儿童感染性腹泻病原微生物、耐药性分析
2021-12-22孟晓飞王爱梅
孟晓飞 王爱梅
(濮阳市疾病预防控制中心微生物检验科,河南 濮阳 457000)
儿童腹泻发病率仅次于呼吸道疾病[1],可引起儿童免疫力降低,水电解质紊乱、发育不良等严重后果,严重危害了儿童的身体健康和生活质量。为了找出感染性腹泻的病原学特征,本文选取本院收治的感染性腹泻儿童100例,探讨儿童感染性腹泻病原微生物、耐药情况。具体内容如下。
1 资料与方法
1.1 一般资料
选取本院2018年12月至2020年12月收治的感染性腹泻儿童100例。纳入标准:所有患儿均符合感染性腹泻的诊断标准[4];本研究内容已被所有患儿家属知晓。排除标准:不配合本研究者。本研究已经过伦理委员会批准。
1.2 观察指标
1.2.1 病原微生物感染种类及其分布情况
从患儿粪便标本提取病毒DNA或RNA后,采用ABi7500型荧光定量PCR仪[迪图(上海)生物科技有限公司]鉴别病毒。按照《感染性腹泻的诊断标准》《全国临床检验操作规程》进行细菌培养[2],将粪便标本接种在麦康凯、木糖赖氨酸去氧胆酸钠、高盐甘露醇琼脂培养基中,在36 ℃条件下培养1 d左右,将可疑菌落接种于克氏双糖铁琼脂中,在36 ℃条件下培养8 h左右,再做血清分型鉴定。
1.2.2 病原微生物耐药性检测
用k-b纸片扩散法进行药敏试验,用金黄色葡萄球菌ATCC25923和大肠埃希菌ATCC25922作为质控菌株;依照临床和实验室标准协会(clinical and laboratory standards institute, CLSI)制定的标准进行结果的判定。
1.3 统计学分析
采用SPSS22.0软件分析两组数据,计数资料表示为n(%),且采用χ2检验;P<0.05表示差异具有统计学意义。
2 结果
2.1 病原微生物感染种类及其分布情况
100例感染性腹泻患儿粪便共培养出97株病原微生物。检出病毒中,占比比较高的依次为诺如病毒Ⅰ型、诺如病毒Ⅱ型和A组轮状病毒;细菌中,致病性大肠埃希菌的构成比最高,其次为沙门菌。见表1。
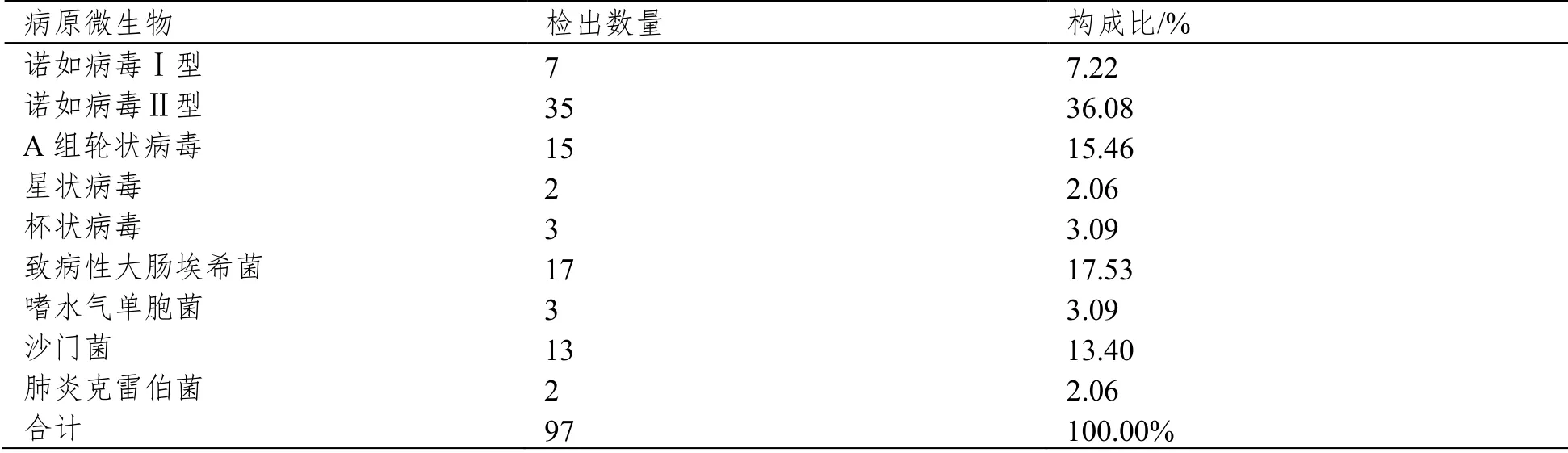
表1 病原微生物感染种类及其分布情况
2.2 耐药性检测
经检测,致病性大肠埃希菌对新生霉素和利福平的耐药性为100%,对四环素和氨苄西林的耐药性为70.11%,对多粘菌素B和阿米卡星的敏感度为100%;沙门菌对新生霉素和利福平的耐药性为100%,对氨苄西林的耐药性为60.23,对阿莫西林和诺氟沙星的敏感度为100%;嗜水气单胞菌、肺炎克雷伯菌等对多数药物敏感度较高,但对新生霉素和利福平的耐药性为100%。
3 讨论
儿童感染性腹泻的主要症状是大便次数异常以及其性状的改变[3],婴幼儿的群体中感染性腹泻的发病率较高,严重危害其健康。本研究结果显示,检出病毒中,构成比较高的有诺如病毒Ⅰ型、诺如病毒Ⅱ型和A组轮状病毒;肠道细菌中,致病性大肠埃希菌和沙门菌的比例较高;与周林等的研究结果相似[4]。
沙门菌作为食源性疾病的常见病原微生物,其传播方式主要是以肉制品、家禽或者蛋白质作为传播媒介,因此应对相关的传播源加强管控。本研究结果显示,大肠埃希菌和沙门菌对新生霉素和利福平的耐药性较高,分析其原因为:临床用药中抗生素的滥用以及菌株质粒的介导造成了致病微生物的变迁[5],从而产生多重耐药等情况,因此,应该加强院内管理,减少多重耐药菌株的风险。在合理使用抗生素的同时,应指导儿童养成良好的生活卫生习惯,以此来减少儿童感染性腹泻的风险。
综上所述,感染性腹泻儿童的主要感染病原为诺如病毒、A组轮状病毒、致病性大肠埃希菌和沙门菌,且致病性细菌具有多重耐药性。
A COVID-19 peptide vaccine for the induction of SARS-CoV-2 T cell immunity
Jonas S Heitmann, et al.
T cell immunity is central for the control of viral infections. CoVac-1 is a peptide-based vaccine candidate, composed of SARS-CoV-2 T cell epitopes derived from various viral proteins1,2, combined with the Toll-like receptor 1/2 agonist XS15 emulsified in Montanide ISA51 VG, aiming to induce profound SARS-CoV-2 T cell immunity to combat COVID-19. We conducted a phase I open-label trial, recruiting 36 participants aged 18 to 80 years, who received one single subcutaneous CoVac-1 vaccination. The primary endpoint was safety analysed until day 56. Immunogenicity in terms of CoVac-1-induced T-cell response was analysed as main secondary endpoint until day 28 and in the follow-up until month 3. No serious adverse events and no grade 4 adverse events were observed. Expected local granuloma formation was observed in all study subjects, while systemic reactogenicity was absent or mild. SARS-CoV-2-specific T cell responses targeting multiple vaccine peptides were induced in all study participants, mediated by multifunctional T-helper 1 CD4+ and CD8+ T cells. CoVac-1-induced interferon-γ T cell responses persisted in the follow-up analyses and surpassed those detected after SARS-CoV-2 infection as well as after vaccination with approved vaccines. Furthermore, vaccine-induced T- cell responses were unaffected by current SARS-CoV-2 variants of concern (VOC). Together, CoVac-1 showed a favourable safety profile and induced broad, potent and VOC-independent T- cell responses, supporting the presently ongoing evaluation in a phase II trial for patients with B cell/antibody deficiency.
Nature. 2021 Nov 23. doi: 10.1038/s41586-021-04232-5.
