胃癌患者术后预后的独立危险因素及淋巴结转移率对不同pN分期胃癌患者预后的影响
2022-02-15余协媛徐永灿汪伟民
余协媛 徐永灿 汪伟民

[摘要] 目的 分析胃癌患者术后预后的独立危险因素及淋巴结转移率对不同pN分期胃癌患者预后的影响。 方法 随机选取2014年1月至2015年10月在湖州市中心医院进行手术切除治疗的胃癌患者100例作为研究对象。采用电话、门诊等方法进行随访,随访时间超过60个月。比较100例胃癌患者的临床基本资料,采用Log-Rank检验分析100例胃癌患者60个月生存率变化。采用Kaplan-Meier检验分析影响胃癌患者术后预后的单因素。采用Cox比例风险回归模型分析影响胃癌患者术后预后的多因素。采用分层分析淋巴结转移率对不同pN分期胃癌患者预后的影响。 结果 100例胃癌患者中,男性比例明显高于女性,年龄大多超过55岁,肿瘤直径<4 cm,肿瘤部位以胃下多見,pT4分期占比明显高于pT1、pT2、pT3,pN0、pN1、pN2、pN3分期占比分别为32.00%、20.00%、22.00%、26.00%;淋巴结转移率,无转移、≤20%、≥21%占比分别为32.00%、18.00%、50.00%,患者CA19-9、CEA含量分别以低于27 U/ml、5 μg/L多见,血小板计数在(100~300)×109个/L,胃癌大多数为低分化,且患者术后经化疗治疗。100例胃癌患者中,术后12、36、60个月生存率分别为80.00%、60.00%、52.00%。经Kaplan-Meier检验分析,肿瘤直径、肿瘤部位、pT分期、pN分期、淋巴结转移率、CA19-9、CEA、血小板计数、原发术后化疗、分化程度均为影响胃癌预后的危险因素(P<0.05)。经Cox比例风险回归模型分析,肿瘤直径、pT分期、pN分期、淋巴结转移率、CA19-9、CEA等均为影响胃癌患者术后预后的独立危险因素(P<0.05)。经Kaplan-Meier分析,淋巴结转移率对pN1期及pN2期胃癌患者的60个月生存率具有明显影响(P<0.05)。 结论 肿瘤直径、pT分期、pN分期、淋巴结转移率、CA19-9、CEA均为胃癌患者术后预后的独立危险因素,淋巴结转移率对pN1、pN2胃癌患者60个月生存率有显著影响。
[关键词] 胃癌;预后;独立危险因素;淋巴结转移率;pN分期
[中图分类号] R735.2 [文献标识码] A [文章编号] 1673-9701(2022)01-0008-06
The influence of independent risk factors for the prognosis of gastric cancer patients and lymph node metastasis rate on the prognosis of gastric cancer patients with different pN stages
YU Xieyuan1 XU Yongcan1 WANG Weimin2
1.Department of Surgery, Huzhou Central Hospital,Affiliated Central Hospital of Huzhou Normal College, Huzhou 313000, China; 2.Department of Gastrointestinal Surgery, Huzhou Central Hospital, Affiliated Central Hospital of Huzhou Normal College, Huzhou 313000, China
[Abstract] Objective To analyze the effect of independent risk factors for the prognosis of gastric cancer patients and lymph node metastasis rate on the prognosis of gastric cancer patients with different pN stages. Methods A total of 100 cases of gastric cancer patients who underwent surgical resection in Huzhou Central Hospital from January 2014 to October 2015 were randomly selected as the research objects. Follow-up was conducted by telephone and outpatient, and the follow-up time was more than 60 months. The basic clinical data of 100 patients with gastric cancer were compared, and the 60-month survival rate of 100 patients with gastric cancer was analyzed by Log-Rank test. The Kaplan-Meier test was used to analyze the single factors affecting the prognosis of gastric cancer patients after surgery. The Cox proportional hazards regression model was used to analyze the multiple factors affecting the prognosis of gastric cancer patients after surgery. The effect of lymph node metastasis rate on the prognosis of gastric cancer patients with different pN stages was analyzed by stratification analysis. Results Among 100 patients with gastric cancer, the proportion of males was significantly higher than that of females. Most of them were over 55 years old. The tumor diameter was less than 4 cm. The tumor sites were more common under the stomach. The proportion of pT4 staging was significantly higher than that of pT1, pT2, pT3. The proportions of pN0, pN1, pN2 and pN3 stages were 32.00%, 20.00%, 22.00%, and 26.00%, respectively. The proportions of lymph node metastasis without metastasis, ≤20%, and ≥21% were 32.00%, 18.00%, and 50.00%, respectively.It was more common to be lower than 27 U/ml and 5 μg/L in patients with CA19-9 and CEA contents. The platelet count was about (100-300)×109/L. The majority of gastric cancer was poorly differentiated, and the patients were treated with chemotherapy after surgery. Among 100 patients with gastric cancer, the survival rates at 12 months, 36 months, and 60 months after surgery were 80.00%, 60.00%, and 52.00%, respectively.According to Kaplan-Meier test analysis, tumor diameter, tumor location, pT stage, pN stage,lymph node metastasis rate, CA19-9, CEA, platelet count, primary postoperative chemotherapy, and degree of differentiation were all risk factors affecting the prognosis of gastric cancer(P<0.05). According to Cox proportional hazard regression model analysis,tumor diameter, pT staging, pN staging, lymph node metastasis rate, CA19-9, and CEA were all independent risk factors affecting the prognosis of gastric cancer patients after surgery (P<0.05). According to Kaplan-Meier analysis, the lymph node metastasis rate had a significant impact on the 60-month survival rate of pN1 and pN2 gastric cancer patients(P<0.05). Conclusion Tumor diameter, pT stage, pN stage, lymph node metastasis rate, CA19-9, CEA are all independent risk factors for postoperative prognosis of gastric cancer patients. Lymph node metastasis rate has a significant impact on the 60-month survival rate of pN1 and pN2 gastric cancer patients.
[Key words] Gastric cancer; Prognosis; Independent risk factors; Lymph node metastasis rate; pN staging
胃癌是一种消化道恶性肿瘤,是临床上常见的恶性疾病之一,据统计,我国每年胃癌新增病例超90万,而其中死亡患者超过66萬。随着人们生活水平的提高,生活方式的改变,胃癌的发病率正逐年提高,且逐渐趋于年轻化,不仅对患者及其家庭的生活造成巨大影响,更对社会发展造成严重影响[1]。目前,临床上治疗胃癌大多采用手术切除联合术后化疗的综合治疗方法,并取得重大进步,但患者5年生存率仍较低。有研究发现[2-3],肿瘤部位、浸润程度、淋巴结转移之间可相互联系、相互作用,共同影响患者的预后,其中,淋巴结转移是胃癌的主要转移方式,也是影响胃癌患者生存质量的重要因素。有研究证实,在一定范围内,检测出的淋巴结个数越多,患者的生存时间越长,预后越好[4]。此外,患者的淋巴结转移个数与胃癌的pT分期明显相关,对于不同分期的患者,淋巴结转移范围及个数也不尽相同[5]。但关于淋巴结转移个数与pN分期的关系尚不明确。本研究主要对胃癌患者术后预后的独立危险因素及淋巴结转移率对不同pN分期胃癌患者预后的影响进行研究,现报道如下。
1 资料与方法
1.1 一般资料
随机选取2014年1月至2015年10月在湖州市中心医院进行手术切除治疗的胃癌患者100例作为研究对象。纳入标准:①符合胃癌的诊断及治疗[6],且经病理学检查确诊者;②无淋巴结或邻近器官转移者;③参与研究前未经放化疗治疗者;④本组研究经本院医学伦理委员会同意批准,均符合医学伦理学;⑤本人及家属均知情同意并签订知情同意书。排除标准:①病历资料不全或中途退出者;②伴有乙肝等感染性疾病患者;③行单纯性改道手术治疗或姑息性手术者。
1.2 随访
采用电话、门诊等方法进行随访,随访时间为60个月。
1.3 方法
基本信息:根据年龄是否超过55岁分为>55岁55例及≤55岁45例;根据性别分为男77例及女23例。
手术情况:根据肿瘤部位分为胃上18例、胃中27例、胃下53例及全胃2例;根据术后是否化疗分为有化疗76例,无化疗24例。
病理情况:根据肿瘤直径是否超过4 cm分为>4 cm 44例及≤4 cm 56例。根据侵犯程度分为pT1期(肿瘤侵犯黏膜下层)12例、pT2期(肿瘤侵犯固有肌层)17例、pT3期(肿瘤侵犯浆膜下层)8例及pT4期(侵犯指脏层腹膜、邻近组织或结构)]63例。根据淋巴结转移成都分为pN0期(无阳性淋巴结转移)32例、pN1期(淋巴结转移1~2枚)20例、pN2期(淋巴结转移3~6枚)22例、pN3期(淋巴结转移超过7枚)26例。根据淋巴结转移率分为无转移32例、转移率≤21% 18例、转移率≥21% 50例。根据组织学分化程度分为低分化56例、中分化25例、高分化19例。
生化资料:根据糖类抗原19-9(carbohydrate antigen 19-9,CA19-9)表达水平分为>27 U/ml 26例,≤27 U/ml 74例;根据癌胚抗原(carcinoembryonic antigen,CEA)表达水平分为>5 μg/L 28例,≤27 μg/L 72例;根据血小板计数分为>300×109个/L 13例,(100~300)×109个/L 81例,<100×109个/L 6例。
1.4 观察指标
①100例胃癌患者的临床基本资料,随访12、24、60个月时100例胃癌患者的生存率变化,影响胃癌患者术后预后的单因素及多因素分析,淋巴结转移率对不同pN分期胃癌患者预后的影响。②采用Log-Rank检验分析100例胃癌患者60个月生存率变化。③采用Kaplan-Meier检验分析影响胃癌患者术后预后的单因素。④采用Cox比例风险回归模型分析影响胃癌患者术后预后的多因素。
1.5 统计学方法
采用SPSS 19.0统计学软件包进行数据分析。生存率差异比较采用Log-Rank检验分析。单因素分析采用Kaplan-Meier检验分析,多因素分析采用Cox比例风险回归模型分析。淋巴结转移率对不同pN分期胃癌患者预后的影响采用分层分析。P<0.05为差异有统计学意义。
2 结果
2.1 胃癌患者临床资料分析
100例胃癌患者中,男性比例明显高于女性,年龄大多超过55岁,肿瘤直径<4 cm,肿瘤部位以胃下多见,pT4分期占比明显高于pT1、pT2、pT3,pN0、pN1、pN2、pN3分期占比分别为32.00%、20.00%、22.00%、26.00%;淋巴结转移率无转移、≤20%、≥21%占比分别为32.00%、18.00%、50.00%;患者CA19-9、CEA含量分别以低于27 U/ml、5 μg/L多见,血小板计数在(100~300)×109个/L左右,胃癌大多数为低分化,且患者术后经化疗治疗。见表1。
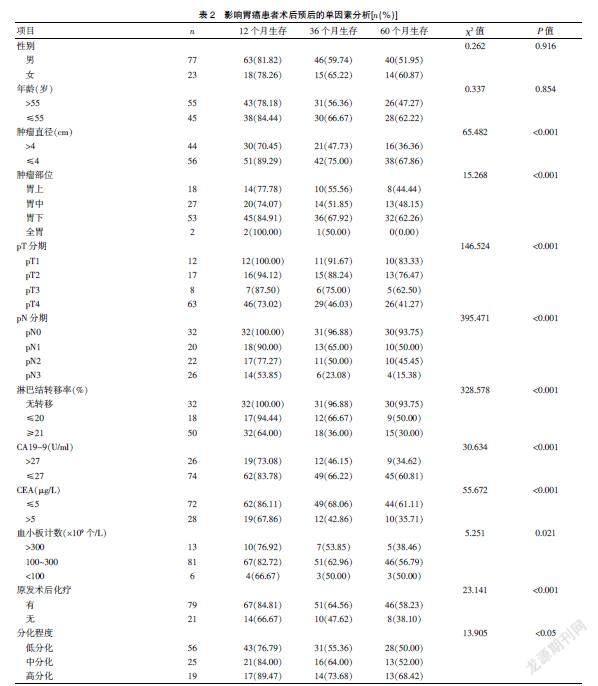
2.2 影响胃癌患者术后预后的单因素分析
100例胃癌患者中,术后12、36、60个月生存率分别为80.00%、60.00%、52.00%。经Kaplan-Meier检验分析,肿瘤直径、肿瘤部位、pT分期、pN分期、淋巴结转移率、CA19-9、CEA、血小板计数、原发术后化疗、分化程度均为影响胃癌预后的危险因素(P<0.05)。见表2。
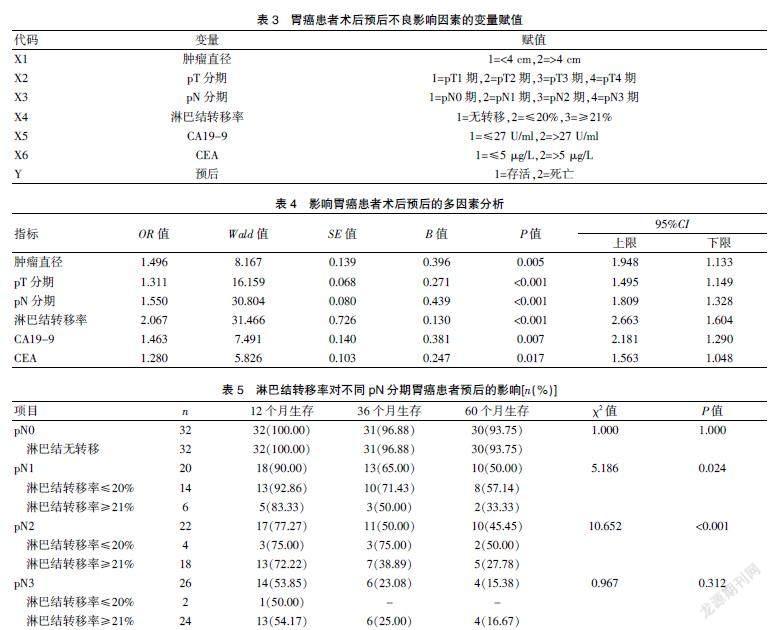
2.3 影响胃癌患者术后预后的多因素分析
经Cox比例风险回归模型分析,肿瘤直径、pT分期、pN分期、淋巴结转移率、CA19-9、CEA等均为影响胃癌患者术后预后的独立危险因素(P<0.05)。见表4。
2.4 淋巴结转移率对不同pN分期胃癌患者预后的影响
经Kaplan-Meier分析,淋巴结转移率对pN1期及pN2期胃癌患者的60个月生存率具有明显影响(P<0.05)。见表5。
3 讨论
胃癌是临床上最常见的恶性肿瘤之一,据统计,在世界范围内,每年胃癌患者的新发病人数超过100万,而死亡人数超过75万,在全球肿瘤相关性死亡疾病中居于第二位[7]。手术治疗是临床上治疗胃癌的主要方法,但术后胃癌复发率较高,而对于胃癌复发尚无特异性有效诊断方法[8]。随着医学科技的发展,医疗设备的完善,临床上诊断及治疗胃癌取得重大进展,但患者的死亡率仍居高不下,且患者预后较差[9]。有研究认为[10],胃癌的发生是一个多因素参与的过程,多种因素参与其中,协同作用。
相关统计,超过50%的癌症患者会并发贫血[11]。血小板是血细胞中最小的细胞,在止血、伤口愈合、炎症反应及器官移植排斥等过程中扮演着重要角色[12]。Cao等[13]研究发现,血小板能阻止肿瘤细胞溶解,屏蔽肿瘤细胞表面和逃逸系统,促进细胞转移,从而对肿瘤细胞起到一定的保护作用。血小板计数是评价血小板数量的有效指标。本研究结果显示,血小板计数是影响胃癌患者术后预后的重要危险因素。
CA19-9、CEA均为相关肿瘤标记物,正常情况下,其表达量极低,而当发生肿瘤时,其表达水平明显升高[14]。Shufang等[15]研究发现,CA19-9、CEA表达水平与患者淋巴结转移及生存率高低明显相关,与本研究结果相似。本研究结果显示,CA19-9、CEA表达水平越高,患者的60个月生存率越低,且其均为影响胃癌患者术后的独立危险因素。
据报道,胃癌患者原发性肿瘤的临床病理特征及术后TNM分期与胃癌术后复发密切相关[16]。但由于各种因素的局限性和差异性,国内外对胃癌根治术后早期复发的独立危险因素的研究结果并不一致[17]。本研究结果发现,肿瘤直径、pT分期、pN分期、淋巴结转移率、分化程度均为影响胃癌预后的危险因素。肿瘤分期系统是为了评估肿瘤疾病的预后、治疗及结果等而开发的分类系统,JGCA与UICC/AJCC临床上常见的评估胃癌患者预后的重要方法,而由于淋巴结转移是胃癌最主要的转移方式[18],因此,胃癌的淋巴结状况被认为是最能影响胃癌患者预后的独立危险因素。有研究发现,淋巴结转移率能够明显减少阶段迁移现象,其对患者的预后具有重要的预测能力[19]。本研究结果表明,肿瘤直径、pT分期、pN分期、淋巴结转移率等均为影响胃癌患者术后预后的独立危险因素。淋巴结转移率不仅是胃癌的独立危险因素,且较pN分期具有更独特的优势,胃癌淋巴结转移的存在和程度直接影响胃癌患者的预后情况[20]。淋巴结转移率对pN1期及pN2期胃癌患者的60个月生存率具有明显影响。
综上所述,肿瘤直径、pT分期、pN分期、淋巴结转移率、CA19-9、CEA均为胃癌患者术后预后的独立危险因素,淋巴结转移率对pN1、pN2胃癌患者60个月生存率有显著影响。
[参考文献]
[1] Logan RP.Helicobacter pylori and gastric cancer[J]. Lancet(London,England),2019,344(8929):1078-1079.
[2] Spolverato G,Pawlik TM.Clinicopathological evaluation of recurrence in early gastric cancer[J].American Journal of Surgery,2019,157(3):202-207.
[3] Bai T,Yokobori T,Altan B,et al.High STMN1 level is associated with chemo-resistance and poor prognosis in gastric cancer patients[J].British Journal of Cancer,2017, 116(9):1177-1185.
[4] Kino H,Nakano M,Kanamori A,et al.Gastric adenocarcinoma of the fundic gland type after endoscopic therapy for metachronous gastric cancer[J]. Internal Medicine,2018,57(6):795-800.
[5] Katsuyuki,Murai,Kohei,et al.Effect of double-layer structure in intramucosal gastric signet-ring cell carcinoma on lymph node metastasis:A retrospective,single-center study[J].Gastric Cancer,2019,22(4):751-758.
[6] 鄭振东,韩涛.胃癌诊疗研究进展[J].临床军医杂志,2017,45(1):1-4.
[7] Zhao R,Zhang Y,Zhang X,et al. Exosomal long noncoding RNA HOTTIP as potential novel diagnostic and prognostic biomarker test for gastric cancer[J]. Molecular Cancer,2018,17(1):68.
[8] Lu Xueying,Li Yanhong,Li Xiaobo,et al. Luteolin induces apoptosis in vitro through suppressing the MAPK and PI3K signaling pathways in gastric cancer[J].Oncology Letters,2017,14(2):1993-2000.
[9] Yiren H,Yingcong Y,Sunwu Y,et al. Long noncoding RNA MALAT1 regulates autophagy associated chemoresistance via miR-23b-3p sequestration in gastric cancer[J]. Molecular Cancer,2017,16(1):174.
[10] Cheng Y,Song Y,Qu J,et al.The chemokine receptor CXCR4 and c-MET cooperatively promote epithelial-mesenchymal transition in gastric cancer cells[J]. Translational Oncology,2018,11(2):487.
[11] Virgilio E,Giarnieri E,Giovagnoli MR,et al.Gastric lavage malignant cells(yGL) and hypohemoglobinemia (yAnemia) as new systems of tumor regression grading and prognostic prediction for gastric cancer after neoadjuvant treatment[J]. Anticancer Research,2019,39(2):1019-1027.
[12] Yun ZY,Li N,Zhang X,et al. Mean platelet volume,platelet distribution width and carcinoembryonic antigen to discriminate gastric cancer from gastric ulcer[J]. Oncotarget,2017,8(37):62 600-62 605.
[13] Cao W,Yao X,Cen D,et al.The prognostic role of platelet-to-lymphocyte ratio on overall survival in gastric cancer:A systematic review and meta-analysis[J]. BMC Gastroenterology,2020,20(1):16.
[14] Shen M,Wang H,Wei K,et al.Five common tumor biomarkers and CEA for diagnosing early gastric cancer:A protocol for a network meta-analysis of diagnostic test accuracy[J].Medicine,2018, 97(19):e0577.
[15] Shufang N,Wene W,Jilin L,et al. Clinical significance and diagnostic capacity of serum TK1,CEA,CA19-9 and CA72-4 levels in gastric and colorectal cancer patients[J].Journal of Cancer,2018,9(3):494-501.
[16] Mahar AL,Jeong Y,Zagorski B,et al.Validating an algorithm to identify metastatic gastric cancer in the absence of routinely collected TNM staging data[J]. BMC Health Services Research,2018,18(1):309.
[17] Acher AW,Squires MH,Fields RC,et al.Readmission following gastric cancer resection:Risk factors and survival[J].Journal of Gastrointestinal Surgery,2016,20(7):1-11.
[18] Ikoma N,Estrella JS,Blum M,et al.Central lymph node metastasis in gastric cancer is predictive of survival after preoperative therapy[J].Journal of Gastrointestinal Surgery,2018, 22(5):1-9.
[19] Wei-Han Z,Xiao-Hai S,Xin-Zu C,et al.Characteristics and survival outcomes related to the infra-pyloric lymph node status of gastric cancer patients[J]. World Journal of Surgical Oncology,2018,16(1):116.
[20] Kim JW,Lee H,Min YW,et al.Oncologic safety of endoscopic resection based on lymph node metastasis in ulcerative early gastric cancer[J]. Journal of Laparoendoscopic & Advanced Surgical Techniques,2019,29(9):1105-1110.
(收稿日期:2021-02-24)
