Role of orthoptics and scoring system for orbital floor blowout fracture: surgical or conservative treatment
2021-12-17JurajTimkovicJiriStranskyKaterinaJanurovaPetrHandlosJanStembirek
Juraj Timkovic, Jiri Stransky, Katerina Janurova, Petr Handlos, Jan Stembirek,6
1Clinic of Ophthalmology, University Hospital Ostrava, 17.Listopadu 1790/5, Ostrava 708 52, Czech Republic
2Department of Craniofacial Surgery, Faculty of Medicine,Ostrava University, Syllabova 19, Ostrava 703 00, Czech Republic
3Clinic of Oral and Maxillofacial Surgery, University Hospital Ostrava, 17. Listopadu 1790/5, Ostrava 708 52, Czech Republic
4IT4Innovations, VSB-Technical University of Ostrava,Studentská 6231, Ostrava 708 33, Czech Republic
5Department of Forensic Medicine, University Hospital Ostrava, 17. Listopadu 1790/5, Ostrava 708 52, Czech Republic
6Laboratory of Molecular Morphogenesis, Institute of Animal Physiology and Genetics CAS, Veveří 97, Brno 602 00, Czech Republic
Abstract
● KEYWORDS: orbital floor blowout fracture; scoring system; orthoptics; ocular motility; diplopia; conservative treatment; surgical treatment
INTRODUCTION
In patients with orbital floor blowout fractures (OFBF),two principal treatment options are available: conservative and surgical treatment. At present, no guidelines facilitating the decision making which of those treatment options to choose and the decisions depend to a great degree on the general experience and habitual practices of the individual departments[1]. The most common criteria include the size of the defect exceeding one-third of the orbital floor or binocular diplopia resulting from the disruption of ocular motility due to the herniation of soft tissues into the defect[2]. Here, it is,however, necessary to mention that binocular diplopia may not be obvious and in some cases, it can be altogether missing despite the presence of a clear ocular motility disorder (e.g.patients with preexisting concomitant strabismus with an alternating suppression)[3-5]. The diagnosis and treatment of ocular motility disorders are a complex process[6]. As orthoptic examination is the best-suited method for diagnosing ocular motility disorders, the fact that its use in the decision making related to OFBF treatment is largely neglected is actually quite surprising[7-8].
The aims of the presented study were to retrospectively evaluate the results of the conservative and surgical treatment of isolated blowout fractures at our department based on given criteria of therapy success. Providing that the success rate was good, additional aims were to identify possible factors, the presence of which can be associated with the chosen treatment path and based on a detailed analysis of those factors, to propose an easy-to-use pilot scoring system for individualized referring to surgical or conservative treatment.
SUBJECTS AND METHODS
Ethical Approval This study was performed in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the University Hospital Ostrava, Approval No.397/2017.
Patients A retrospective analysis of the documentation of all patients who were treated for isolated blowout orbital fracture and followed up between September 2013 and October 2016 was performed. All patients meeting the following inclusion criteria were included in the study: age at the time of injury 15-80y, isolated one-sided orbital floor fracture confirmed by CT scan, a full orthoptic examination performed per our standard procedure, normal retinal correspondence, normal direct and indirect pupillary light reflex, and known long-term results of the therapy (at least 6-months follow up). Preexisting concomitant strabismus with an alternating suppression was an exclusion criterion.
Treatment Procedures at Our Hospital In each patient,a CT scan with slices below 1 mm was performed, meeting the guidelines and criteria set by the American College of Radiology[9]. The size of the orbital floor defect was measured using defect-delineating and orbital floor delineating tangents in the xVisionViewer software (Vidis, s.r.o, Prague,Czech Republic) and evaluated both in the mediolateral and anterioposterior axes on frontal and sagittal slices of the orbit.The convex shape of the orbital floor was not considered due to the software capabilities. The acquired data were subsequently used for calculating a percentage of the defect in the direction of each axis and of the orbital floor area.
All patients were examined by a maxillofacial surgeon and by an ophthalmologist. The complex examination by an ophthalmologist took place several days after the injury,which allowed time for the initial swelling to partially subside and, therefore, to help us distinguish between ocular motility disorders caused by intraorbital swelling/bleeding from true ocular motility disorders. The examination included the evaluation of refraction, near and far vision, intraocular pressure, biomicroscopic examination of the anterior and posterior segments of both eyes, examination of motility,fixation, accommodation and convergence, of binocular spatial functions using colour filters, Worth four lights and Bagolini striated glasses tests, the degree of strabismus in prism cover test and by synoptophore. The eye position in the anterior-posterior orbital axis was assessed using Hertel exophthalmometer. The ocular motility disorders were objectively assessed and documented by the Lancaster screen test. Based on all those findings, a team consisting of a maxillofacial surgeon and ophthalmologist decided about the treatment methods (conservative/surgical revision with orbital floor reconstruction). The decision whether or not to operate was made strictly individually in each patient, considering multiple factors, among others the defect size and position,enophthalmos on the affected side >2 mm, or ocular motility disorder (with or without binocular diplopia). All the above examinations were repeated during follow-ups.
Where the decision to perform surgery was made, the intervention was performed once the swelling had subsided.We operate through a combination of subciliary and subtarsal approaches in the region of the lower eyelid, accessing the periorbita through the orbitalis oculi muscle. Cutting through the periorbita and exposing the orbital floor defect, herniated tissues are released. The defect is subsequently reconstructed using a resorbable RapidSorb Orbfloor Pl plate (DePuy Synthes, Massachusetts, USA), which is during the surgery shaped to fit the orbital floor and fixed to the edge of the defect with two resorbable stitches. Finally, the plate position and ocular motility are evaluated using the forced duction test and close the wound.
The rehabilitation of ocular motility and, if need be, prismatic correction were managed by an ophthalmologist. The recorded parameters included the need for revision of the original surgery of the orbital floor fracture, the need for surgical correction of an ocular motility disorder and eventual prism correction using glasses.
For evaluating the long-term results of the treatments, the criteria of success/failure of the treatment were set as detailed in Table 1.
Methods of descriptive statistics were used for the initial evaluation of data; namely, the sample mean, sample standard deviation, sample median, minimum and maximum values and the number of patients were used for the continuous variables[relative fracture area (RFA) and lengths in individual axes, age of patients, follow-up period] and sample relative and absolute frequency for categorical variables (all remaining variables used only a binary differentiation between normal/abnormal finding was used for orthoptic variables). Subsequently, the statistical significance of individual factors for their referring to conservative or surgical treatment was assessed using Mann-Whitney test for continuous data and contingency tables withχ2-test for categorical data at the level ofP<0.05. The null hypothesis was H0: the variables in the contingency table are independent. “To achieve a better approximation, Yates correction was used for selected contingency table analyses.Individual variables were subsequently sorted according to the relative risk of being referred to the surgical treatment and strong and weak factors were determined. Correlations between individual variables were determined and uncorrelated variables were subsequently used for creating a pilot scoring system by Logistic regression. Statistical evaluation was performed in the R (R Core Team, 2018) and Microsoft Excel 2010 (Microsoft Corporation, Redmond, Washington, USA).

Table 1 Criteria of the success/failure of the treatment
RESULTS
From September 2013 till October 2016, 69 patients were treated for isolated one-sided orbital floor fracture, 47 of which were male and 22 female. The mean age was 43y(SD=19, median age 42y, min-max 15-80y). Mann-Whitney test revealed no statistically significant difference between the age of patients who were and were not referred to surgery(P=0.94). The median time from the injury to the orthoptic examination was 7d (mean 9d, min-max 1-19d). The median time from the injury to surgery (if performed) was 10d (mean 16d, min-max 5-21d).
Surgical treatment was performed and the orbital floor reconstructed (always after a thorough evaluation of the patient by both the maxillofacial surgeon and the ophthalmologist) in 34 patients (49%) while the remaining 35 patients (51%) were treated conservatively. The mean follow-up period was 26mo in patients after surgical intervention (median 24mo, minmax 12-50mo), and 24mo in patients treated conservatively(median 21mo, min-max 12-51mo). No statistically significant difference in the length of the follow-up period was found between patients treated conservatively and those who underwent surgical treatment (Mann-Whitney test,P=0.453).The mean orbital floor defect size was 279 mm2in patients who underwent surgical intervention (SD=124, median 276 mm2,min-max 77-498 mm2) while in conservatively treated patients,the mean was 177 mm2(SD=98, median 178 mm2, min-max 40-481 mm2). The difference in defect size between both groups was statistically significant (Mann-Whitney,P=0.003).The comparison of the results of the orthoptic examination between the groups can be found in Table 2.
By the end of the follow-up period, we recorded success in 97% of patients who were conservatively treated. Only in one (3%) patient treated conservatively, the final orthoptic examination revealed an ocular motility defect with binocular diplopia; this defect was, however, caused by a partial paralysis of the trochlear nerve, hence the surgical treatment wouldAll parameters derived from Lancaster test describe the injured side only.in all likelihood not have any effect anyway. Where surgical treatment is concerned, we recorded absolute or partial success in 80% of patients. The therapy was without effect in 15% (5 patients) in whom minor ocular motility disorders persisted,namely binocular diplopia in non-primary position,i.e., only in one of the other eight cardinal directions of gaze. In two surgically treated patients (6%), the therapy was unsuccessful(the ocular motility disorder and binocular diplopia persisted even in the primary position). In both these patients, the binocular diplopia that was poorly tolerated by the patient was successfully eliminated by prescription of prism correction in eyeglasses; in one case, an additional surgical procedure addressing strabismus was performed.

Table 2 Results of orthoptic examination, comparison of the presence of individual disorders between the conservatively treated and surgically treated patient groups
Results of the subsequent calculation of relative risks and odds ratios of individual parameters for their referring to the surgical treatment is shown in Table 3. Subsequently, Logistic regression was used to propose a pilot scoring system (Table 4).Models using multiple values of the RFA derived from the CT scans were tested; of those, 25% RFA yielded the best results and hence, this value was used in the developed scoring system. The RFA and limitation of the eyeball elevation detected by the Lancaster screen test were the strongest predictors and assigned the highest values in the scoring system. Additional factors included changes in the ocular motility and position assessed on the Lancaster screen test,presence of any form of binocular diplopia and evaluation of the ocular motility disorder in the vertical direction using the prism cover test.
The threshold values for the scoring system were determined as values associated with an 80% probability of being referred to surgery or conservative treatment in our retrospective study. The use of the scoring system is simple-all factors with assigned values that are present in the patient are to be summedFactors were distinguished in a binary way only (normal/abnormal finding). Where the confidence interval included the value of 1.00,the relationship was considered weak and not taken into account for subsequent modeling.up; if the total is 22 or less, the patient should be treated conservatively while where it exceeds the threshold value of 35 points, the patient is referred for surgical treatment. This is, of course, valid unless a clear contraindication for either decision is present (e.g.,when the patient’s condition prevents surgery). Between those two values, the dependency is almost linear, with a score of 29 denoting a 50% likelihood for being referred for either treatment.
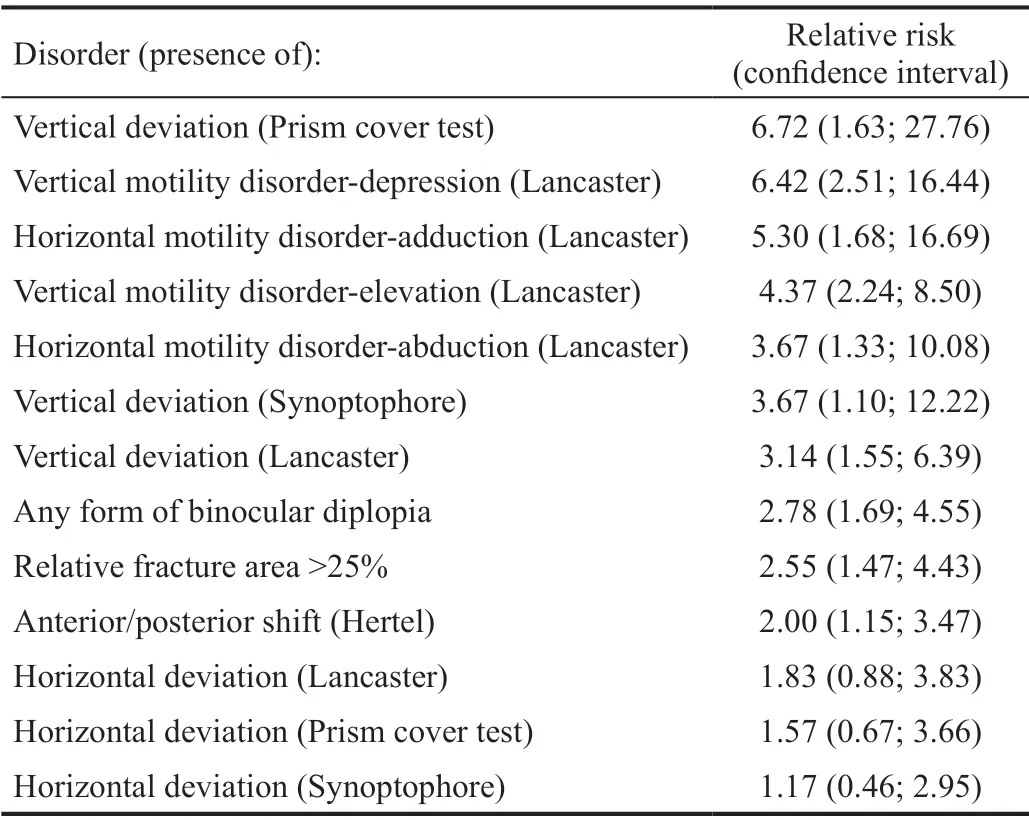
Table 3 Relative risk of referring patients with named factors for surgical treatment
DISCUSSION
Results of Treatment In our patient group, success was recorded in 97% of conservatively treated and 80% of surgically treated patients. All patients with conservative treatment healed well; in the only patient with persistingproblems, those were caused by a reason outside the orbit,namely paralysis of the trochlear nerve. Of seven surgically treated patients in whom the surgical treatment was regarded as ineffective or unsuccessful according to the set criteria, the condition after surgery was better than before it in 4 patients out of 7.

Table 4 A pilot scoring system for decision for surgical or conservative treatment of orbital floor blowout fracture
Our results indicate that none of the patients who were referred for conservative treatment would benefit from surgical treatment and we can thus state that the decision not to operate was correct in all of them. In surgically treated patients, the condition worsened in one patient and failed to improve in two patients. Although the surgical therapy was unsuccessful in these patients, we still believe that the decision to operate was correct as the character of the injuries was so serious (RFA over 30 % of the orbital floor and objectively detected ocular motility disorder) that conservative therapy could in no way yield a better result.
In patients with surgical therapy, the defect size was typically larger than in patients with conservative therapy, which was also associated with a higher risk of complications and represented another reason for a seemingly lower success rate in these patients. Even relatively small defects may in some cases require surgical intervention. As an example, we can mention a patient with the RFA of only 20% of the orbital floor in whom however a decision to operate was made. The main reason for such decision was the localization of the defect in the medial axis of the orbital floor and the consequent definite restriction of movement of the inferior rectus muscle with binocular diplopia. It is, therefore, necessary to emphasize that especially where the decision whether to operate or not is close, it is also necessary to take the site of the defect into account as centrally located defects are associated with herniation of oculomotor muscles much more often than even larger defects localized outside the axial position.
Risk Factors and Scoring System The decision whether or not to operate a patient with an orbital blowout fracture can be a complicated one, especially since subjective complaints of the patient may be changing over time-both in the sense of spontaneous regression of the ocular motility disorder(potentially including binocular diplopia) and recovery of the facial sensitivity and, conversely, in the sense of developing late complications such as ocular motility disorders due to the late change in the volume of orbital soft tissues that can be caused by fading of the swelling or by atrophy of (usually adipose) tissue occurring over a longer period after the injury.It is therefore necessary to evaluate each patient individually and to consider the possible benefits even in patients who show no subjective complaints in the early post-injury period. At present, there is no scoring system that could help clinicians in decision making. According to existing papers,the most common indication criteria for surgical solution are enophthalmos over 2 mm and RFA over 50% of the orbital floor with persisting herniation of soft tissues of the periorbit,binocular diplopia and affected ocular motility resulting from herniation of oculomotor muscles[3,10-16].
Our results confirm that the defect size determined by CT and its accurate measurement is indeed one of the most important criteria in decision making. A detailed analysis of CT scans in both sagittal and frontal slices can provide information both on the size and localization of the defect. Kovářet al[17]performed a retrospective study on 80 patients where they attempted to determine indication criteria for surgical intervention based on the volume of the prolapsed tissue. According to their findings,the threshold for surgical intervention was 500 mm3in anterior and posterior fractures and 1400 mm3in anterior-posterior fractures. Chiason and Matic[18]used the CT-derived ratio of width and length of inferior and medial rectus muscles in their study on 18 patients. In their study, the indication criterion was the length/width ratio of 1.0 for the inferior rectus muscle and 0.7 for the medial rectus muscle.
The change of the eyeball position in the anterior-posterior direction in the sense of enophthalmos, if present, is generally considered to be an indication for surgery[3,11-14,16]. While we observed a statistically significant difference between the presence of a defect in the anterior/posterior shift of the eye by Hertel test, the effect was relatively weak when compared to most of the others and its addition into the scoring system was not shown to have a notable effect on the accuracy.We can also find support for this finding in the literature.For example, Alinasabet al[19]who studied the relationship between herniation of soft tissues and enophthalmos disproved the opinion that herniation of 1 mL of orbital soft tissues into maxillary sinus leads to 1 mm eyeball shift in the anteriorposterior axis. Another study described a conservative treatment in patients with blowout fractures, 22% of whom presented with enophthalmos with more than 2 mm and despite that, all of them resolved without surgical treatment over time[20]. We believe that the main reason is the fact that in the early post-injury period, the presence of enophthalmos is often confounded by changes in the orbital tissues (swelling of orbital soft tissues, bleeding or the presence of pneumoorbit caused by penetration of the air from paranasal sinuses)[19].Besides, enophthalmos is largely a cosmetic problem and as such, it can be resolved through surgery at a later time if the patient is treated conservatively and enophthalmos persists.Therefore, disregarding enophthalmos as an indication criterion in the initial decision making does not pose a significant risk(if any) to the patient[21].
Our experience shows that performing a full orthoptic examination and evaluation of the ocular motility disorder before indicating the patient for conservative or surgical treatment as well as during the rehabilitation is crucial. In the early post-injury period, orthoptic examination allows a more accurate evaluation of motility and position of the eye in the orbit and differentiation between dynamic and restrictive strabismus. From this perspective, the Lancaster screen test is of utmost importance, providing among other data also information about the extent of incomitant, usually restrictive,strabismus. The possibility to evaluate the development of individual parameters over time further underlines the importance of complex orthoptic examination.
The ocular motility disorders represent a frequent, diagnostically very important, symptom of orbital fractures as well as one of their most serious complications. Vertical ocular motility disorders are more common than horizontal in orbital fractures[2]. In our study, the limitations to the vertical ocular motility documented on the Lancaster screen, together with the vertical strabismus deviation detected by cover prism test,represent crucial factors affecting to a great degree the decision whether or not to indicate surgical intervention.
The most typical subjective presentation of ocular motility disorders is binocular diplopia. From this point of view,the relatively low importance of binocular diplopia for the indication for surgery revealed by Logistic regression in our model is surprising. Although the presence of binocular diplopia was an important and statistically significant factor in our study, it was awarded only 4 points in the scoring system,which makes it a parameter of substantially lower importance than the RFA or elevation abnormalities detected on Lancaster screen. The likely reason is that in the early post-injury period,binocular diplopia can be to a major degree masked by the swelling of orbital soft tissues with a drooping upper eyelid.Besides, in the long term, binocular diplopia can be obscured by neuroadaptation and suppression that is highly individual.The presented scoring system aims to provide help in deciding whether or not to operate in patients with orbital blowout fracture. In our experience, the results of orthoptic examinations are more important than the RFA on itself and/or a focus on the presence of binocular diplopia. It is of course necessary to further improve the accuracy and verification of the system and we need to emphasize that we present this system as an adjunctive tool, especially at this stage. The proposed thresholds of ≤22 points for conservative treatment and >35 for surgical treatment correspond to 80% probability to be referred for either treatment in our retrospective study.Our recommendation to refer patients with scores ≤22 points for conservative treatment and those with scores >35 for surgery is, however, obviously not absolute-the scoring system aims to provide guidance but in every single case, an individual approach taking additional factors into account,such as the patient’s age, overall health condition or exact site of the defect, is necessary. This is especially true where patients with a score falling between the proposed threshold values are concerned (i.e., in the range where the relative frequency of the indication to surgery steeply and almost linearly increases). The total score of 29 points was associated with a 50% probability of surgery.
Study Limitations It must be of course emphasised that as this is a retrospective study, it is burdened with autocorrelation.Hence, we present it rather as a basis for further prospective studies and, at this moment, an adjunctive tool; in other words,the proposed scoring system should not be interpreted as the only correct decision-making procedure but rather as a procedure that would lead to results identical to ours (which are, however, very good).
Speaking of results of our treatment, an objection can be made that all patients including those whose therapy was not fully successful were included in modelling. Here, we would like to point out that this scoring system is not used for predicting results of the treatment but only for selecting the treatment method. Not even the best therapy can resolve all defects without any consequences and the injuries of patients in whom we did not record full success were very serious (scores 37 to 56); hence, we believe that their referring to surgery was correct and that their inclusion into the model was, therefore,justified.
An obvious limitation of the study is that although we can be quite sure that none of the patients who were referred for conservative treatment would have benefited from surgery,we cannot be certain that conservative treatment would not be sufficient in some patients who were referred to surgery. In the retrospective view and knowing the results of our scoring system, there were patients with low scores who were referred to surgery. This, however, only underlines the potential value of the presented scoring system in preventing surgery in such patients,i.e., patients who would in all likelihood not benefit from it.
In conclusion, referring patients with orbital blow-out fracture to surgical or conservative treatment is a complex and complicated problem. The decision must be therefore made individually for each patient and consider surgical revision even in patients without subjective complaints in the early post-injury period with relatively smaller orbital floor defects.In our experience, a full orthoptic examination by an experienced ophthalmologist should form an indispensable part of the examination of each patient with orbital blowout fracture, both to provide data necessary for treatment decision,for the rehabilitation of ocular motility disorders and for evaluation of the therapeutic success. The proposed scoring system could become a valuable adjunctive tool for deciding which path to take in the treatment of isolated orbital blowout fractures in everyday practice.
ACKNOWLEDGEMENTS
Foundation:Supported by the Ministry of Health, Czech Republic Conceptual Development of Research Organization(FNOs/2017).
Conflicts of Interest:Timkovic J, None; Stransky J, None;Janurova K, None; Handlos P, None; Stembirek J, None.
杂志排行
International Journal of Ophthalmology的其它文章
- Comparison of trifocal toric and bifocal toric intraocular lens implantation in patients with cataract and high corneal astigmatism
- Comparison of perioperative parameters in one-handed rotational phacoemulsification versus conventional phacoemulsification and femtosecond laser-assisted cataract surgery
- Decreased retinal microvasculature densities in pterygium
- Fourier analysis of corneal Scheimpflug imaging: clinical use in keratoconus
- Establishment of a prediction tool for ocular trauma patients with machine learning algorithm
- Outcomes of half-width vertical rectus transposition augmented with posterior fixation sutures for sixth cranial nerve palsy
