Evolving concept of dyssynchrony and its utility
2022-02-26PriyankaSatishBharatNarasimhanAndreasHagendorffBhupendarTayal
Priyanka Satish, Bharat Narasimhan, Andreas Hagendorff, Bhupendar Tayal,✉
1.Houston Methodist DeBakey Heart and Vascular Center, Houston, TX, USA; 2.Leipzig University Hospital, Department of Cardiology, Leipzig, Germany Correspondence to: bhupendar.tayal@gmail.com https://doi.org/10.11909/j.issn.1671-5411.2022.01.010
ABSTRACT The role of electromechanical dyssynchrony in heart failure gained prominence in literature with the results of trials of cardiac resynchronization therapy (CRT).CRT has shown to significantly decrease heart failure hospitalization and mortality in heart failure patients with dyssynchrony.Current guidelines recommend the use of electrical dyssynchrony based on a QRS > 150 ms and a left bundle branch block pattern on surface electrocardiogram to identify dyssynchrony in patients who will benefit from CRT implantation.However, predicting response to CRT remains a challenge with nearly one-third of patients gaining no benefit from the device.Multiple echocardiographic measures of mechanical dyssynchrony have been studied over the past two decade.However, trials where mechanical dyssynchrony used as an additional or lone criteria for CRT failed to show any benefit in the response to CRT.This shows that a deeper understanding of cardiac mechanics should be applied in the assessment of dyssynchrony.This review discusses the evolving role of imaging techniques in assessing cardiac dyssynchrony and their application in patients considered for device therapy.
Cardiac resynchronization therapy (CRT)was introduced as an experimental therapy in patients with severe symptomatic heart failure (HF) refractory to medical therapy,with evidence of conduction delay.[1]Over the years,many multicenter trails have consistently demonstrated the benefit of CRT among patients with significant HF symptoms with reduced left ventricular(LV) ejection fraction (EF) and a conduction block with wide QRS duration > 130 ms.[2-6]Not all patients with electrical dyssynchrony respond similarly to CRT and failure rate to respond was about 30%.[7]
Most of the large trials included patients with wide QRS irrespective of the QRS morphology.A meta-analysis and a sub-study of the Multicenter Automatic Defibrillator Implantation Trial II(MADIT II) demonstrated that benefits, including the long-term mortality benefit, are most likely to be among patients with left bundle branch block(LBBB) on the surface electrocardiogram (ECG).[8,9]This suggests that the true substrate to CRT response exists mostly among patients with LBBB cardiomyopathy.This review will provide some historical perspective on the use of cardiac imaging in patients with CRT, but mostly it will concentrate on how cardiac imaging can be applied in context to patients with LBBB and uses of dyssynchrony in patients with CRT.
LBBB AND HEART FAILURE
In patients with LBBB, proximal septal activation takes place earlier as the breakthrough point lies distal to it while the activation of the LV free wall is significantly delayed due to the myocardial fiber-tofiber transmission of the electrical impulse rather than the faster Purkinje system.This abnormal activation pattern of the LV is associated with a decreased filling time, increase in mitral regurgitation and a decrease in stroke work.[10]There is also a shunting of myocardial blood flow from the septum, an increase in workload of the LV free wall and a disturbance in circumferential shortening of the LV.[11,12]Over time this ineffective contraction leads to a decrease in LV EF and LV remodeling.[11]
Identification of LBBB on surface ECG, however,can be sometime erroneous and misleading.Studies have demonstrated that nearly one-third of patients are misdiagnosed with LBBB based on surface ECG.[13,14]In fact, these patients have a combination of LV hypertrophy, LV dilatation, and left anterior fascicular block.This is important to consider given the fact that patients are most likely to respond to CRT if they have a true LBBB.A stricter definition of LBBB is proposed by Strauss,et al.,[15]which can be helpful especially if the patient is under consideration for CRT implantation.This criteria proposes the presence of a notching in two contiguous leads (V5, V6, I and aVL) , a wider QRS duration (≥ 130 ms in women and ≥ 140 ms in men)and QS or rS pattern in lead V1.These stricter criteria for the presence of LBBB have shown to increase the sensitivity and specificity to identify potential responder to CRT.[16]
DYSSYNCHRONY AND HEART FAILURE
Regional discoordination in the contraction of LV is termed as dyssynchrony.It is frequently observed among patients with HF.[17]Patients with HF also commonly have electrical dyssynchrony.[18]It was presumed that mechanical contraction heterogeneity between different LV segments is a direct result of the electrical dyssynchrony.However, later it was demonstrated that mechanical dyssynchrony can be observed among patients with HF in the absence of electrical dyssynchrony.[19]Likely, mechanical dyssynchrony is related to LV fibrosis and LV dilatation observed among patients with HF.[20,21]
Now related to CRT, the concept of dyssynchrony becomes important when the following two conditions are met.Firstly, HF is a result of the dyssynchrony and not the opposite.This is where concept of LBBB cardiomyopathy is important to understand.As explained in the previous segment,LBBB patients have certain characteristic electrical and mechanical events which leads to development of HF.Secondly, this dyssynchrony should be amenable by CRT.If the dyssynchrony is the result of extensive LV fibrosis, then it is unlikely to be resolved by the placement of an extra LV lead.Therefore, in the view of the authors, it is important to understand this before applying the concept of any kind of dyssynchrony in the patients with CRT.
CONVENTIONAL DYSSYNCHRONY: A HISTORICAL PERSPECTIVE
Over the years, several methods to assess dyssynchrony has been described by different groups using different modalities of cardiovascular imaging.[22,23]Among the imaging modalities, echocardiography has a clear advantage over others due to higher temporal resolution.Different echocardiographic techniques have been utilized to measure dyssynchrony, including M-mode, spectral Doppler, tissue Doppler imaging (TDI), two-dimensional (2D) and three-dimensional (3D) speckle tracking echocardiography (STE).Although they differed in techniques,the underlying principle was the same.All these techniques utilized the time- to-peak difference between the opposing walls of the LV to measure dyssynchrony.Each technique had a different cutoff to define a significant dyssynchrony.Different conventional methods are shown in Figure 1 and Figure 2.
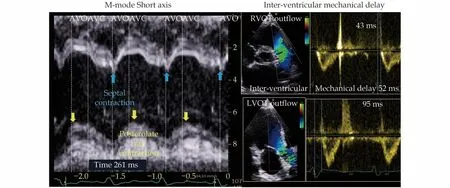
Figure1 The convention methods of dyssynchrony assessment.Left panel shows the dyssynchrony using M-mode on a short axis image.This is patient with left bundle branch block.The early septal contraction and late posterior wall contraction can be easily appreciated.A cut off of 130 ms was used to define significant dyssynchrony by this method.Right panel shows how to determine dyssynchrony by the interventricular mechanical delay.A cutoff of 40 ms was proposed as the significant dyssynchrony by this method.
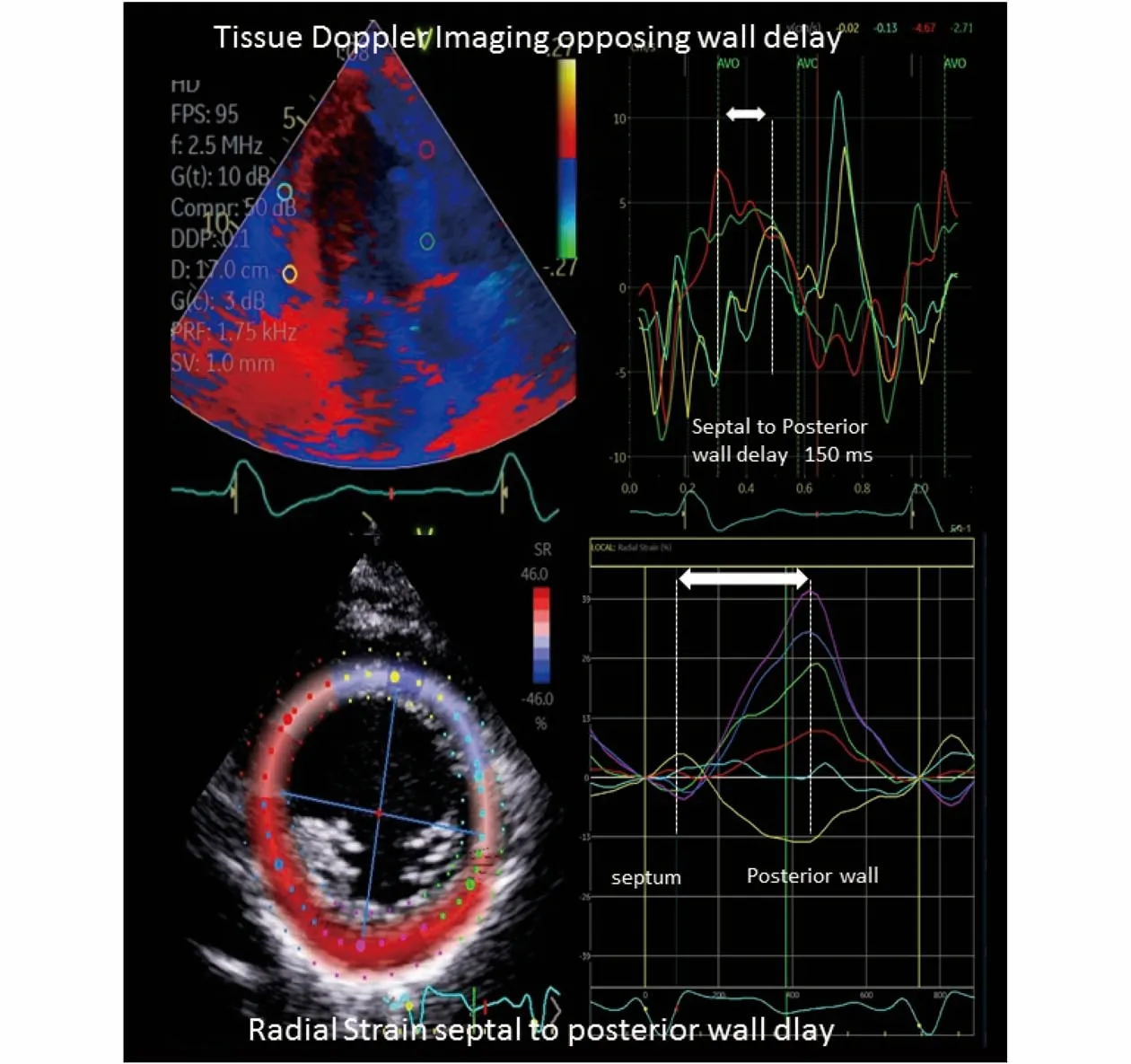
Figure2 Time-to-peak based tissue Doppler imaging and radial strain dyssynchrony methods.Opposing wall delay of > 65 ms was regarded as the presence of significant dyssynchrony by most studies, however, in EchoCRT trial a cutoff of 80 ms was used.25 For the radial strain a uniform cutoff of 130 ms is being applied in the literature.
Two different trials raised a question on the utility of mechanical dyssynchrony in the field of CRT.Predictors of response to CRT (PROSPECT) trial applied 12 different methods available at that time to measure dyssynchrony and none of the methods showed an association with a positive response to CRT.[24]Furthermore, the methods showed a large intra- and inter-observer variability.[24]Echocardiography guided CRT(EchoCRT) trial was the largest randomized trial where patients were recruited solely based on the presence of mechanical dyssynchrony with the absence of electrical dyssynchrony (QRS duration < 130 ms).[25]The methods of dyssynchrony applied to select patients are shown in Figure 2.All patients included has LV EF ≤ 35%,symptomatic HF and were under optimal medical therapy for HF.In this trial, patients (n= 809) were randomized in 1∶1 fashion to CRT-on or CRT-off.The trial was prematurely stopped due to futility.All-cause mortality was significantly higher among the patient with CRT-On.It was observed that young patients had a higher likelihood of dying in the CRT-on arm.EchoCRT trial demonstrated that lone presence of dyssynchrony is not enough for the response to CRT.Both these trials used time-topeak based methods.These time-to-peak methods do not tell anything about the pathophysiology of the HF.They just indicate that there are segmental difference in the contractility of the heart which can be multifactorial.It is like the assessment of LVEF,which do not elucidate anything regarding the pathogenesis if found to be low.However, presence of these time-to-peak dyssynchrony do have prognostic impact which will be discussed in the later segments.
NEWER TECHNIQUES: QUALITATIVE DYSSYNCHRONY METHODS
We would like to discuss two qualitative methods of dyssynchrony which are essentially based on the same mechanism but are assessed using different techniques.[26,27]These methods follow the root cause of pathophysiology of LBBB leading to the development of cardiomyopathy.We do not think these methods have any applications in other forms of bundle branch block.The only additional application of these methods is in patients with pacemaker induced cardiomyopathy.Right ventricular(RV) pacing induced cardiomyopathy have the same activation pattern as the patients with LBBB with some minor differences.[28]
TYPICAL LBBB CONTRACTION PATTERN
As described previously that true LBBB causes early activation of the septum and delayed activation of the free wall due to myocardial fiber-to-fiber activation rather than a fast Purkinje system.This ineffective contraction eventually leads to development of a cardiomyopathy.We believe that in the initial phase only early contraction of septal and delayed contraction of the LV free wall is observed.But eventually as time progresses in some of these patients with LBBB, the septal contraction becomes very short lived which can be related to biological factors, hemodynamic conditions, presence of other comorbidities or idiopathic.The septal contraction becomes so short lived and early that it will pull the LV apex towards the right leading to a stretch of the LV free wall.There will be a redistribution of the myocardial workload with increasing load on the LV free wall and reduced workload or negative workload on the septum.[12,29]This inefficient contraction pattern can be demonstrated using 2D STE.Risum, et al.[30]in a series of studies described three specific LV longitudinal characteristics by STE associated with LBBB cardiomyopathy.The presence of these characteristics described as a typical LBBB contraction pattern are found to associated with not only improved reverse remodeling, but also improved survival when treated with CRT.[26,30]Features of a “typical” LBBB pattern include the following: (1) Septal contraction within 70% of the interval between the start of QRS and aortic valve closure, (2) pre stretch of the lateral wall and,(3) late closure of the lateral wall after aortic valve closure.A typical LBB contraction pattern is shown in Figure 3.
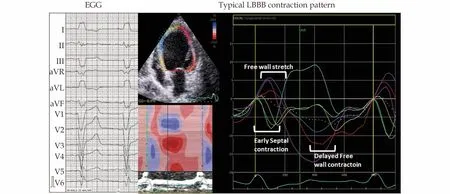
Figure3 This figure on the left panel shows a true LBBB by Strauss, et al.[15] with notching in lead I and aVL and V waves in lead V1 and wide QRS complex.On the right panel longitudinal strain on a 4-chamber image shows the typical contraction patter with all the three features.
In a prospective 4-year follow up study of 208 LBBB patients, the absence of a typical LBBB contraction pattern was associated with a 3-fold increase in mortality with CRT implantation independent of QRS width.More importantly, the presence of this typical contraction pattern was found to be additive in selecting patients with relatively narrower QRS duration ( QRS of 120-149 ms).The advantages of this method is that it a qualitative method rather than measuring the absolute differences in time, which can have a huge variability.Moreover,this method demonstrates the underlying pathophysiology of HF rather than a bystandermlike the time-to-peak methods.
Apical Rocking and Septal Flash
Apical rocking and septal flash are based on the same principle discussed above.Septal flash is the early contraction of the septum.Apical rocking is a phenomenon which occurs due to typical contraction pattern described above in patients with LBBB.Early septal contraction pulls the apex to the right towards the septum and delayed contraction of the LV free wall with no septal contraction pulls the apex towards the left.This transverse motion of apex during systole in both directions is described by Stankovic et al as apical rocking.[27]Both these phenomena highlight the typical contraction pattern described in patients with LBBB.The only difference is that it is based on eyeballing rather than objectivity like the ‘typical’ contraction pattern described by Risum,et al., which can make it difficult to notice for an in experienced reader.The usefulness of apical rocking and sepal flash was studied by Stankovic et al in a study with 1 060 patients.The correction of both these phenomenon at follow-up were associated with a higher likelihood of reverse LV remodeling.Moreover, the presence these markers were associated with nearly 60% reduction in mortality at a median follow-up duration of 46 months.These markers were found to be additive to biological factors and QRS duration.
LV Lead Position
LV lead position plays a vital role in the outcome after CRT.[31,32]However, the position of LV transvenous lead depends on anatomy and access to cardiac veins.Avoiding placement of LV lead in the region of LV scar has shown to improve response after CRT.[33]In addition to avoiding scar, assessment of dyssynchrony can be utilized in guiding the optimal site for lead placement.Basically, using dyssynchrony analyses, the site of latest activation segment of LV can be identified, and lead placement can be targeted at to that site.Two separate randomized trials have shown the utility of dyssynchrony analysis in identifying the optimal LV lead placement site.[34,35]Both TARGET and STARTER trials used 2D STE (radial strain) to identify the site of latest activation.In TARET 220 patients were enrolled and patients were randomized to 1:1 fashion based on the use of echocardiography LV lead placement.[34]In comparison to standard LV lead placement, 15% more patients responded to echo guided lead placement and lower number of patients had HF hospitalization or suffered death (P=0.03).[34]Based on the position of LV lead to optimal site by imaging, patients were classified as concordant (same segment), adjacent (within 1 segment)and remote (≥ 2 segments).Patients with echo guided concordant lead placement had 4-fold increase odds of response than others.[34]Identical results were obtained in the STARTER trial.[35]STARTER trial further added that the procedural time was not significantly different between the echo guided and standard method (134vs.130 min).Furthermore, a sub-study later showed that the benefit was particularly observed among patients with intermediate QRS duration (120-149 ms) and non-LBBB QRS morphology.[36]
These two studies indicate that concept of dyssynchrony can be further extended in lead placement can be clinically useful tool without any additional procedural time.In future, some fusion of strain mapping by imaging and fluoroscopic images during procedure can make this more useful.The only issue is the echocardiographic technique applied in determination of optimal site of activation delay.It is not always clinically feasible to obtain good short axis images to perform radial strain.Moreover, inter-observer variability can be very high when performed by someone inexperienced in performing radial strain, further limiting its clinical use.
Dyssynchrony after CRT Implantation
As discussed previously dyssynchrony in HF can be multifactorial and not necessarily be related to pathogenesis of HF.Time-to-peak based dyssynchrony methods do not infer anything about the underlying pathology of HF just like LVEF.They are more of a prognostic marker.Presence of mechanical dyssynchrony by time-to-peak methods are found to be related to poor prognosis in patients with both ischemic and non-ischemic cardiomyopathy.[37,38]In experimental studies it is demonstrated that dyssynchrony can induce certain molecular changes which increase susceptibility to fatal ventricular arrythmias (VA).[39,40]Several studies have demonstrated that persistence or worsening of dyssynchrony after CRT in patients with HF is associated with increased risk of VA and mortality.[41-44]
Any persistence, worsening or onset new dyssynchrony after CRT can indicate two possibilities: I)worsening of HF, and II) LV lead induced dyssynchrony.If there is no worsening in HF then the second possibility should be considered.If the latter is suspected, then either changing the lead position or turning the CRT off should be considered.However, no observational or randomized studies have investigated it thus far.Only future studies, if any, designed to investigate this will provide more answers.The role of imaging in CRT is summarized in Figure 4.

Figure4 A schematic diagram showing the current application of the knowledge of dyssynchrony in our view.Out of all the methods described, we believe typical LBBB contraction pattern using longitudinal strain and assessing for septal flash and apical rocking by eyeballing has the most compelling evidence for clinical application.Imaging can be further helpful in LV lead placement by assessing the latest segment of activation and absence of scar.Post CRT implantation, if dyssynchrony can play a role in assessment for prognosis.Persistent or worsening of dyssynchrony may indicate poor prognosis and increased risk of fatal arrythmias.CRT: cardiac resynchronization therapy; LBBB: left bundle branch block LV: left ventricular.
CONCLUSION
Dyssynchrony is a marker of poor prognosis.The conventional time-to-peak based methods have limited use in selection of patients for CRT.However,they can be utilized to identify the latest site of activation for lead placement and as prognostic marker post device therapy.Limited dyssynchrony methods have utility in selection of patients for CRT.Data from randomized studies are needed for their validity.Newer and more advanced computer simulations-based methods are being tested, but further refinement and sophistication is needed for them to be clinically applicable.[45,46]
杂志排行
Journal of Geriatric Cardiology的其它文章
- Atrial fibrillation in older adults with cancer
- Vectorcardiographic QRS area as a predictor of response to cardiac resynchronization therapy
- Electrocardiographic markers of cardiac resynchronization therapy response: delayed time to intrinsicoid deflection onset in lateral leads
- Novel electrocardiographic dyssynchrony criteria that may improve patient selection for cardiac resynchronization therapy
- Alcohol consumption in relation to the incidence of atrial fibrillation in an elderly Chinese population
- Assessment of causal direction between thyroid function and cardiometabolic health: a Mendelian randomization study
