Comparison of trifocal toric and bifocal toric intraocular lens implantation in patients with cataract and high corneal astigmatism
2021-12-17MerveBozkurtGencerHikmetBasmakErdoganYasarOzkanOnal
Merve Bozkurt Gencer, Hikmet Basmak, Erdogan Yasar, Ozkan Onal
1Ophthalmology Clinic, Antalya Training and Research Hospital, Antalya 07100, Turkey
2Ophthalmology Department, Eskisehir Osmangazi University Medicine Faculty, Eskisehir 26040, Turkey
3Ophthalmology Department, Aksaray University Medicine Faculty, Aksaray 68100, Turkey
4Ophthalmology Clinic, Ozalp State Hospital, Van 65800,Turkey
Abstract
● KEYWORDS: cataract; trifocal toric intraocular lens;bifocal toric intraocular lens; stereopsis; satisfaction
INTRODUCTION
Cataract surgery improves vision and refractive defects can also be corrected during surgery. Modern phacoemulsification surgery and recently developed intraocular lenses (IOLs) have increased the visual expectations of patients[1]. Conventional spherical monofocal and bifocal lenses provide a significant increase in visual acuity, visual satisfaction and a reduction in eyeglasses dependence, but not in patients with high corneal astigmatism[2]. Nearly 22%of patients with cataract have ≥1.50 D corneal astigmatism[3].Although some methods such as corneal incision to the vertical axis and limbal relaxation incisions have been used for the correction of astigmatism during cataract surgery, limited and unpredictable improvements are obtained with these methods due to individual differences in the incision site healing process and surgeon factor[4-5]. Toric IOLs are predictable convenient options for the correction of astigmatic refractive defects in patients who don’t prefer to wear glasses after cataract surgery[6-7].
Trifocal toric lenses have a semi-apodization mechanism(regulates optical crusher for distance-intermediate-near)and enhanced focus of depth (EDOF). These lenses also correct ≥1.00 D corneal astigmatism by toric attachment on their optics. Thus, these lenses aim to obtain best and smooth visual acuity without glasses at distance (6 m and far), intermediate (80 cm) and near (40 cm). Bifocal toric lenses are also preferable options due to satisfactory results at distance-intermediate-near[8], the surgical procedure is safer and successful vision is obtained[9]. Trifocal toric IOL is an alternative option in appropriate patients due to a low residual astigmatism value after cataract surgery and satisfactory functional results in distance-intermediate-near, thereby improving quality of life[10-11]. In addition, functional success has been found to be higher in surgeries where rotation of the implanted toric IOL is ≤5°[12]. Glasses dependence after cataract surgery has become almost eliminated with the introduction of trifocal toric lenses[13-14]. These lenses can provide high-performance vision at both near and mid distance without affecting distance vision[15]. Significant improvement in quality of daily life are achieved with this gain in intermediate vision[16].
The aim of this study was to investigate and compare quality of life, satisfaction, contrast sensitivity, glare, depth perception,and IOL rotation levels of patients implanted with Acriva Trifocal toric IOL and Acriva bifocal toric IOL.
SUBJECTS AND METHODS
Ethical Approval The study was conducted according to the principles of the Declaration of Helsinki and approval was obtained from the Ethics Committee of Eskisehir Osmangazi University (No.80558721/122). The Universal Trial Number(UTN): U1111-1264-1020. The informed consent was obtained from the subjects.
The study included 40 patients who were admitted to Eskisehir Osmangazi University Faculty of Medicine Ophthalmology Department between September 2016 and May 2017 with low vision in both eyes and best corrected distance visual acuity (CDVA) of ≤0.5 according to Snellen chart examination. Patients were excluded from the study if they had diabetes mellitus, hypertension, optic neuritis, glaucoma,diabetic retinopathy, age-related macular degeneration,pseudoexfoliation, pterygium, strabismus, corneal nephelion,or a history of ophthalmic surgery. Patients were randomly divided into two groups. A total of 20 eyes of patients with corneal astigmatism of ≥1.00 underwent cataract surgery and the VERION digital microscope-mounted marking system was applied to both eyes with Acriva Reviol tri-ED trifocal toric IOL (Amsterdam, the Netherlands). The other 20 patients underwent cataract surgery and Acriva Reviol bifocal toric IOL (Amsterdam, the Netherlands) was implanted with the conventional corneal marking method. These trifocal toric and bifocal toric IOLs hydrophobic, acrylic and contains 25%water. These IOLs have same optic and haptic diameter, 6 and 11 mm respectively. Both IOLs designs are plate haptic. All ophthalmological examinations of the patients were performed preoperatively and postoperatively by the same examiner. The measurements of IOL rotation and others were performed at operative time and postoperative 1stday, 1stweek, 1st-3rd-6thmonths. Refraction and intraocular pressure (IOP; NIDEK Tonoref II device, 2015, Maehama, Hiroishi, Gamagori, Aichi,Japan) were measured. In both groups, the best uncorrected and corrected distance visual acuities (UDVA and CDVA)were measured at a distance of 6 m with logMAR visual chart. The best uncorrected and corrected intermediate visual acuities (UIVA and CIVA) were determined at a distance of 80 cm with the logMAR near vision chart, and the best uncorrected and corrected near visual acuities (UNVA and CNVA) were measured at a distance of 40 cm. Anterior and posterior segment examinations (tropicamide drops 1%)were performed in all patients. Anterior segment photographs(Topconsl-D7, SN: 1613331, Japan) and macular optical coherence tomography (Zeiss Cirrus HD) images were taken and fundus photographs were recorded with Optos 200Tx. Corneal astigmatism and Kappa angle (Haag-Streit LensstarLS900) were measured and patients with corneal astigmatism of ≥1.00 D and Kappa angle of ≤0.40 were included in the study. Astigmatic axes not evaluated. In both groups, Haag-Streit T-Cone was added to the Lensstar LS 900 for the IOL spherical and cylindrical powers of the patients. To determine the spherical power of IOL, emmetropia was aimed for using SRK-T and Barret formulas. Cylindrical power was calculated using the online module at http://easytoriccalculator.com/acriva.php?lang=en. The NEI-VFQ-25 Visual Function Questionnaire, comprising 25 questions[17], was applied to patients to measure quality of life preoperatively and postoperatively.
In addition to preoperative measurements of the trifocal toric patient group, the Alcon VERION Digital Microscope Mounted Marking System was used to digitally mark the location of corneal incisions during surgery, the size of the capsulorhexis to be opened in the lens capsule and the position of the cylindrical IOL within the eye (within the lens capsule), and a 5.5 mm capsule opening was preferred in this study. The axis was determined according to the keratometric measurements obtained when the cylindrical IOL was placed in the capsule and stabilization was achievedby inserting the IOL into this axis. In the bifocal toric group patients, reference points and IOL position were marked on the astigmatic quadrant of the biomicroscope with a marker pen before surgery. At the 6-month examination, biomicroscopic examination, refraction, IOP, distance-intermediate-near uncorrected and corrected visual acuity were evaluated.Postoperative keratometry was determined after detailed anterior-posterior segment examinations and rotation of the IOL was examined by dilating the pupilla (tropicamide 1%). For the objective measurement of IOL rotation, the method proposed by Wolffshon and Buckhurst[18]in their 2010 study was used. Postoperative photographs were taken using Topcon digital slit lamp (Topconsl-D7, SN: 1613331,Japan) of the lensin situ. All images were photographed at a magnification of ×10 using retro illumination and analyzed.Rotation was determined for each postoperative visit. At the same time, patient satisfaction, the need for glasses and glare symptoms were evaluated by direct questioning of the patients. The Vector Vision CSV-1000E Contrast Sensitivity Test was used for contrast sensitivity and glare measurement.The measurements were performed under normal room illumination conditions after correcting for CDVA. Glare was measured using 2 halogen lamps attached to the CSV-1000E.Glare was tested by switching on the halogen lamps under photopic conditions in the same manner as in the contrast sensitivity test. Near stereopsis (40 and 80 cm) was measured with “TitmusStereotest” and distance stereopsis (2 and 3 m) with the “Distance Randot Stereotest”. The tests were performed using binocular and polarizing glasses and the final arc/s value that the patients could see was recorded.
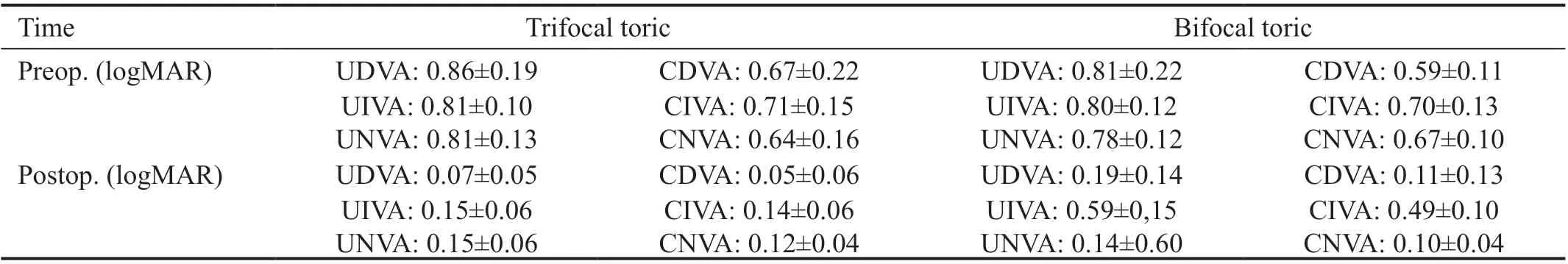
Table 1 Preoperative and postoperative visual acuity results mean±SD
Statistical Analysis Data obtained in the study were analyzed statistically using IBM SPSS for Windows version 21.0 software. Using descriptive statistical analysis, numerical variables were summarized as mean±standard deviation(SD) values. The normal distribution of numerical data was evaluated with the Shapiro Wilk test. The paired samplet-test was used to compare the pre- and postoperative values within groups whereas independent samplest-test was used for between groups comparisons. Statistical significance was assumed atP<0.05.
RESULTS
In this study, the trifocal toric group included 40 eyes of 20 patients, comprising 7 males and 13 females with a mean age of 63.7±11.11y (range 47-81y). The bifocal toric group included 40 eyes of 20 patients, comprising 10 males and 10 females with a mean age of 54.66±11.98y (range 36-74y). No statistically significant difference was observed between the patient groups in terms of age and gender (P=0.077,P=4.422,respectively). The surgeries were performed by the same surgical team with the phacoemulsification technique and no complications occurred. No changes were found between postoperative measurements over the time. Therefore, it was defined 6thmonth. Preoperative and postoperative 6thmonth best uncorrected and corrected distance-intermediate-near visual acuity results are shown in Table 1.
There was no significant difference between preoperative distance-intermediate-near visual acuities in both groups(P=0.102, 0.647, 0.280, respectively). In the postoperative follow-up, mean distance-intermediate-near visual acuity increased significantly compared to the preoperative values(allP<0.001). There was no significant difference between the groups in terms of postoperative distance and near visual acuities (P=0.269,P=0.451, respectively). The postoperative UIVA and CIVA levels were found to be significantly higher in the trifocal toric group compared to the bifocal toric group(P<0.001).
The preoperative and postoperative 6thmonth spherical mean values, cylindrical mean values, and spherical equivalent measurements of the patients are shown in Table 2.
There was no statistically significant difference in postoperative spherical, cylindrical and spherical equivalent measurements(P=0.885, 0.676, 1.000, respectively). In both groups,spherical, cylindrical and spherical equivalent measurements were statistically significantly lower postoperative values compared to preoperative values (P<0.005).
The mean spherical and toric powers of the implanted IOL’s were found be similar. Spherical and toric powers in the trifocal toric group were +21.00 D and +2.50 D respectively.In the bifocal toric group were +21.50 D and +3.00 D respectively.
The mean scores of the visual function scale (NEI-VFQ-25)questionnaire completed by patients preoperatively and at postoperatively 6thmonth are shown in Table 3.
The preoperative and postoperative NEI-VFQ25 questionnaire results of the trifocal toric and bifocal toric groups were found to be statistically similar and there was no significant difference between them (P=0.158, 0.691, respectively). In both groups,the quality of life questionnaire scores were determined to have statistically significantly increased in the postoperative period compared to the preoperative values (P=0.001 andP<0.001).In the trifocal toric group, 2 (10%) patients were prescribed near glasses and 2 (10%) patients were prescribed distance glasses. Near or distance glasses were not needed by 16 (80%)patients. In the bifocal toric group, 2 patients required near glasses (10%) and 2 patients required distance glasses (10%).There was no significant difference between the two groups in terms of wearing glasses (P>0.05) with a low number of patients wearing glasses in both groups.
In respect of general patient satisfaction, 17 patients (85%)were very satisfied with the surgery and postoperative visual performance in the trifocal toric group and the other 3 patients(15%) were satisfied. In the bifocal toric group, 10 patients(50%) were very satisfied with their visual performance and surgical condition, and 10 patients (50%) were satisfied with their visual performance. The overall satisfaction rate in the trifocal toric group was significantly higher than the bifocal toric group (P=0.03).
In the trifocal toric group, 16 patients (80%) had no glare complaints, 3 patients (15%) had mild complaints and 1 patient(5%) had moderate glare complaints. In the bifocal toric group, 10 patients had mild glare (50%), and the remaining 10 patients had no complaints (50%). Glare complaints were significantly lower in the trifocal toric group compared to the bifocal toric group (P=0.03).
Contrast sensitivity and glare were evaluated at 6thmonth. The contrast sensitivity and glare results of the patients are shown in Figures 1 and 2.
The best contrast sensitivity and glare results were obtained at 6 cpd spatial frequency. Although the contrast sensitivity function was not statistically significant (P>0.05) in the trifocal toric group, it was found to be slightly better than in the bifocal toric group.
In both groups, the patients underwent binocular “Titmus Stereotest” at near and medium distance and “Distance Randot Stereotest” at long distance. The stereopsis results of the patients are shown in Table 4.
In both groups, binocular depth perception at 40 and 80 cm,and 2 m distances were found to be statistically significantly higher in the trifocal toric group than in the bifocal toric group(P=0.02, 0.048, 0.003). Although there was no statistically significant difference in stereopsis, the trifocal toric group had higher depth perception (P=0.577) at a distance of 3 m.
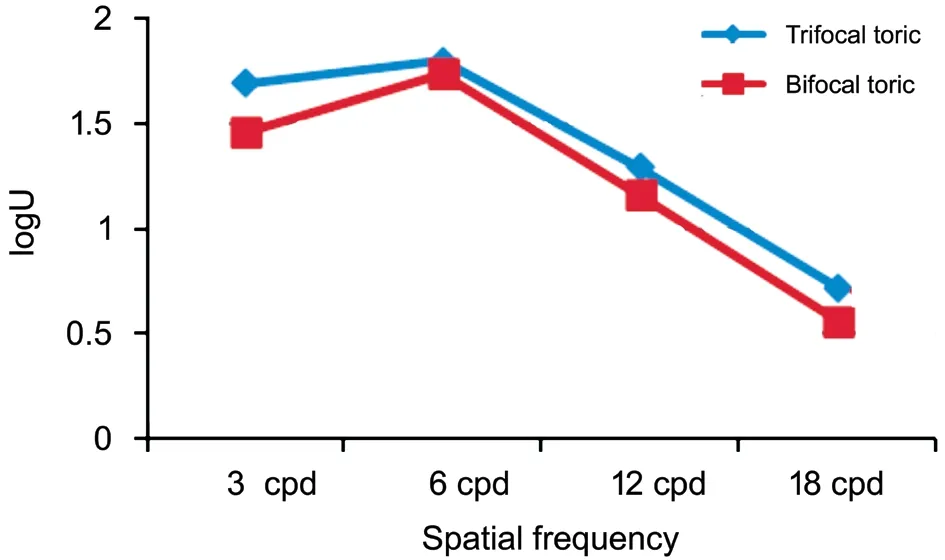
Figure 1 Contrast sensitivity at postoperative 6th month.
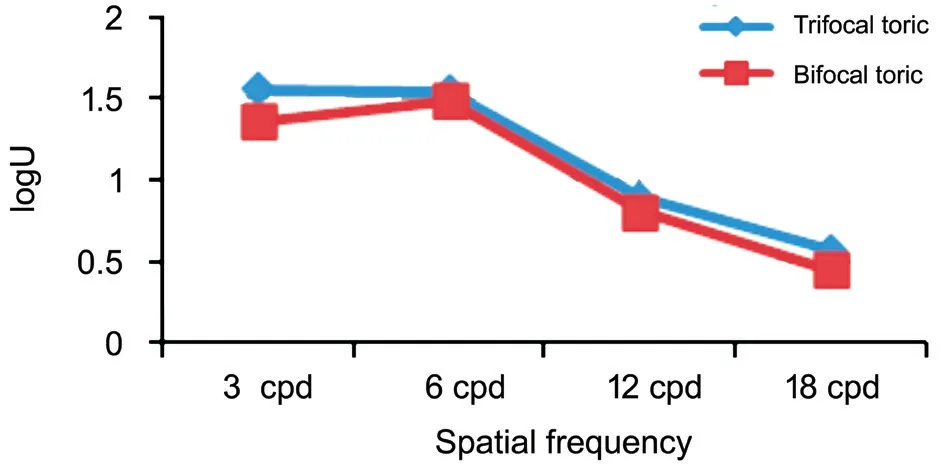
Figure 2 Glare at postoperative 6th month.

Table 2 Preoperative and postoperative refraction measurements mean±SD, D
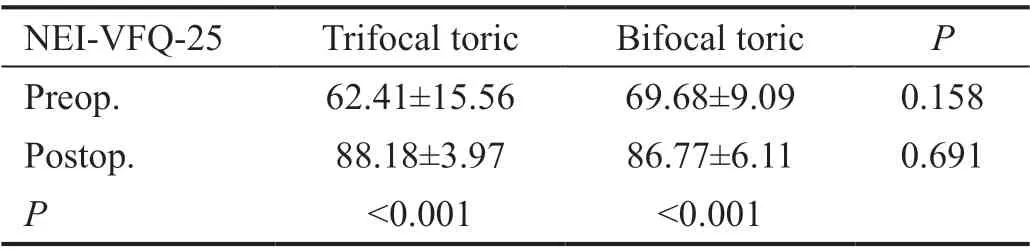
Table 3 Mean visual function scale questionnaire (NEI-VFQ-25) scores
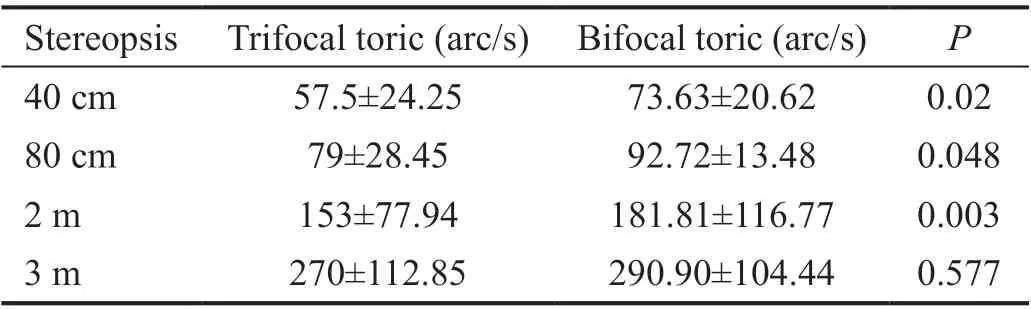
Table 4 Postoperative 6th month stereopsis values
The IOL rotation was evaluated with pupil dilation at postoperative 6thmonth. The mean rotation was 5.76°±3.93°(min: 0° max: 15°) in the trifocal toric group and 12°±7.1°(min: 2° max: 28°) in bifocal toric group. The amount of rotation was observed to be statistically significantly lower in the trifocal toric group (P=0.004).
DISCUSSION
The result of this study showed a statistically significant increase in visual quality of life in both groups (P<0.001),according to the results of the visual function scale (NEIVFQ-25). Toet al[19]reported that NEI-VFQ-25 significantly improved after cataract surgery (P< 0.001) particularly after bilateral eye surgeries. It can be said that the removal of cataracts and IOL implantation generally improve the quality of life of patients. The general satisfaction of the patients was higher in the trifocal toric group than in the bifocal toric group,which may have been due to better intermediate distance visual acuity. It should be acknowledged that both IOLs have different reading additions, and thus the choice of near/intermediate testing distance has been designed to suit the trifocal and as a consequence could disadvantage the bifocal.Petzoldet al[20]reported that after bilateral implantation of bifocal IOLs, 95.9% of patients started that they could accomplish all common tasks without any significant problems.In another study, Rementería-Capeloet al[21]reported that the questionnaire showed high patient satisfaction for those who had undergone trifocal toric IOL implantation.
In the current study, glasses independence was 80% in both groups. Torun Acaret al[22]reported that >90% of patients had no visual impairment in their daily activities. In a study by Voskresenskayaet al[16], 95% of patients did not need near glasses. Kretzet al[9]documented that only 10.5% of patients required postoperative correction for near or intermediate distance. According to these results, it can be said that the need for distance and near glasses in the current study patients decreased significantly at a similar rate to findings in literature.In the trifocal toric group of the current study, there were no glare complaints in 80% and mild glare was determined in 15% of the patients. In the bifocal toric group, 50% of patients had no complaints and 50% had mild glare. In the study by Voskresenskayaet al[16], 16.7% of patients had glare complaints while Kretzet al[9]reported 45.7% halo and 30.4%glare in their patients. The Acriva Reviol Tri-ED trifocal toric IOL semi-apodization technology can significantly reduce the loss of light in the eye, which can cause a significant reduction in glare complaints.
In the current study, the highest contrast sensitivity value was observed at 6 cpd spatial frequency (1.80±0.24 logU and 1.74±0.20, respectively) in trifocal toric and bifocal toric IOL under photopic conditions, and contrast sensitivity values decreased at increasing spatial frequencies. The highest contrast sensitivity levels were also at 6 cpd spatial frequency in studies by Kretzet al[23]and Mojziset al[11]. In contrast to the current study, Voskresenskayaet al[16]reported the highest sensitivity at 3 cpd spatial frequency. The contrast sensitivity curve of the current study patients was found to be highest at 6 cpd spatial frequency, similar to the findings of other studies.
In the current study, the results of the Titmus test, which measures near stereopsis were reported as 57.5±24.25 and 72.63±20.62 arc/s. The distance stereopsis values were found to be 270±112.85 and 290.90±104.44. In a study by Ferrer-Blascoet al[24], 30 patients underwent bilateral bifocal IOL implantation and the near stereopsis Titmus test results were 44.55±1.08 arc/s. Titiyalet al[25]reported that perfect near stereopsis of 20 arc/s was present in 80% of cases, and 82%had good distance stereopsis of 100 arc/s or better. The near and distance stereopsis results in the current study were similar to results in literature.
In the current study, the mean IOL rotation was 5.76°±3.93°(min: 0° max:15°) in the trifocal toric group and 12°±7.1°(min: 2° max: 28°) in the bifocal toric group. In a study by Mojziset al[11], 40% of patients had 0° rotation, 53%had 1°-3° rotation and 7% had 4°-5° rotational deviation.Lubińskiet al[26]performed toric IOL implantation in 26 eyes of 18 patients and reported the mean rotational deviation in the postoperative 6thmonth to be 1.1°±2.4°. In a study of Dubinsky-Pertzovet al[27], 56 eyes of 56 patients were implanted with monofocal toric IOL and in the postoperative 1stmonth IOL rotational deviation was reported 3.18°±3.3° and IOL rotation significantly increased between day 1 to day 7 postoperatively. It is known that, after toric IOL implantation,15° rotation causes loss of half of the desired effect and 30°rotation loses all the desired effect. Rotation of 90° causes the existing astigmatic problem to double. Stabilization of the toric IOL inside the eye postoperatively is closely related to its haptic structure. Bifocal toric IOL was implanted with the conventional corneal marking method and the bifocal IOL group had higher rotation. Although two kind of lenses have same material and designs. Therefore, the Acriva Toric IOL was considered to be very successful due to the plate haptic structure and because the Alcon VERION imaging system used in this study is superior to the classical corneal marking method in IOL placement and axis determination.
In conclusion, trifocal toric or bifocal toric IOL implantation in appropriate patients yields satisfactory and predictable results.Trifocal toric and bifocal toric implantation is considered a satisfactory surgical procedure with the elimination of spectacle dependence, low astigmatism levels and high patient satisfaction. The application of IOL implantation with digital systems rather than manual marking during surgery can be considered to provide more accurate results for IOL stabilization. The main limitation of this study might be the relatively low number of patients. With the evaluation of the 6-month results of trifocal toric and bifocal toric IOL implantation in this study, it was concluded that satisfactory results were obtained especially in intermediate and distance stereopsis,which had a positive effect on the quality of life of the patients.
ACKNOWLEDGEMENTS
Conflicts of Interest:Bozkurt Gencer M, None; Basmak H,None; Yasar E, None; Onal O, None.
杂志排行
International Journal of Ophthalmology的其它文章
- Comparison of perioperative parameters in one-handed rotational phacoemulsification versus conventional phacoemulsification and femtosecond laser-assisted cataract surgery
- Decreased retinal microvasculature densities in pterygium
- Fourier analysis of corneal Scheimpflug imaging: clinical use in keratoconus
- Establishment of a prediction tool for ocular trauma patients with machine learning algorithm
- Role of orthoptics and scoring system for orbital floor blowout fracture: surgical or conservative treatment
- Outcomes of half-width vertical rectus transposition augmented with posterior fixation sutures for sixth cranial nerve palsy
