New-onset depression after hip fracture surgery among older patients:Effects on associated clinical outcomes and what can we do?
2022-01-11HaoChengQinZhiWenLuoHengYiChouYuLianZhu
Hao-Cheng Qin,Zhi-Wen Luo,Heng-Yi Chou,Yu-Lian Zhu
Hao-Cheng Qin,Yu-Lian Zhu,Department of Rehabilitation Medicine,Huashan Hospital,Fudan University,Shanghai 200040,China
Zhi-Wen Luo,Department of Sports Medicine,Huashan Hospital,Fudan University,Shanghai 200040,China
Heng-Yi Chou,Department of Orthopedics,Huashan Hospital,Fudan University,Shanghai 200040,China
Abstract BACKGROUND Hip fracture in the elderly is a worldwide medical problem.New-onset depression after hip fracture has also received attention because of its increasing incidence and negative impact on recovery.AIM To provide a synthesis of the literature addressing two very important questions arising from postoperative hip fracture depression (PHFD) research:the risk factors and associated clinical outcomes of PHFD,and the optimal options for intervention in PHFD.METHODS We searched the PubMed,Web of Science,EMBASE,and PsycINFO databases for English papers published from 2000 to 2021.RESULTS Our results showed that PHFD may result in poor clinical outcomes,such as poor physical function and more medical support.In addition,the risk factors for PHFD were summarized,which made it possible to assess patients preoperatively.Moreover,our work preliminarily suggested that comprehensive care may be the optimal treatment option for PHFDs,while interdisciplinary intervention can also be clinically useful.CONCLUSION We suggest that clinicians should assess risk factors for PHFDs preoperatively,and future research should further validate current treatment methods in more countries and regions and explore more advanced solutions.
Key Words:Depression;Hip fracture;New onset;Risk factors;Treatments;Clinical outcomes
INTRODUCTION
Hip fractures are one of the most common physical injuries in the elderly,and they often occur after a sudden fall in older people with osteoporosis.In addition to osteoporosis,other risk factors include aging,osteoarthritis,malnutrition,muscle weakness,arthritis,and visual impairment[1-3].At least 120 million people around the world are affected by hip fractures.Between 2012 and 2016,the cumulative incidence of hip fractures among those aged 55 years and over in urban China was 148.75 per 100,000.Moreover,the cost of hospitalization for hip fractures increased six-fold from 2012 to 2016,while per person,it increased by 1.59 times[4,5].Given that the global population of the middle-aged and elderly is expanding,hip fractures will be sure to transform into a significant challenge and a critical health issue for all of humanity.The 1 mo mortality rate after hip fracture surgery is approximately 5% to 8%[6],while the cumulative mortality rate at 12 mo is 33%[7].In addition to the high mortality rate,hip fractures threaten patients’ functional status in all aspects[8,9],especially ambulation ability in the elderly[10].Even among those who lived in the community before their hip fracture,11% ended up as bedridden,20% did not regain normal walking ability,fewer than 30% returned to their previous level of activity,and 80%used walking aids for a year after their hip fracture[1,11].
Depressive symptoms are also prevalent among the old[12],and the onset of depression is obviously associated with a sudden injury or illness that can lead to hospitalization.This is also how postoperative hip fracture depression (PHFD) occurs.Wilsonet al[13] also defined this as new-onset depression,a postoperative diagnosed disease following a depression-free preoperative period,which has been well described in certain cohorts.The prevalence of depressive symptoms is up to 50%among hospitalized older adults,and over one-third of the sample in the study by Ciroet al[14] reported high depressive symptoms during hospitalization.The incidence of depression is also high in patients with broken hips[15].Information extracted from multiple studies[16-19] showed that the prevalence of depression after hip fracture ranged from 9% to 47%.In the systematic review and meta-analysis by Heidariet al[20],researchers concluded that the prevalence of depression among older hip fracture patients was 23% (95% confidence interval [CI]:0.18-0.29).Many studies have proven that older adults with depression are associated with emotional suffering,rising health expenditures,higher risk of suicide,and diminishing quality of life (QOL)[21-23].There is a clinical association between hip fracture and depression.Loss of walking ability,poor QOL,pain,and a sense of loss of future life caused by hip fracture are potential risk factors for depression.
This review explores the risk factors related to PHFD,its adverse clinical outcomes,and effective interventions by means of a literature search.It is expected to provide ideas for clinical workers to deal with the disease and provide direction for researchers.
MATERIALS AND METHODS
We referred to previously published literature search methods[24].We used the PubMed,Web Of Science,EMBASE,and PsyclNFO databases to conduct a systematic review of the published literature and searched up until December 31,2020.The search terms were hip fracture,femoral neck fracture or femoral intertrochanteric fracture and depression,and depressive disorder or low mood (search strategy,Figure 1).We researched reference lists of previously published reviews and studies in these reviews to ensure that no papers were missed.There were no restrictions on language or country of publication.After removing the same study from different databases,two reviewers (Qin HC,Luo ZW) assessed the titles and abstracts of initial papers independently and determined the final inclusion eligibility.Then either reviewer identified the full text of all possibly relevant records and included all subtypes of PHFD.Differences were settled by consensus (Figure 2).

Figure 1 The full-text summary diagram.

Figure 2 Flowchart diagram of the electronic search.
RESULTS
How does PHFD develop (pathogenesis of PHFD)?
From the micro point of view regarding the formation of postoperative depression,postoperative peripheral inflammation can lead to an increase in proinflammatory cytokines in the brain in various ways,resulting in cognitive impairment[25].In turn,these inflammatory factors continue to affect structures in the brain such as glia(microglia and astrocytes),the neurotrophic support of neurons,and changes in the cytotoxicity of neurons.
Looking at this from a macro perspective,the changes in all aspects of life brought about by a hip fracture operation have varying degrees of psychological impact.These include the fear of becoming too dependent on caregivers and placing too much burden on family members;fear that the body will not be able to function as before;loss of hope,confidence,or anxiety about future life;feeling lonely and isolated because their daily activities are restricted;and fear of falling again or even death.These psychological changes after surgery all contribute to the formation of depressive symptoms to a certain extent.
Risk of developing depression in hip fracture
In patients with PHFDs,there are many risk factors that contribute to the progression of the disease including age,sex,complications,types of fracture and preoperative status,and emotional-social support.With a thorough understanding of its risk factors,we can efficiently prevent and diagnose the disease in a timely manner.
Age and frailty:Epidemic data show the link between age and hip fractures;the number of hip fractures and the cost of treatment are increasing in China due to the aging of the population.In the study by Chenget al[26],there were statistically significant differences in the incidence of hip fractures among different age groups.Meanwhile,as people grow older,loss of bone and muscle mass increases the risk of falling,leading to fractures[27].Age is also an important factor in the development of depression.Both the prevalence and the incidence of major depression double after the ages of 70-85[28].Combining these two factors,age as a risk factor for both hip fracture and depression,suggests that age is a potential risk factor for the development of PHFD.Williamset al[29] discovered that the odds ratios (ORs) for depression following fractures among younger women (≤ 65 years) were 0.62 (0.35 to 1.11;P=0.12) and 3.33 (1.24 to 8.98;P=0.02) for older women (> 65 years).However,new knowledge is emerging that frailty,an age-related cumulative decline in multiple physiological systems,is a better predictor of mortality and morbidity than chronological age[30].At the same time,many of the items in the assessment of frailty are risk factors for fractures and depression[31].The identification and assessment of frailty may facilitate the identification of vulnerable preoperative patients so that management can be implemented in a timely manner.The association between the frailty index (as a risk factor) and the risk of PHFD is still unknown,and subsequent research is required to prove this association.
Sex:Among several factors that can influence the epidemiology of hip fractures,sex seems to be the most relevant factor.According to epidemiological data on depression in older adults,depression affects twice as many women as men[28].Hip fracture is an important and debilitating condition in older people,especially women.Epidemiological data vary between countries,but it is globally estimated that hip fractures will have an influence on approximately 18% of women and 6% of men[8].An essential reason is that functional outcomes reported between males and females in survivors and functional outcomes between men and women are most often reported as equivalent or favoring men,although men are consistently reported as having more postoperative complications[32].For example,at discharge,men were more independent in locomotion,transfers,and sphincter control[33].It is also possible that the difference is artificial and that sex differences in help-seeking behavior or symptom reporting exist to the extent that women are more likely to admit and complain about their dysphoric feelings than men,who are more likely to deny and instead of act them out[34].However,there is some controversy.For example,although the incidence is higher in women than in men,the severity of postoperative depression in men is often higher than in women,and the ratio of men to women varies by type of depression[35].
Types of hip fracture:Surgical treatment of hip fractures is mainly divided into internal fixation,hemiarthroplasty,and total arthroplasty.Studies have shown that sex and age are associated with different hip fractures[36].Extracapsular-intertrochanteric fractures were found to increase dramatically with age in women.Since sex and age are risk factors for the development of PHFDs,the type of fracture also plays an important role.Moreover,the postoperative status and rehabilitation requirements for all kinds of T fractures vary,thus representing the differences in the recovery of patients’ postoperative activity ability,which has become one of the leading factors for the development of PHFDs.Elderly patients who receive internal fixation surgery for femoral intertrochanteric fracture do not recommend weight bearing of the affected hip joint at an early time of recovery.A considerable number of patients are still in bed or sitting in a chair for a long time within 1 mo after discharge.Therefore,displaced femoral neck fractures,treated with total hip arthroplasty or hemiarthroplasty,provide a better functional outcome than treatment with internal fixation[37].
Preoperative status and comorbidity:The preoperative status determines the maximum degree of recovery from surgery to some extent.In the study by Shyuet al[38],the authors found that those who were female and had lower prefracture activities of daily living performance were more likely to be at higher risk for depression.Poor nutritional status can also induce postoperative pain[39].In addition to poor motor function and nutritional status being risk factors for the development of PHFDs,some articles found that chronic preoperative opioid use,history of smoking,drug or alcohol use disorder,and preoperative smoking were also risk factors[13,40].Patients with underlying conditions are often more vulnerable to another condition.The presence of comorbidities such as preoperative anxiety disorder[13],cardiovascular disease,diabetes,and cognitive dysfunction was associated with the incidence of postoperative depression[41].In Miguel-Diezet al[42],the authors concluded that the incidence of hip fracture is higher in subjects with chronic obstructive pulmonary disease.Liuet al[43] discovered that predisposed patients with fewer comorbidities belong to the progressively lower-risk group rather than the fluctuating higher-risk group,which suggests that more comorbidities increase the risk of long-term depression following hip fracture.Unfortunately,after extensive literature research,no scale can be found to quantify the association between PHFD and preoperative comorbidities.Given that this may provide better risk stratification,this scale should be created in subsequent studies.
Status of prognosis:The quality of prognosis can be divided into acute and long-term outcomes,and both are sure to be risk factors accelerating depression.In the prognosis of the acute phase,pain is an important risk factor for PHFD.Numerous articles[44-46]have examined the mechanisms linking pain and depression,indicating that pain can remodel neural pathways to trigger negative symptoms of depression.Voshaaret al[15] identified postoperative pain and baseline anxiety as the strongest independent risk factors for depression.Bruggemannet al[47] provides tentative evidence that postinjury beliefs and hopelessness influence levels of depression and anxiety in hip fracture patients in the acute phase of their injury.Long-term risk factors such as loss of walking ability and reduced self-care ability can contribute to the progression of depression.Studies have also indicated a significant difference in the incidence of depression between homebound and semi-homebound elderly adults[48].The psychological changes of the patient as they recover are also important[49].Prolonged bedtime,reduced range of activity,and severe effects on the ability to perform daily activities are all susceptible to forming a sense of helplessness.In conclusion,each stage of the patient’s psychological and physical changes after surgery can affect the development of depression.
Psychosocial factors:Patients’ education,which is often overlooked,is linked to depression.In Liuet al[43],researchers distinguished groups of postoperative depressive-symptom trajectories,and found that patients in the progressively lowerrisk group were less likely to be illiterate than those in the fluctuating higher-risk group (P=0.02).Emotional support from family,friends,and society plays an important role in one’s psychological development,especially those who have experienced impaired health-related QOL[50].Low socioeconomic status[51],living in a rural area,being unmarried,and housing circumstances promote depression disorder,although no direct experimental data have demonstrated an association between PHFD and these factors.
PHFD-associated clinical outcomes
Depression alone or hip fracture alone can lead to a decrease in QOL.The purpose of this part is to summarize the serious clinical outcomes of PHFDs.Exploring the impact of PHFDs on patients can help doctors provide more comprehensive treatment strategies.
PHFD has a great impact on physical function.There was a unanimous conclusion that during the first months after a hip fracture,the physical functioning of all the patients was seriously affected.At the same time,depression symptoms were associated with worse patient-reported outcomes[9,52,53].The trial by Kohringet al[54] quantified the effect of depression on physical function recovery;untreated depressed patients demonstrated significantly smaller gains in physical function computerized adaptive test scores than nondepressed patients.The changes in preoperative and postoperative adjusted mean scores ranged from 37.8 to 45.1 in the nondepression group compared to 38.3 to 45.1 in the untreated depression group (P=0.020).These results suggest that the recovery of physical function in patients with postoperative depression is very limited.Moreover,Gialanellaet al[55] found that neuropsychiatric symptoms made the rehabilitation process slower and less efficient in hip fracture patients.The decline in physical function is bound to affect the QOL,in turn affecting the patient’s psychological changes.Therefore,it is necessary to put an end to this vicious cycle.
Affect postoperative physiological and psychological reactions:Some experiments have reported a statistically significant effect of depression on postoperative pain,resulting in aggravation of both conditions[56,57].Aftonet al[58] found that improvements in depression and anxiety symptoms after surgery were associated with enhancements in pain severity and physical dysfunction.In Cristanchoet al[59],researchers found that a group experiencing a persistently high level of depressive symptoms had poorer functional recovery and higher rates of pain in the year following hip fracture.However,there are new experimental data[60] showing that the relationship between pain and the geriatric depression scale (GDS) after hip fracture is not statistically significant.The effect of depression on postoperative pain needs to be further determined.In addition to causing pain,depression triggers complications after surgery.The analysis by Panet al[61] of the relationship between psychiatric disorders and postoperative outcomes in patients undergoing primary total knee arthroplasty showed that patients with psychiatric disorders had higher ORs for most complications.Second fracture,rate of intensive care unit inpatient[62],postoperative infections[63],and chronic medical illness[64] are all linked to depression.In terms of psychological reaction,patients often show poor adherence,cognitive impairment[65],and poor motivation,which directly affect the rehabilitation and medication process.
More medical support is required:Sullivanet al[66] found that depression was significantly correlated with longer hospital longer limits of stability (LOS) while controlling for demographics and injury severity (P=0.023) by looking at 460 subjects.Longer hospital stays[67] mean increased health care costs and a reduced flow of inpatients.Shelleyet al[57] also statistically analyzed the relationship between injuryand hospital-related variables and posttraumatic stress disorder and depression at baseline and 12 mo after orthopedic trauma,showing that depression at baseline and 12 mo was associated with mechanical ventilation and LOS.In addition,the cost of treating a variety of complications mentioned in the previous section associated with postoperative depression accounts for a large part of the cost.Given increasing health care costs and the condition in which hospital beds are scarce,it is necessary to reduce the incidence of postoperative depression as much as possible to alleviate this situation.
Increase the possibility of rehospitalization:Goldet al[68] showed that overall,90-d readmission rates were approximately 8% for total hip arthroplasty (THA) and total knee arthroplasty (TKA),while the readmission for subjects with depression was 21%-24% higher overall.Therefore,depression is related to a markedly higher risk of readmission after THA and TKA.Reduced readmissions can facilitate the rationalization of the allocation of medical resources and exert apparent impacts on cost and quality.Hospital readmission rates are increasingly used as an indicator of health care quality and a potential source of regulatory penalties for hospitals[69].At present,there are few studies on the direct effect of PHFDs on readmission,and further studies are needed.
Hip fracture is a common cause of mortality in older adults[70] and has a 1-year mortality of approximately 25%[71].Older people with depression also have a higher mortality than average[28].Both factors were independent predictors of mortality in elderly individuals.Liuet al[72] listed the risk factors for mortality in elderly patients with hip fractures,and depression was included.Nightingaleet al[73] concluded that depressive symptoms increase the risk of mortality in patients with hip fracture in the following 2 years.By contrast,Hershkovitzet al[74] demonstrated that only dementia and age were independent predictors of mortality in hip fracture patients during the first 2 years after discharge from a post-acute rehabilitation program,while the presence of depression was not.As the most important clinical concern,patient mortality should be given sufficient attention.
Why does PHFD have such clinical outcomes?Patients with depression may feel hopeless,lack motivation,and be apathetic predisposing them to not participate actively in rehabilitation (adverse effects of depression and cognitive impairment on rehabilitation participation and recovery from hip fracture)[75].Therefore,depression may exert its negative effect as a mediatorviadifferential response to rehabilitation as well as other behaviour with a potential negative effect such as decreased activity,decreased social behaviour,and impaired diet.
Duggalet al[16,76-78] performed a series of studies and found that neutrophil bactericidal properties,monocyte and natural killer cell functioning,and T regulatory immune cells were impaired only in hip fracture patients who developed depressive symptoms.The dysregulation of these immune cells lead to a decline in immune system function and easily lead to postoperative infection.
People with depression tend to have higher cortisol levels than normal people.The higher the cortisol levels in older people,the frailer they are and the worse their physical function[79].Low levels of serum anti-glucocorticoid dehydroepiandrosterone (DHEAS) sulfate have been associated with poorer physical function.Phillipset al[18] found that the ratio of cortisol to DHEAS was significantly higher in patients with PHFDs and was also associated with poorer physical function.The effects of depression on physical functioning may also be mediated by regulating these two substances.
DISCUSSION
Interventions for PHFD
To prevent the negative effects of depression on postoperative recovery and allow patients to recover to the preoperative physical condition as much as possible with less time,effort and cost,PHFD intervention is necessary.The interventions,inclusion criteria,exclusion criteria,groups,and main results included in each trial are listed in Figure 3[80-83,43].
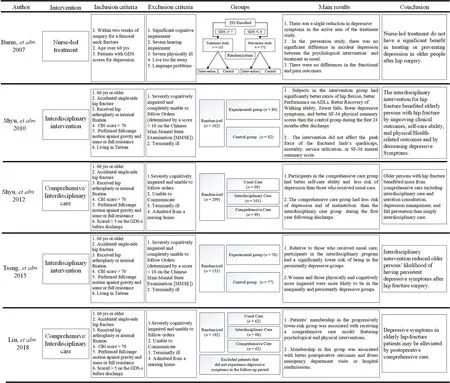
Figure 3 General summary of interventions for postoperative hip fracture depression.
One of the major reasons we focused on postfracture depression rather than preoperative depression is that the treatment of preoperative depression is similar to that of general depression.Depression in patients with PHFDs can be treated by both physical and psychological approaches because improvements in treating physical function can lead to better relief of depression,and early identification and intervention of risk factors for PHFDs is apparently an optimal choice compared with general depression treatments.
Nurse-led treatment and prevention for PHFDs are not significantly effective:Burnset al[80] wanted to determine whether a structured psychiatric intervention (nurse-led)is more effective than treatment as usual (TAU) in reducing depressive symptoms in older people who have depression after hip fracture surgery.Moreover,they explored whether a psychological intervention (cognitive behavior therapy) was more effective than TAU in preventing the development of depression in older people who were free from depressive symptoms immediately after surgery.This was a trial to determine if intervention for depression can treat and prevent its occurrence and progression.In the treatment study,they found a slight reduction in depressive symptoms.In prevention studies,there was no significant difference in the incidence of depression between psychological intervention and conventional treatment.There was also no difference in function or pain outcomes.
In the treatment-of-depression trial,121 participants scored 7 or higher on the GDS and were allocated to nurse intervention (n=61) or treatment as usual (n=60).There were no differences in variables of interest between the two groups at baseline.After six weekly treatments,28 (52%) in the control group remained depressed,compared with 17 (34%) in the intervention group.This univariate comparison was of only marginal statistical significance (P=0.10).GDS scores were simultaneously slightly lower (adjusted 6 wk mean 6.3 [intervention group]vs7.1 [control group],mean difference=0.8;P=0.11].
In a prevention-of-depression trial,172 participants scored 6 or lower on the GDS,and 170 were allocated to the cognitive behaviour therapy (CBT) intervention or treatment as usual (n=85 in each,two participants dropped out before randomization).There were no differences in variables of interest between the two groups at baseline.After the 6 wk follow-up,4 (6%) of the intervention group had depression,compared with 11 (16%) in the treatment-as-usual group (P=0.15).
In conclusion,the findings from the abovementioned trials have some implications for clinical practice.The findings of these two trials indicate that interventions do not have a distinct benefit in treating or preventing depression in older people after hip surgery.Neither therapy had a distinct effect on other variables of interest such as pain,functional recovery,or length of stay.Although the nurse-led intervention is ineffective in either preventing or treating depressive symptoms,this study confirmed the rates of depression after surgery for hip fracture found in previous studies and found that poor clinical outcome was related to factors other than depressed mood.Because they may cause lower human and financial expenditures,the therapeutic methods contained in it also have certain reference significance.
Interdisciplinary intervention decreases depressive symptoms,especially the risk of being persistently depressive:Interdisciplinary treatment involves several professionals who independently treat various issues a patient may have,focusing on the issues in which they specialize.Previous studies[84,85] have shown that interdisciplinary interventions can effectively reduce depressive symptoms after hip fracture surgery in the short term.Shyuet al[81] reported its long-term effects on variables such as self-reported and performance-based outcomes until the 2ndyear after patient discharge.They hypothesized that the clinical benefits of the interdisciplinary intervention would persist into the 2ndyear.
The results showed that depressive symptoms decreased significantly over the first 12 mo after discharge,especially within the 6thmo after discharge,which is consistent with the conclusion of previous experiments.Subjects in the intervention group obviously had fewer depressive symptoms than those in the control group (P=0.05).Over the next 12 mo,although the two groups did not differ significantly in risk for depression at months 12,18,and 24 after discharge,the severity of depressive symptoms at these time points was greater in the control group than in the intervention group.
In most studies of depressive symptoms among older adults with hip fracture,the focus was on the average change in depressive symptoms over time and how individuals deviate from this average.However,there are actually several broad categories of changes in each person’s depression trajectory.Tsenget al[83] wanted to determine the distinct trajectories of depressive symptoms over time and the effects of the interdisciplinary intervention on these distinct courses of changes in depressive symptoms.Tseng performed a secondary analysis using data from previous clinical trials to confirm this hypothesis.
After the classification and correlation analyses of patients with different depression trajectories,it was found that participants in the experimental group were less likely to be persistently depressive over the 2-year period of observation,which means that interdisciplinary intervention reduces the risk of being persistently depressive among older patients with hip fracture.However,the interdisciplinary intervention did not apparently reduce the risk of being marginally depressive.
For interdisciplinary care,although there are multidisciplinary combination therapies,the actual benefits are controversial in some studies.Some experiments[86-88] have shown that compared with conventional geriatric care and rehabilitation,interdisciplinary home rehabilitation for older individuals following hip fracture resulted in similar proportions of complications,readmissions,and total days spent in the hospital after discharge.Interdisciplinary approaches to some aspects of patient recovery after hip surgery remain controversial.
Comprehensive care is the optimal solution at present.In recent years,increasing attention has been given to comprehensive nursing after hip fracture in the elderly[89].At same time,some articles[90-92] have proven that the comprehensive hip fracture program reduced the rate of in-hospital postoperative complications and mortality and improved physical function,role physical,general health,and mental health more than those who received usual care.Improvements in function and a focus on the psyche of the patient with comprehensive treatment can restore the patient’s mental state.
Shyuet al[82] filled a gap in research on the effectiveness of comprehensive therapy directly on depressive symptoms after hip fracture.They designed a study to compare the consequences of the comprehensive care model with those of the author’s previously developed interdisciplinary care model and usual care.They hypothesized that elderly patients who received the comprehensive intervention would have fewer depressive symptoms.After deriving ORs from regression coefficients,they found that the comprehensive care group was 52% less likely to be at risk for depression than the usual care group (OR=0.48,P<0.01).Similarly,the comprehensive care group was 49% less likely than the interdisciplinary care group (OR=0.51,P<0.05) to be at risk for depression.In conclusion,researchers’ comprehensive care programs with depression management appeared to be more beneficial than interdisciplinary care alone for older persons with hip fracture.
After determining that comprehensive care can reduce the probability risk for depression,Liu and Yanget al[43] conducted a secondary analysis of data on a subsample of hip fracture patients at risk for depression.The goal was to examine the associations of membership depressive symptom trajectory groups with receiving the comprehensive care model.Participants belonging to the better postoperative depressive-symptom trajectory group were hypothesized to have received the comprehensive care model.After using a series of analyses to fit trajectory models with two to five trajectory groups,the researchers found that the best fit to the observed data was the model containing two distinct depressive-symptom trajectory groups.To identify the predictors of group membership,they used binary logistic regression modelling and found that patients were likely to be in the progressively lower-risk group if they received comprehensive care than those who received interdisciplinary or usual care(OR=2.78,95% CI:1.00-7.85,P=0.05).Patients in the progressively lower-risk group(approximately 71%) experienced low levels of depressive symptoms that diminished over the 12 mo following surgery.
This analysis is based on a previous experiment,and the conclusion is drawn that comprehensive care featuring both psychological and physical interventions can not only reduce the potential risk for depression but also alleviate depressive symptoms in elderly hip fracture patients.
Both comprehensive intervention and interdisciplinary intervention include a postoperative bedside rehabilitation plan and a postdischarge rehabilitation plan at home.Rehabilitation treatment focuses on the recovery of body function.This is important because depressed patients’ functional recovery is mutually affected.Depression worsens the effectiveness of rehabilitation treatment,and poor consequences in turn continue to increase the psychological pressure of patients.This is sure to be a dilemma for most patients after fracture surgery.Therefore,in the treatment of PHFD patients,it is necessary to pay attention to the physiological and psychological recovery of patients.The treatment we give can only be meaningful if both are improved simultaneously.In addition to the rehabilitation program,only the comprehensive care models feature structured management of depressive symptoms,including patients with GDS-s scores > 10 (n=4).Psychiatric consultation was arranged during hospitalization for diagnosis,suggested psychosocial interventions,and medication management,and a home nurse followed up on patient appointment attendance and adherence to medication regimens.This nurse provided individual consultations,emotional support,and engaged family support for patients with GDS-s scores > 5 (n=28).However,we cannot confirm the effect of depression management because of the difficulties of teasing out the impact of a single care component within a complex intervention program.Early assessment also plays an important role in both intervention models,and geriatric assessment in the early stage can yield information on developing tailored interventions by identifying the type of depression trajectory.For example,those whose GDS scores at discharge are within the 95% CI (6.5-8.5) may need further interventions for interventions for managing depressive symptoms.
The common shortcoming of both models is that the regions we included in the study cannot generalize the global situation,and the effects of the intervention in this study might not be observed if implemented in Western countries or in Japan,limiting the generalizability of the findings to these nations.A comparison of the three treatment strategies is shown in Table 1.
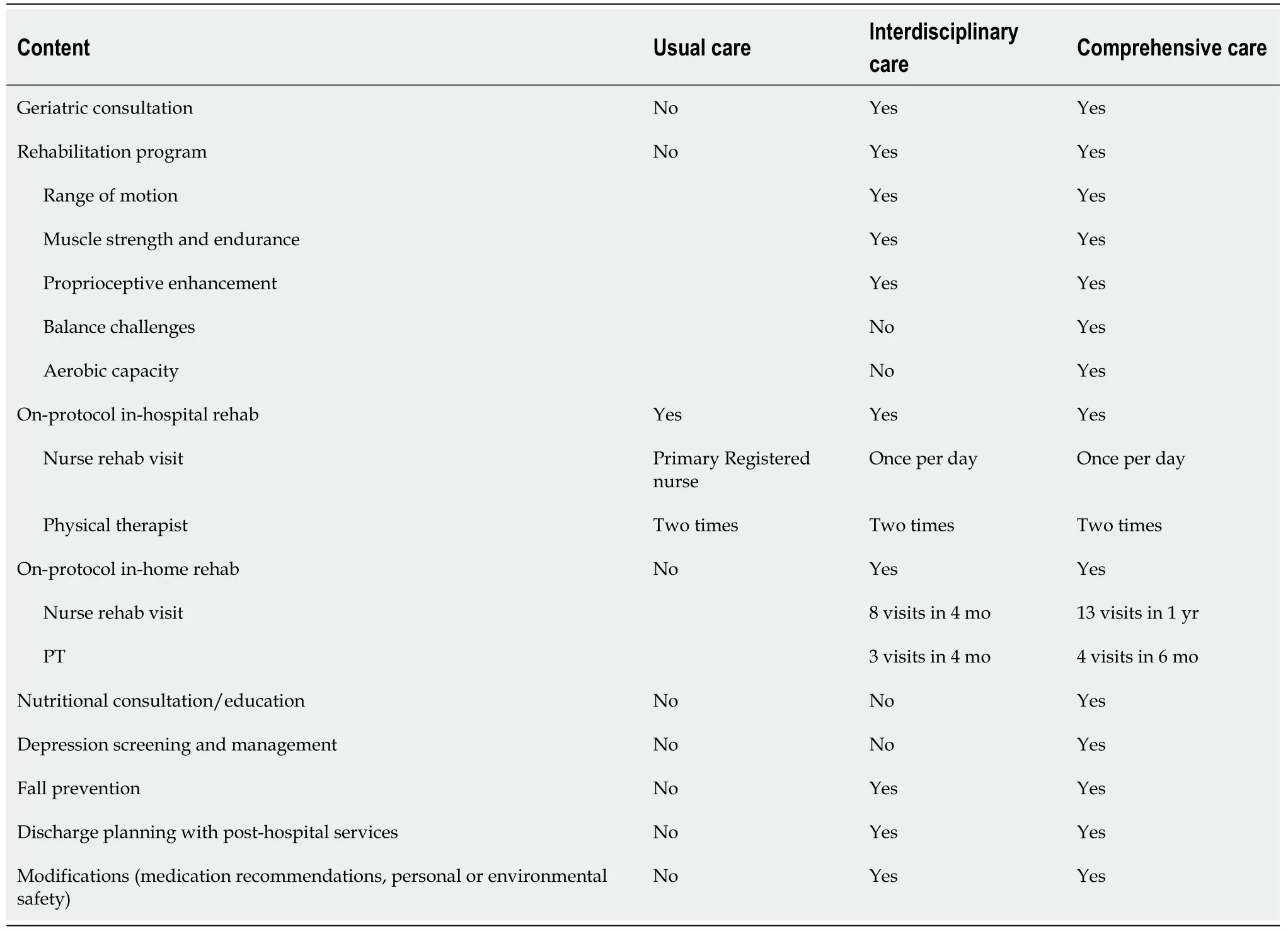
Table 1 Comparison of three care models
Management of medication:In terms of medication management,concerns here are that antidepressants can increase the risk of fractures and reduce physical function.Agarwalet al[93] compared physical function in current female antidepressant users and nonusers and found that the grip strength of nonusers was 13.3% lower than that of current users (P=0.04).Wuet al[94] demonstrated that depression and antidepressant use are independently linked to an increased risk of fracture.Thus,antidepressant treatment might increase the risk of secondary fractures in patients with PHFDs.Specifically,selective serotonin reuptake inhibitor (SSRI) antidepressants have been associated with reduced bone mineral density,and an increased risk of fragility fracture and tricyclic antidepressants may increase the risk of fractureviamechanisms rather than an influence on bone mineral density.However,data on the effects of other antidepressants on bone is insufficient[95].Older patients,who are particularly vulnerable to osteoporosis,may be preferentially prescribed non-SSRI antidepressants.In conclusion,determining whether antidepressant treatment is required and which antidepressant should be prescribed for specific PHFD patients remains unknown.However,at minimum,PHFD patients should be tested for bone mineral density before medication is prescribed.Subsequent studies should compare the risk-benefit ratio for PHFD patients who take antidepressants to those who do not.
Psychological intervention:To date,we have not found an article demonstrating a specific psychotherapy for PHFDs or a controlled trial to verify its effectiveness.However,given the characteristics of patients after hip fracture (i.e.most patients are frail and elderly),some psychological treatment methods for elderly patients with depression can be appropriately adopted.Commonly used and proven psychotherapeutic methods include CBT,behavioral activation therapy,interpersonal psychotherapy,problem-solving therapy (PST),life-review therapy,and nondirective counseling[96].CBT is a widely used technique in the treatment of depression,and its methods are constantly being innovated to apply to different types of depression patients.However,its core is the therapist through therapeutic interactions and topics of discussion,using a psychoeducational approach,and teaching patients new ways of coping with stressful situations to modify the patient’s dysfunctional beliefs (cognitive restructuring) and change their current behaviour as well as future functioning.Huanget al[97] demonstrated the effectiveness of CBT through a three-step process in elderly individuals:behavioral scheduling,cognitive assessment and restructuring,and altering dysfunctional beliefs and performing problem-solving strategies.In PST,patients learn how to systematically solve their problems in a number of steps.Kiosseset al[98] integrated a problem-solving approach (situation selection,situation modification,attentional deployment,cognitive change,and response modulation)with compensatory strategies,environmental adaptations,and caregiver participation to improve emotional regulation in 74 older adults with depression and found that the participants in problem adaptation therapy had a significantly greater reduction in depression.Life-review therapy is mainly used in older adults and is aimed at balancing positive and negative reminiscences,redefining negative experiences,and elaborating memory.The results of Preschlet al[99] indicated that life-review therapy can be recommended for depressive older adults.In the field of psychotherapy for PHFDs,there is still an urgent need for a large amount of experimental data to support the effectiveness of these methods.
CONCLUSION
Our study found that PHFD,if left untreated,has a significant impact on postoperative recovery.Therefore,preoperative identification of risk factors and postoperative intervention on depressive symptoms themselves are important.Given the current research,patients who have PHFDs may benefit from a comprehensive postoperative care model that features both psychological and physical interventions and an interdisciplinary care model.In addition,interdisciplinary approaches may also be a reasonable choice.More high-quality randomized controlled studies are required to validate current models and explore more effective interventions to further intervene in PHFD.
In this review,we introduced PHFDs and summarized their risk factors and clinical outcomes.In addition,we presented a summary of all previous interventions for depression after hip fracture and summarized the methods and experimental results of interdisciplinary treatment,comprehensive treatment,nurse-led treatment,and usual treatment for doctors' reference.Hip fractures are very common in older people and are associated with high rates of disability and mortality.However,depression following joint fracture surgery is also common and places a greater burden on the patient's recovery.Therefore,it is necessary to have a deep understanding of this kind of concomitant disease and to make correct diagnoses and interventions for a better prognosis.
Serious clinical outcomes may occur if PHFD is not dealt with in a timely manner,which emphasizes more importance in the assessment of risk factors to prevent PHFD.If multiple risk factors exist,then patients should be classified as high-risk,and the depression scale should be evaluated after surgery.This is of great significance for the early identification and intervention of PHFD patients.Therefore,the PHFD scale for preoperative risk factors should be reasonably used in patients.Since there is no unified version of the scale at present,future studies can focus on this aspect.
Patients with high-risk factors should receive appropriate intervention before surgery,rather than after the onset of postoperative depressive symptoms,when it may be too late,the cost of treatment increases,and the effectiveness of treatment decreases.Subsequent studies may focus on preoperative intervention on the mechanism of PHFD-induced poor outcomes.
What if,after all that,depression still occurs? At present,it seems that interdisciplinary treatment and comprehensive treatment combined with medication therapy are appropriate choices.(See the hypothesis of clinical diagnosis and treatment of PHFD in Figure 4).
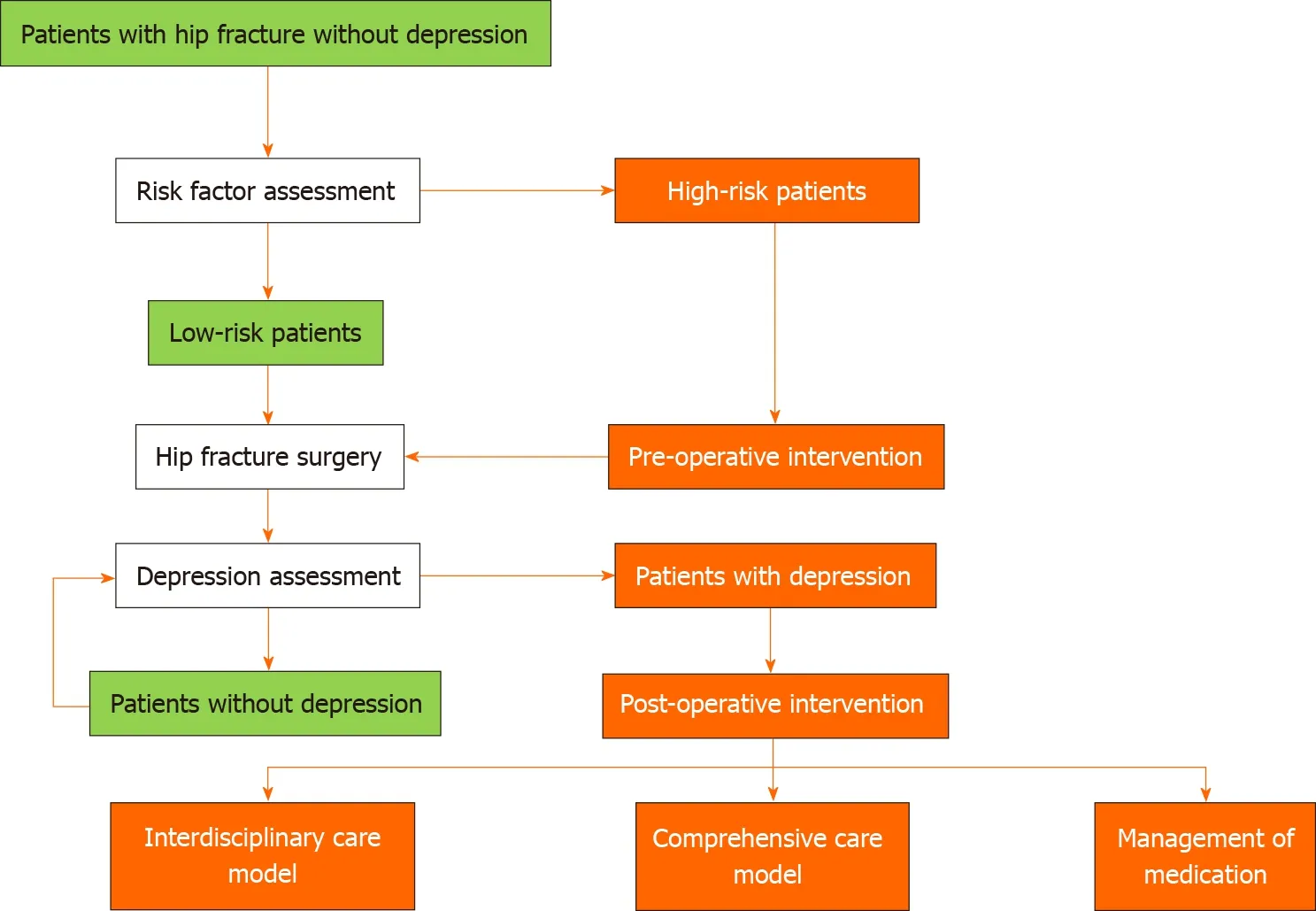
Figure 4 Hypothesis of clinical diagnosis and treatment of postoperative hip fracture depression.
However,future research should explore whether global effectiveness means fitting different countries and regions well.To further verify that the treatment regimen is suitable outside of China,it can be tested in countries with similar national conditions,such as Cambodia and India.At the same time,it can also be tried in smaller developed countries such as Singapore to verify the effect of this treatment on countries with different economic development.In this process,treatment patterns will evolve based on local characteristics and eventually produce a version that works for the entire world.A final point should not be overlooked:we need to expand the scope of the research to explore more effective interventions to further treat PHFDs.
ARTICLE HIGHLIGHTS
Research background
The number of hip patients is on the rise,while the number of postoperative depressions is also increasing.The coexistence of the two diseases makes it more difficult for patients to recover their mental and physical functions after surgery,making this a worldwide medical problem.
Research motivation
Clinically,we observed that depression after hip fracture in the elderly is very common and has caused a great burden on patients’ families and society.Therefore,we wondered if we could find the best intervention to solve the problem.
Research objectives
The aim was to make doctors more aware of the serious consequences of postoperative hip fracture depression (PHFD).In addition,we hoped to provide a basis for the early detection of PHFDs and recommend treatment methods after occurrence of the disease.
Research methods
We searched four databases for articles related to new depression after hip fracture and classified similar articles.
Research results
In this article,we summarize the risk factors for PHFD and the associated adverse outcomes,which can help to raise awareness of the disease and help with its early diagnosis.At the end of this paper,we summarize the practical and effective interventional methods in clinical practice:Interdisciplinary treatment and comprehensive treatment.
Research conclusions
Preoperative identification of risk factors and postoperative intervention on depressive symptoms themselves are important.In addition,PHFDs may benefit from a comprehensive postoperative care model that features both psychological and physical interventions and an interdisciplinary care model.
Research perspectives
Future research should explore global effectiveness in working with different countries and regions.Moreover,the following need should not be overlooked:we need to expand the scope of the research to explore more effective interventions in order to further treat PHFDs.
杂志排行
World Journal of Psychiatry的其它文章
- Effectiveness of cognitive behavioral therapy-based interventions on health outcomes in patients with coronary heart disease:A metaanalysis
- Subgrouping time-dependent prescribing patterns of first-onset major depressive episodes by psychotropics dissection
- Self-compassion and resilience mediate the relationship between childhood exposure to domestic violence and posttraumatic growth/stress disorder during COVID-19 pandemic
- Psychiatric hospitalization during the two SARS-CoV-2 pandemic waves:New warnings for acute psychotic episodes and suicidal behaviors
- CPEB1,a novel risk gene in recent-onset schizophrenia,contributes to mitochondrial complex I defect caused by a defective provirus ERVWE1
- Breast cancer in schizophrenia could be interleukin-33-mediated