A case of posterior scIeritis with transient myopia and increased intraocuIar pressure
2022-02-23
We write to present a case of posterior scleritis associated with transient myopia,increased intraocular pressure and chorioretinal detachment.This study was performed in accordance with the Declaration of Helsinki.An informed written consent for publication of the clinical and laboratory data was obtained from the patient.Posterior scleritis is a rare disease with unclear etiology.About 20%-40% of the cases may be related to some systemic diseases.When posterior scleritis is diagnosed and treated timely,most of the patients may have a good prognosis.We here present an unusual case of posterior scleritis.
A 29-year-old Han male patient presented with decreased vision of the right eye for one day.He had a history of chronic nephritis for 18y and received routine hemodialysis treatment due to uremia.Both his family and psycho-social histories were normal.His blood pressure fluctuated from 150/85 to 170/100 mm Hg.He had no previous history of refractive error.At the time of initial examinations,his visual acuity (VA)was 20/70 OD,and the best corrected visual acuity (BCVA)was 20/20 OD with -2.50 D.No abnormalities were found in his bilateral anterior segments,while a small amount of superficial retinal hemorrhage as well as cotton wool spots were seen in the fund of his both eyes (Figure 1).Combined with the fluorescent fundus angiography (FFA;Figure 2),he was initially diagnosed with a refractive error of the right eye and bilateral hypertensive retinopathy.Three days after his initial consultation,the right eyesight of the patient continued to deteriorate,and he started to have ocular redness and pain.Upon examinations,the VA of his right eye was 20/250.The anterior chamber of his right eye was found shallow with concurrent increased intraocular pressure of 49 mm Hg.A diagnosis of acute angle-closure glaucoma of the right eye was then considered.After intravenous drip infusion of mannitol (20%,250 mL),the BCVA became 20/200 OD with -4.00/-0.75×50°.The anterior chamber was still shallow with the iris-lens diaphragm moved anteriorly (Figure 3A).The dilated funduscopy showed a temporal retinal detachment with the underlying choroid spherically bulged in the right eye,and no retinal breaks were found (Figure 3B).Therefore,a diagnosis of acute angle-closure glaucoma was less possible.Investigations,including the B-scan ultrasonography,ultrasound biomicroscopy (UBM),optical coherence tomography (OCT;Figure 3C-3E) and FFA (Figure 2),were performed,and the results showed the iris-lens diaphragm moved anteriorly with a ciliary detachment in his right eye.An exudative retinal detachment with the underlying choroidal detachment was also found.The magnetic resonance imaging (MRI) showed a slightly high T1-weighted image(T1WI) signal (Figure 4A) and low T2-weighted image(T2WI) signal (Figure 4B-4D) in the temporal posterior part of the right eyeball.The computed tomography angiography(CTA) exhibited temporal wall thickening of the right eyeball(Figure 4E-4F).Serological tests,including anti-nuclear antibody (ANA) test,rheumatoid factors test,tuberculosis antibody test,human leukocyte antigen (HLA)-B27 test,tests of toxoplasma,rubella virus,cytomegalovirus and herpes simplex virus (TORCH),human immunodeficiency virus(HIV) test,and syphilis antibody test,were found normal.Based on the findings,the patient was diagnosed with posterior scleritis of the right eye and treated with intravenous 10 mg of dexamethasone per day.
各行各业纷纷摆拍出“不小心摔了一跤”的“炫富照”, 这些照片,虽是摆拍,却不失为他们的真实状态。年轻一代敢于表达自我,他们因爱岗而炫,因奉献而“富”!


After one-week treatment of glucocorticoids,the patient's ocular redness and pain were reduced.The BCVA improved to 20/30 OD with -3.25/-0.50×70°.The anterior chamber depth was found normal and the intraocular pressure was 18 mm Hg OD(Figure 3A).The exudative retinal detachment examined by the dilated funduscopy was obviously attenuated.Both the height and area of the choroidal elevation decreased significantly(Figure 3B).The axial length of the right eye was 23.32 mm as measured by the IOL-master to exclude the presence of myopic shift.Recovering of the ciliary detachment,choroid detachment and exudative retinal detachment was found by the B-scan ultrasonography,UBM and OCT (Figure 3C-3E).Since then,the therapeutic regimen has changed to 1 mg/kg of prednisone orally,with the dosage tapered off by 5 mg per week.The patient whose symptoms of ocular redness and pain had disappeared was re-examined after three-week treatment.The BCVA of his right eye improved to 20/20 with -1.50 D.The intraocular pressure was 16 mm Hg OD.The structures of his right eye were found morphologically normal (Figure 3).The FFA also showed a significant improvement in retinal vascular leakage of his right eye (Figure 2).With an additional twoweek treatment,the BCVA became 20/20 OD with -0.25 D,and the axial length of his right eye was 23.34 mm as measured by the IOL-master.

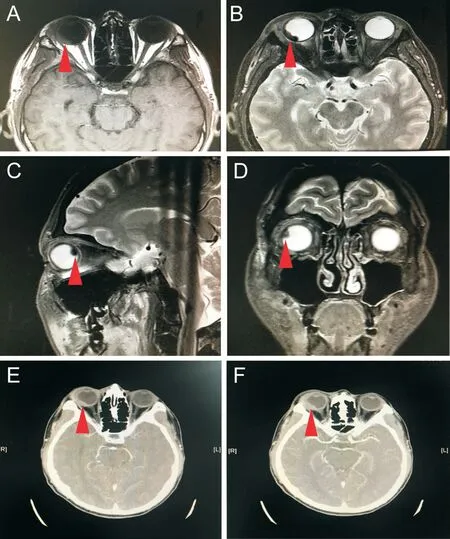
The clinical manifestations of posterior scleritis are complex and variable,lacking specific symptoms and signs.In our case,myopia was the initial manifestation,which was followed by increased intraocular pressure and a shallow anterior chamber.It is rare in posterior scleritis when fundus lesion is not the primary manifestation.Theoretically,posterior wall thickening of the eyeball may result in shortening of the ocular axis,and thus the hyperopia.However,no significant change in the axial length of the patient's right eye was found,despite the presence of posterior wall thickening.The main reason of these changes may be attributable to the uveal effusion and ciliary detachment secondary to posterior scleritis.After relaxation of the suspensory ligaments,the lens became thickened and moved anteriorly,resulting in a myopic shift as well as a shallow anterior chamber and narrow angle.Uveal effusion is an abnormal accumulation of fluid in the suprachoroidal space,resulting in elevation of the choroid.There are various inflammatory and hydrostatic conditions that can cause uveal effusion,but in some cases no obvious cause exists.In this setting,patients are thought to have a distinct,primary abnormality of the choroid or sclera,called uveal effusion syndrome,common in nanophthalmos.A few reports showed that uveal effusion might be the consequence of drug use,such as indapamideand paracetamol,and was manifested as myopia and angle closure.However,uveal effusion secondary to posterior scleritis is not common.A typical “T” sign as detected by the B-scan ultrasonography is more commonly seen in posterior scleritis,suggestive of inflammatory involvement of the posterior eyeball.But this patient shows the ultrasonic manifestations of nodular posterior scleritis,which main manifestations of ultrasonography were nodular thickening of sclera and high internal reflectivity.Because the lesions mainly involve the equator of the eyeball,it is more likely to have a backflow of the vortexes,and thus the formation of uveal effusion.The inflammatory leakage of fluid from the choroid into the suprachoroidal space may lead to ciliochoroidal effusion.Additionally,this rare secondary glaucoma should be distinguished from acute angleclosure glaucoma and malignant glaucoma.This choroidal eminence is also easily confused with fundus tumors,such as choroidal melanoma.In contrast,choroidal tumors were often characterized by an acoustic hollow with low internal reflectivity in the B-scan ultrasonographs and signals of internal blood flow in the color Doppler ultrasound images.Besides findings of the B-scan ultrasonography,the patient showed typical CTA and MRI features of posterior scleritis.Localized thickening of the scleral wall was observed by the CTA,while as lightly high T1WI signal and low T2WI signal of the thickened and elevated wall of the eyeball were found by the MRI.Therefore,imaging investigations are great significance for the diagnosis of posterior scleritis.For the patients with transient myopia,a shallow anterior chamber and increased intraocular pressure,the possibility of uveal effusion and posterior scleritis should be considered.
小学生这个年龄段就是对世界充满了很强地好奇心还有求知欲,并且,孩子们带着活泼好动的天性、注意力难以集中等一些性格特征。所以,在进行小学数学授课的过程当中,假若老师选择先进规范的教学措施,便可以调动起孩子们学习数学的积极性,进一步提升教学质量;相反,课堂授课死板乏味,孩子们便会难以集中注意力听讲。所以,在进行生活化授课过程当中,老师应该主动创设活泼、和谐的数学课堂气氛,指引孩子们保持良好的心态走进课堂学习里面去。
ACKNOWLEDGEMENTS
None;None.
猜你喜欢
杂志排行
International Journal of Ophthalmology的其它文章
- Spaceflight-associated neuro-ocuIar syndrome:a review of potentiaI pathogenesis and intervention
- Certificate for IJO to be indexed in WJCI
- Effect of aberrometry in diagnosis of isoIated spherophakia
- BiIateraI congenitaI uveaI coIoboma concurrent with retinaI detachment
- Spontaneous rupture of ocuIar surface squamous neopIasia-a case report
- Incidence of endophthaImitis after phacoemuIsification cataract surgery:a Meta-anaIysis
