risk of diastolic hypertension decreased with increasing serum SOD levels up to the turning point (SOD = 58 IU/mL).Furthermore, all included participants were divided into two groups according to the inflection point of serum SOD levels (58 IU/mL).Compared with participants with low serum SOD levels (serum SOD < 58 IU/mL), high serum SOD levels participants (serum SOD > 58 IU/mL) had significantly lower DBP instead of SBP.We observed a significantly gradual downward trend in associations between serum SOD levels and DBP when SOD < 58 IU/mL, while there were no associations between serum SOD levels and DBP when SOD > 58 IU/mL (Figure 3A).Interestingly, similar results showed a significant gradual downward trend in associations between serum SOD levels and the risk of diastolic hypertension when SOD <58 IU/mL (Figure 3B).
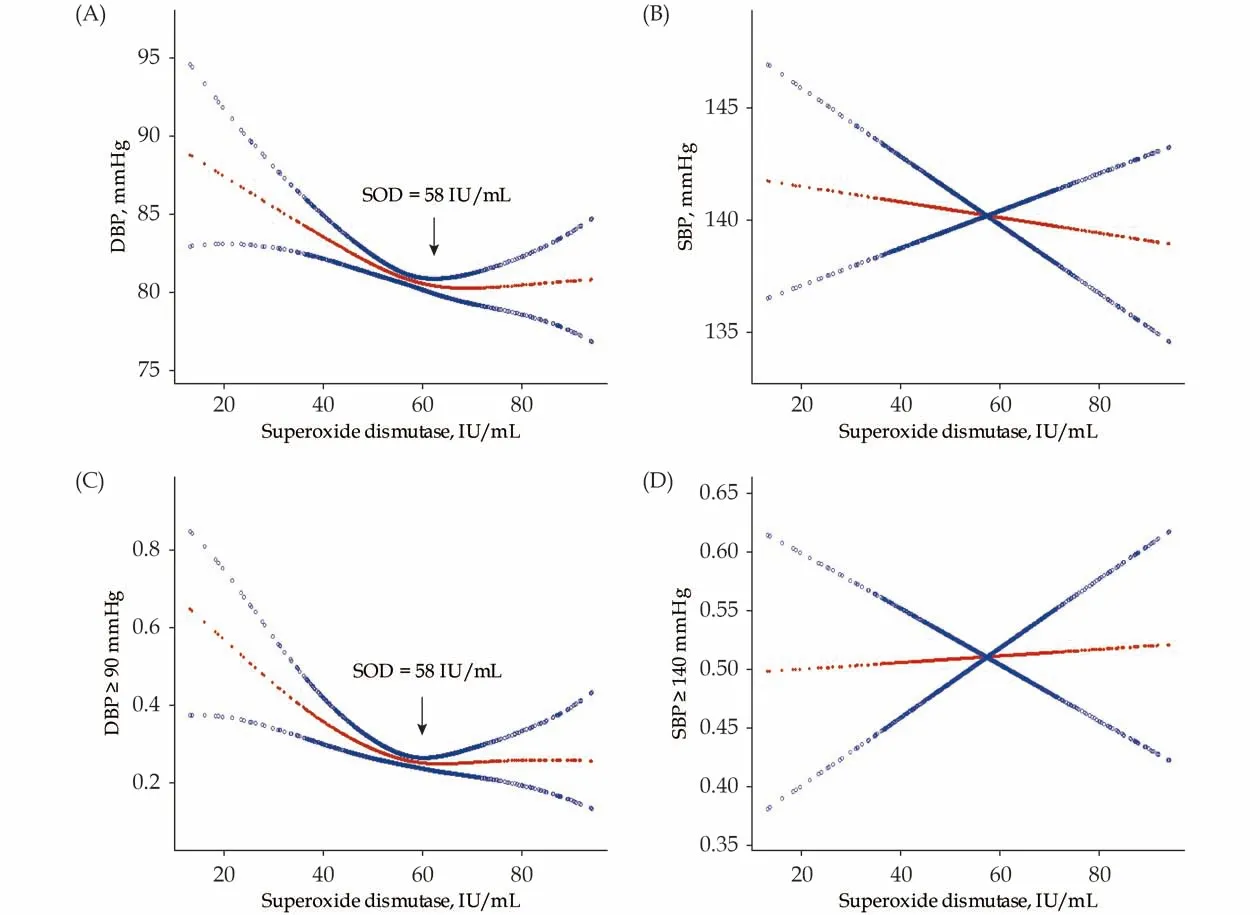
Figure2 Smooth curve on associations between SOD levels and diastolic (A & C) and systolic (B & D) blood pressure respectively.DBP: diastolic blood pressure; SBP: systolic blood pressure; SOD: serum superoxide dismutase.
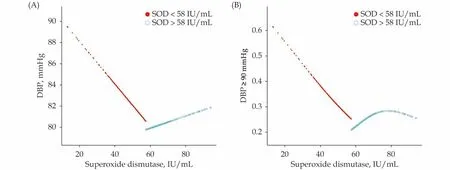
Figure3 SStratified analysis on association between SOD levels and diastolic blood pressure (A) and diastolic blood pressure ≥90 mmHg (B).DBP: diastolic blood pressure; SOD: serum superoxide dismutase.
Association between Serum SOD and BP After Adjusting for Confounding Factors
Multiple linear regression analysis was performed to further prove the association between serum SOD and BP.As shown in Table 2, serum SOD was negatively correlated with DBP (Sβ =-0.088; 95% CI: -0.170 to -0.049;P< 0.001) but not with SBP (Sβ = 0.013; 95% CI: -0.086, 0.147;P=0.607) in Crude Model.After other confounding factors were added, including age, gender, current status of smoke, alcohol drinking, exercise, disease history (diabetes, stroke and heart disease), BMI and blood biomarkers (total cholesterol, LDLC,HDLC, hs-CRP, creatine and plasma glucose), the serum SOD still had a strong relationship with DBP(Sβ = -0.069; 95% CI: -0.151 to 0.026,P= 0.005,Model 4) but not with SBP (Sβ = 0.014, 95%CI:-0.153 to 0.084,P= 0.564, Model 4).However, there was still no correlation between serum SOD and SBP after these adjustments were made.

Table2 Multiple linear regression analysis for relationship between SOD and BP.
Association between Serum SOD and Hypertension After Adjusting for Confounding Factors
Multiple logistic regression analysis was performed to further prove the association between serum SOD and the risk of hypertension.As shown in Table 3, the results suggested that serum SOD was independently associated with the risk of diastolic hypertension (OR = 0.984; 95% CI: 0.973-0.996;P= 0.01; Model 4) after adjustments were made, including for age, gender, current status of smoke, alcohol drinking, exercise, disease history(diabetes, stroke and heart disease), BMI and blood biomarkers (total cholesterol, LDLC, HDLC, hs-CRP, creatine and plasma glucose).Our resultsshowed that serum SOD was not associated with the risk of systolic hypertension (1.001; 95% CI:0.990-1.012;P= 0.836, Model 4) after adjusting for relevant confounding factors.

Table3 Multiple Logistic Regression Analysis for Relationship between SOD and High BP (DBP ≥ 90 mmHg or SBP ≥ 140 mm-Hg).
Stratified Analysis for Association between Serum SOD and BP by Multiple Linear Regression Analysis
Multiple linear regression analysis was performed to further prove the association between serum SOD and BP stratified by sex, overweight,category of residence and disease history.As shown in Table 4, we observed no significant effect modifiers between serum SOD and DBP after stratifying the analysis by sex (interactionP= 0.539 4), BMI (in-teractionP= 0.519 2), waist circumference (interactionP= 0.0.723 3), category of residence (interactionP= 0.921 3), heart disease (interactionP= 0.453 6),stroke (interactionP= 0.074 1) and diabetes (interactionP= 0.662 7).We also observed no significant effect modifiers between serum SOD and SBP after stratification of the analysis.Importantly, serum SOD levels (< 58 IU/mL, > 58 IU/mL) were an effect modifier of the association between serum SOD and DBP (interactionP= 0.006 0) but not a modifier of the association between serum SOD and SBP (interactionP= 0.600 8).

Table4 Multiple linear regression analysis for relationship between SOD and blood pressure stratified by gender, overweight,category of residence and CVD diseases.
Stratified Analysis for Association between Serum SOD and Risk of Hypertension by Multiple Logistic Regression Analysis
Multiple logistic regression analysis was performed to further prove the association between serum SOD and hypertension stratified by sex, overweight, category of residence and disease history.As shown in Table 5, we observed no significant effect modifiers between serum SOD and the risk of diastolic hypertension after the stratified analysis by sex (interactionP= 0.132 7), BMI (interactionP=0.142 2), waist circumference (interactionP= 0.309 5),category of residence (interactionP= 0.128 2), heart disease (interactionP= 0.964 2), stroke (interactionP= 0.712 8) and diabetes (interactionP= 0.162 1).We also observed no significant effect modifiers between serum SOD and SBP after the stratified analysis.Similarly, serum SOD levels (< 58 IU/mL,> 58 IU/mL) were an effect modifier of the association between serum SOD and the risk of diastolic hypertension (interactionP= 0.005 0) but not a modifier of the association between serum SOD and the risk of systolic hypertension (interactionP= 0.762 5).

Table5 Multiple logistics regression analysis for relationship between SOD and blood pressure stratified by gender, overweight,category of residence and CVD diseases.
DISCUSSION
In this prospective cohort including 1 630 Chinese adults 65 years or older, our results indicated Lshaped relationships between serum SOD levelsand DBP and diastolic hypertension after important identified confounders were adjusted.The inflection point for the curve was found to be a serum SOD level of 58 IU/mL.To the best of our knowledge,this is the first study in a Chinese elderly population to provide clear evidence of the association between serum SOD levels and diastolic hypertension.
In recent years, it has been found that oxidative stress plays an important role in the pathogenesis of hypertension by activating the renin-angiotensin-aldosterone system (RAAS).[17,18]SOD is an antioxidant enzyme that protects against oxidative stress by catalyzing the dismutation of superoxide anion(O2·-) into hydrogen peroxide and oxygen.[19]Some studies have shown that level and/or activity of SOD were decreased in animal models and/or humans with hypertension.[12,13,19-21]One study demonstrated that in newly diagnosed hypertensive patients without antihypertensive treatment, SOD levels were lower than those in the normal population, and SOD activity was negatively correlated with both systolic and diastolic blood pressure.[22]SOD3 is closely linked to hypertension among the three SOD isoenzymes because SOD3 plays a key role in regulating O2·-levels in the vasculature.Gongora,et al.[20]found that hypertension caused by angiotensin II was greater in Sod3-/-mice compared with wild-type mice.However, none of these studies clarified the relationship between different serum SOD levels and hypertension.
In the present study, our results indicated thatserum SOD levels are associated with the risk of diastolic hypertension, and a linear regression model with a smooth curve further showed an L-shaped relationship between serum SOD levels and the risk of diastolic hypertension, while there was no correlation between serum SOD levels and the risk of systolic hypertension.A previous study did not indicate any shaped associations between serum SOD levels and hypertension.Importantly, we found the inflection point for the curve at a serum SOD level of 58 IU/mL, the risk of diastolic hypertension decreased with the increase of serum SOD levels up to the turning point, and the diastolic hypertension was not correlated with SOD levels at SOD > 58 IU/mL.On further analysis, we found that serum SOD levels (< 58 IU/mL, > 58 IU/mL) were an effect modifier of the association between serum SOD and DBP or the risk of diastolic hypertension but not a modifier of the association between serum SOD and SBP or the risk of systolic hypertension.In addition, no significant effect modifiers were found between serum SOD and DBP, SBP, or the risk of diastolic hypertension or systolic hypertension after the stratified analysis by sex, BMI, waist circumference, category of residence, heart disease, stroke and diabetes.According to the results, we can easily judge the risk of diastolic hypertension according to different SOD levels in patients.These findings may provide clinical guidelines on the primary prevention of diastolic hypertension for the Chinese elderly population.
The mechanism driving the link between serum SOD levels and hypertension has not been fully elucidated.The occurrence of diastolic hypertension is related to high sympathetic tension, increased excitability of the RAAS and increased peripheral vascular resistance.[23]In this study, we found that the risk of diastolic hypertension decreased with increasing serum SOD levels up to 58 IU/mL.This may be because SOD protects against oxidative stress, which may reduce diastolic blood pressure by antagonizing RAAS.When the concentration of serum SOD is greater than 58 IU/mL, the effect of SOD antioxidant stress may reach saturation, and the increase in SOD is not related to DBP.A previous study found that the occurrence of isolated diastolic hypertension is closely related to BMI,[24]but in our study, we observed no significant effect modifiers between serum SOD and diastolic hypertension after the stratified analysis by BMI.This difference may be caused by the following reasons: first,the inclusion of different groups of people, as our study included Chinese elderly people over 65 years old and the Framingham Heart Study[24]included people aged 28 to 62.Second, 84.7% of the participants included in our study were people with BMI < 25 kg/m2, and the number of people who were overweight was relatively small.Systolic hypertension is usually caused by decreased arterial system elasticity due to increased calcium and collagen deposition on the arterial wall.[25]The effect of SOD is not directly related to the above systolic hypertension mechanisms, which may explain our results that there was no relationship between serum SOD levels and the risk of systolic hypertension.Our findings suggest that increasing the concentration of serum SOD to a certain extent can reduce the risk of diastolic hypertension.A meta-analysis[26]indicated that tempol, a SOD mimetic, reduced BP and showed that antioxidant capacity played an important role in prevention after inducing hypertension in various animal models of hypertension.Further research is needed to identify drugs that can safely and effectively increase the level of human serum SOD for the treatment of hypertension.
Our study has some obvious strengths.First, our study results were from an elderly population of CLHLS, which is a prospective, longitudinal, community-based study.This is the first national cohort with an elderly Chinese population and has high-quality data, including demographic and socioeconomic characteristics, social and behavioral risk factors and enough biochemical indexes, with a multistage cluster sampling approach.Second, in this community-based cross-sectional study, for the first time, we found a nonlinear and L-shaped relationship between serum SOD levels and the risk of diastolic hypertension after adjusting for important identified confounders, and the inflection point for the curve was found to be a serum SOD level of 58 IU/mL.Third, enough confounding factors, including demographic characteristics, social and behavioral risk factors and biochemical indexes, were adjusted by correction analysis, which ensures the accuracy and reliability of our results.
This study also has some notable limitations.First, our data only contained the concentration of SOD in serum without SOD activity, which cannot reflect the role of SOD in a more comprehensive way.Second, the data did not distinguish between essential hypertension and secondary hypertension,and it was not possible to determine the relationship between serum SOD levels and these two types of hypertension.Third, the results of our study are only applicable to elderly individuals in China, and the effect of serum SOD levels on BP may be different between young individuals and elderly individuals.Fourth, all the blood tests in this study were only measured once at the same time (2011-2012).The time courses of SOD levels were not measured.Since there was no information about the long-term change in SOD levels, it may lead to inaccurate SOD levels, which may further bias our analysis results.Last, although more than 9,000 people were included in the CLHLS study and more than 2,000 people participated in blood biochemical testing,1,630 people were eventually included in our study because approximately 800 people were excluded due to lack of important variables.In addition, our study did not address some potential confounding issues that may be related to racial group differences, leading to some bias in the results.
In summary, our results indicated a L-shaped relationship between serum SOD levels and DBP or the risk of diastolic hypertension and found that the inflection point for the curve was a serum SOD level of 58 IU/mL.When the serum SOD level is lower than 58 IU/ml, the risk of diastolic hypertension decreases with increasing serum SOD levels and the risk does not decrease when SOD level is higher than 58 IU/mL.Our study suggests that increasing the level of serum SOD to a certain range to increase antioxidant stress is beneficial for the treatment of diastolic hypertension.
COMPETING INTERESTS
None.
RESEARCH FUNDING
This work was supported by grants from the National Natural Science Foundation of China (NSFC 81860070 and 82070350), JiangXi Province Science Foundation for Distinguished Young Scholar(20202ACBL216001) and Jiangxi Province’s Main Discipline Academic and Technical Leader Training Program-Leading Talent Project (20204BCJ22029).
杂志排行
Journal of Geriatric Cardiology的其它文章
- Atrial fibrillation in older adults with cancer
- Vectorcardiographic QRS area as a predictor of response to cardiac resynchronization therapy
- Electrocardiographic markers of cardiac resynchronization therapy response: delayed time to intrinsicoid deflection onset in lateral leads
- Novel electrocardiographic dyssynchrony criteria that may improve patient selection for cardiac resynchronization therapy
- Evolving concept of dyssynchrony and its utility
- Alcohol consumption in relation to the incidence of atrial fibrillation in an elderly Chinese population
