Risk factors for prolonged intensive care unit stays in patients after cardiac surgery with cardiopulmonary bypass:A retrospective observational study
2021-12-11XueyingZhngWenxiZhngHongyuLouChuqingLuoQinqinDuMengXioyuWuMeifenZhng
Xueying Zhng ,Wenxi Zhng ,Hongyu Lou ,Chuqing Luo ,Qinqin Du ,Y Meng ,Xioyu Wu ,Meifen Zhng ,*
a School of Nursing,Sun Yat-Sen University,Guangzhou,China
b Sun Yat-Sen University Cancer Center,Guangzhou,China
c Digestive Disease Center,The Seventh Affiliated Hospital,Sun Yat-Sen University,Shenzhen,China
Keywords:Cardiac surgery Cardiopulmonary bypass Intensive care units Length of stay Risk factors
ABSTRACT Objectives:Patients after cardiac surgery with cardiopulmonary bypass (CPB) require a stay in the ICU postoperatively.This study aimed to investigate the incidence of prolonged length of stay (LOS) in the ICU after cardiac surgery with CPB and identify associated risk factors.Methods:The current investigation was an observational,retrospective study that included 395 ICU patients who underwent cardiac surgery with CPB at a tertiary hospital in Guangzhou from June 2015 to June 2017.Data were obtained from the hospital database.Binary logistic regression modeling was used to analyze risk factors for prolonged ICU LOS.Results:Of 395 patients,137 (34.7%) had a prolonged ICU LOS (>72.0 h),and the median ICU LOS was 50.9 h.Several variables were found associated with prolonged ICU LOS:duration of CPB,prolonged mechanical ventilation and non-invasive assisted ventilation use,PaO2/FiO2 ratios within 6 h after surgery,type of surgery,red blood cell infusion during surgery,postoperative atrial arrhythmia,postoperative ventricular arrhythmia (all P <0.05).Conclusions:These findings are clinically relevant for identifying patients with an estimated prolonged ICU LOS,enabling clinicians to facilitate earlier intervention to reduce the risk and prevent resulting delayed recovery.
What is known?
· Patients after cardiac surgery with cardiopulmonary bypass(CPB) require a stay in the ICU postoperatively.
· Some patients require a prolonged length of stay (LOS) in the ICU,while prolonged stays are associated with many factors.
· Previous studies,especially in China,have focused on risk factors for prolonged ICU LOS after surgery for one or all heart diseases rather than on patients undergoing CPB.
What is new?
· A high proportion of prolonged LOS in the ICU occurred in patients after cardiac surgery with cardiopulmonary bypass suggests that early evaluation and intervention cannot be ignored.
· This study identifies factors,particularly early postoperative factors (involved prolonged mechanical ventilation and noninvasive assisted ventilation use and so on),associated with prolonged intensive care unit stay in patients after cardiac surgery with cardiopulmonary bypass.
1.Introduction
Cardiopulmonary bypass (CPB) is regarded as one of the most important advances in medicine in the 20th century [1].In 2018,approximately 70.85%of cardiovascular operations in 693 hospitals in China were performed under CPB to maintain normal blood circulation without blood interference in the surgical field[2].The most common types of cardiac surgery performed with CPB are heart transplants,combined coronary artery bypass grafts (CABG),and valve surgery[3].Improvements in the versatility and safety of CPB have led to improvements in early outcomes[4].Nevertheless,side effects and postoperative complications associated with CPB still occur,including pulmonary dysfunction [5],atrial fibrillation,neurocognitive changes [6],acute kidney injury [7],inflammation,and coagulation disorders[8].Therefore,it is necessary for patients to stay in the ICU postoperatively to monitor changes in their condition and reduce complications.
Some patients require a prolonged length of stay (LOS) in the ICU after CPB.The definition of prolonged ICU LOS is generally 3-7 days [5,9],while to optimize identification of those at high risk,a definition of>72 h has been adopted[10,11].Prolonged ICU LOS is associated with higher rates of complications,medical care costs,and mortality rates [12-14].Thus,identifying risk factors associated with prolonged ICU LOS after cardiac surgery with CPB could potentially yield multiple benefits.Several factors are associated with prolonged ICU LOS,including age,oxygenation index (PaO2/FiO2ratios),atrial fibrillation grading [15],type and duration of surgery [13],pulmonary hypertension,prolonged ventilation [14],duration of intubation,units of transfused blood,and inotrope infusion time in the ICU [16].
Prolonged ICU LOS can have a variety of adverse effects on patients;therefore,it is particularly important to identify risk factors associated with this parameter.Previous studies[5,9]have focused on preoperative and intraoperative factors associated with prolonged ICU LOS after surgery;however,little is known about early postoperative factors.Some scholars [9,17,18] in Europe and the United States use EuroSCORE or Parsonnet to predict ICU LOS in patients undergoing cardiac surgery,while others have demonstrated that these models are not suitable for use in China[19]due to inequalities in medical resource allocation and institutional policies governing ICU discharge.Here,we investigated possible risk factors for prolonged ICU LOS in a Chinese hospital.The aims of the current study were to investigate the incidence of prolonged ICU LOS after cardiac surgery with CPB and retrospectively identify risk factors associated with prolonged ICU LOS.
2.Methods
2.1.Study design and participants
The present investigation was a retrospective observational study conducted in the ICU of a tertiary hospital in Guangzhou,South China,from June 2015 to June 2017.The study population comprised patients admitted to the ICU after cardiac surgery with CPB.The inclusion criteria were:patients who underwent cardiac surgery (including isolated CABG,isolated or multiple valve surgery,or valve surgery and CABG)with CPB,postoperative admission to the ICU,and age ≥18 years.The exclusion criteria were:patients who died within 72 h after surgery or were transferred from the ICU due to non-therapeutic factors,such as financial difficulties.
2.2.Data collection
The study was approved by the institutional review board of the Anthropology Department at Sun Yat-Sen University (No.SYSUIRBDA20170630),and the requirement for informed consent was waived.With the permission of the hospital and the ICU,the electronic hospital records of patients who underwent cardiac surgery with CPB from June 2015 to June 2017 were accessed,including nursing,operation anesthesia,and CPB records.Data collection was carried out by two graduate students in June 2017.All data were proofread by another person to ensure accuracy.Any doubt about the data was resolved by the clinical teacher and the medical record room manager to the greatest extent possible.Information obtained from the electronic records included demographic details,disease and perioperative clinical data,and ICU LOS.Data collected were based on previous literature reports of variables associated with prolonged ICU LOS.
Preoperative variables include the following:age,sex,education,Body Mass Index (BMI),history of smoking,complications,history of cardiac surgery,New York Heart Association (NYHA)class,ejection fraction,N-terminal pro-brain natriuretic peptide(NT-proBNP),creatine kinase MB (CK-MB),serum creatinine,creatinine clearance rate and type of surgery.Intraoperative variables include the following:emergency,surgery time,duration of CPB,duration of aortic occlusion and red blood cell (RBC).Postoperative variables include the following:PaO2/FiO2within 6 h after surgery,SaO2within 6 h after surgery,NT-proBNP,CK-MB,serum creatinine,creatinine clearance rate,postoperative atrial arrhythmia,postoperative ventricular arrhythmia,prolonged mechanical ventilation and non-invasive assisted ventilation use.We used prolonged ICU LOS following cardiac surgery as the outcome variable.There is no consensus definition of prolonged ICU LOS following cardiac surgery.In China,it is generally accepted that the definition of prolonged ICU LOS is a stay longer than 72 h.
2.3.Data analysis
Normally distributed continuous variables are presented as means and standard deviations (SD).Non-normally distributed continuous variables are presented as medians and interquartile ranges.Categorical variables are presented as frequencies and percentages.Patients were divided into two groups based on whether their ICU stay after surgery was prolonged (>72 h).Univariate analysis was used to evaluate factors potentially associated with prolonged ICU LOS.Quantitative variables were compared using the t-test.The Mann-Whitney test or the Kruskal-Wallis test were used to analyze non-parametric data.Categorical variables were compared using the chi-square test.Two-tailed P values<0.05 were deemed to indicate statistical significance.After univariate analysis of factors that were potentially predictive of a prolonged ICU LOS,all variables with P values<0.05 in that analysis were analyzed via binary logistic regression modeling to identify independent risk factors that predicted a prolonged ICU LOS.IBM SPSS version 25 was used for statistical analyses.
3.Results
3.1.Patient population
The study population included 395 patients who underwent cardiac surgery with CPB and were subsequently admitted to the ICU.Their mean age was 58 years,47.1%were women,and 6.3%had a history of cardiac surgery.Valve surgery was the most frequently performed procedure (59.5%).The median ICU LOS was 50.9 h.A total of 137 patients(34.7%)had prolonged stays(>72 h)in the ICU.All demographic characteristics are shown in Table 1.
3.2.Univariate analysis
In univariate analysis,16 variables were associated with a prolonged ICU stay at a significance level of P<0.05(Table 1),including age,NT-proBNP,surgery type,history of cardiac surgery,hypertension,and NYHA class.Intraoperative variables that differed significantly between the prolonged and the non-prolonged ICULOS groups in the univariate analysis included surgery time,duration of CPB,RBC,and duration of aortic occlusion (Table 2).
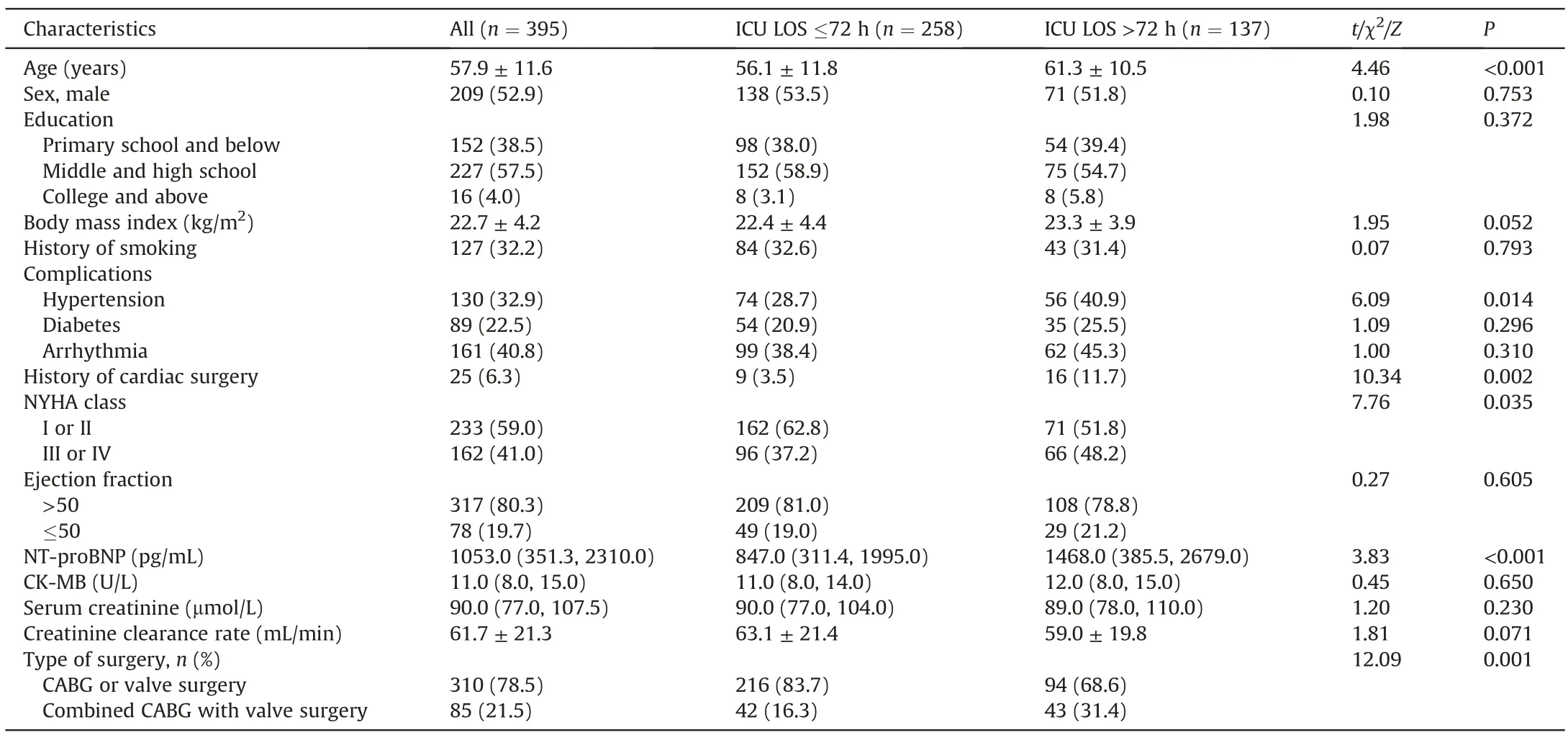
Table 1 Patient characteristics before cardiac surgery with cardiopulmonary bypass.
The results of univariate analysis of associations between postoperative variables and ICU LOS are shown in Table 3.PaO2/FiO2,postoperative atrial arrhythmia,postoperative ventricular arrhythmia,non-invasive assisted ventilation use,NT-proBNP,and prolonged mechanical ventilation differed significantly between the prolonged and non-prolonged ICU LOS groups(all P <0.001).
3.3.Logistic regression analysis
Eight risk factors significantly associated with prolonged ICU LOS in binary logistic regression analysis are shown in Table 4.The factor most significantly associated with prolonged ICU LOS was non-invasive assisted ventilation use,with an odds ratio (OR) of 7.713 and a 95% confidence interval (CI) of 2.987-19.918(P <0.001).Other factors significantly associated with prolonged ICU LOS included prolonged mechanical ventilation,Oxygenation Index,postoperative ventricular arrhythmia and postoperative atrial arrhythmia.Finally,the logistic regression model was statistically significant (χ2=173.766,P <0.001).The resulting model passed the Hosmer-Lemeshow test(P=0.538).
4.Discussion
In the current study,which was conducted at a single center in China,the rate of prolonged ICU LOS (>72 h) after cardiac surgery with CPB was 34.7%,which is substantially higher than that reported in some other studies such as Nakasuji(13.0%)[20].Patients with prolonged ICU LOS after cardiac surgery are reportedly more likely to experience postoperative complications and higher ICU hospitalization costs,and identifying risk factors for prolonged ICU LOS may contribute to reducing these burdens.Several conclusions can be drawn from the data generated in the present study.
The five postoperative risk factors independently significantly associated with prolonged ICU LOS in the current study were:oxygenation index within 6 h after surgery,atrial arrhythmia,ventricular arrhythmia,prolonged mechanical ventilation,and non-invasive assisted ventilation use.The lung function of patients with non-invasive auxiliary ventilation is impaired and airway management is comparatively difficult in such patients,which can affect their ICU LOS.Second,mechanical ventilation duration was longer in patients with prolonged ICU LOS in the current study,consistent with some previous investigations,in which prolonged mechanical ventilation was associated with longer ICU LOS[21,22].Weaning may be delayed in patients who require assisted ventilation,such as those with ventilator-associated lung injury and pneumonia[23-25],and such patients may therefore spend moretime in the ICU.
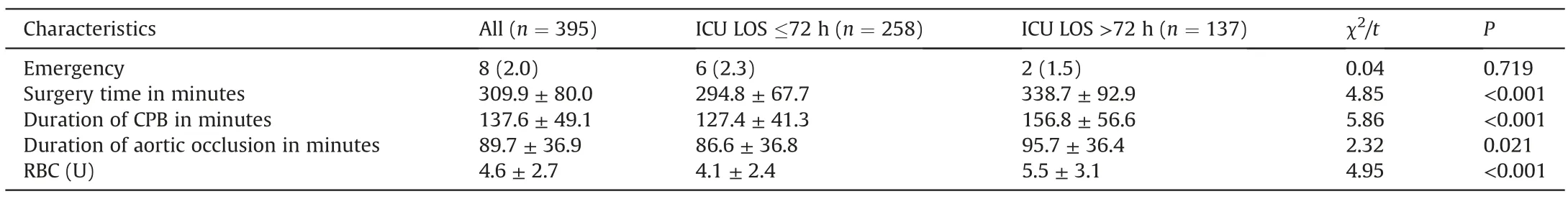
Table 2 Patient characteristics during cardiac surgery with cardiopulmonary bypass.
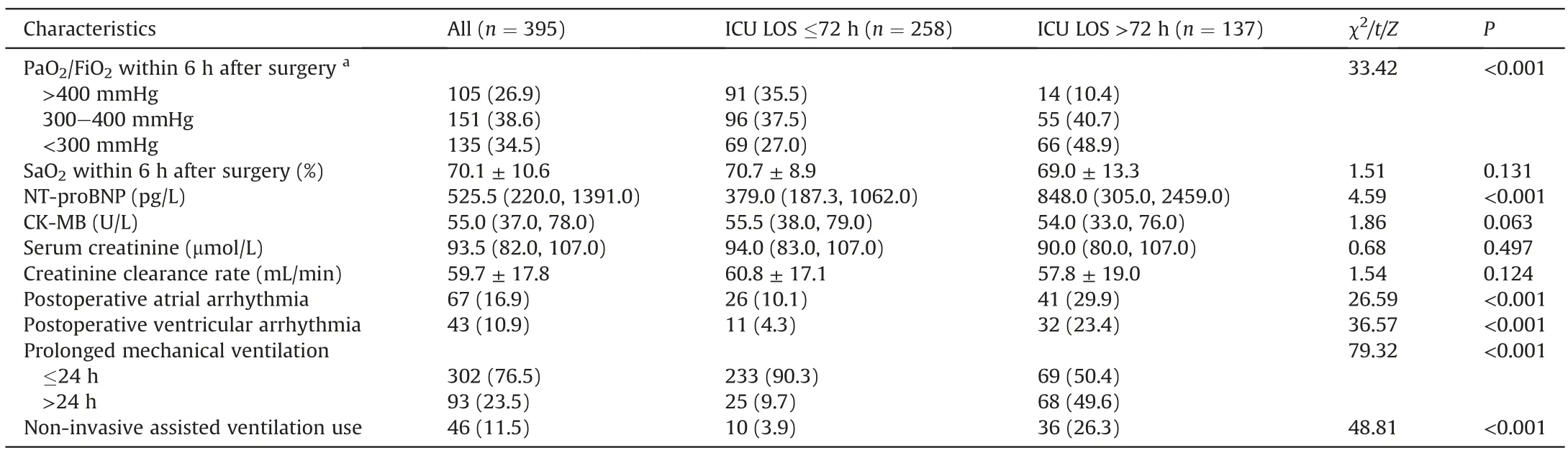
Table 3 Early postoperative characteristics of patients after cardiac surgery with cardiopulmonary bypass.
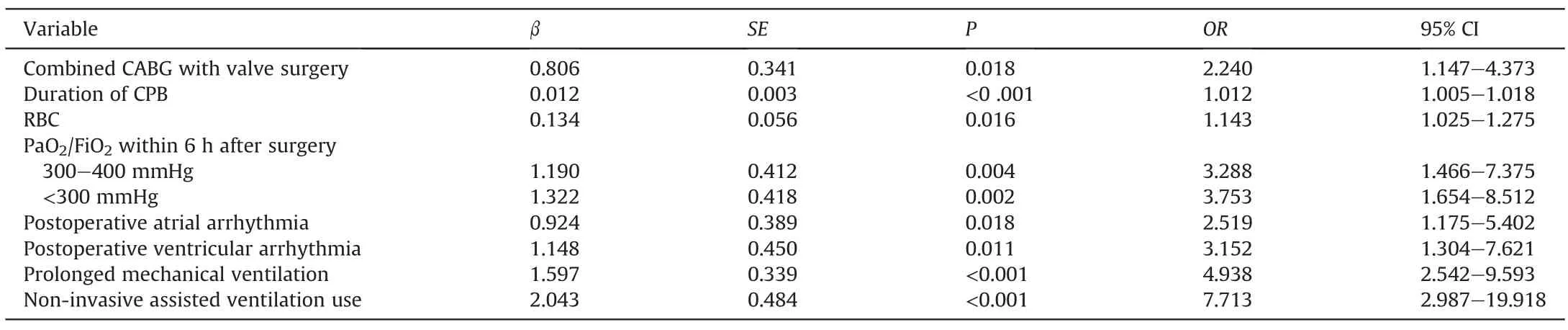
Table 4 Logistic regression analysis of patient length of stay in the intensive care unit after cardiopulmonary bypass adjusted by age and sex (n=395).
In the present study,patients with prolonged ICU LOS were more likely to exhibit ventricular and atrial arrhythmia following surgery.Arrhythmia is a common symptom of cardiovascular diseases,and malignant arrhythmia is characterized by rapid onset and rapid deterioration.In one study that monitored patients after coronary surgery with CPB,atrial fibrillation was a significant risk factor for prolonged ICU LOS[26].Further,a systematic review that assessed factors influencing ICU LOS after cardiac surgery in adults found that atrial fibrillation/arrhythmia was associated with increased ICU LOS [5].A predictable reduction in the likelihood of arrhythmias may contribute to reducing ICU LOS.The observation in the current study that oxygenation index within 6 h after surgery significantly influenced ICU LOS may be due to the use of noninvasive assisted ventilation after cardiothoracic surgery which improves oxygenation.Previous studies [27] have shown that a lower oxygenation index is associated with a longer stay in ICU and higher in-ICU mortality.It is relatively simple for nurses to detect a low oxygenation index after cardiac surgery through early observation of patients [28],allowing doctors to receive timely information and perform the early intervention.
Type of surgery was an independent significant predictive preoperative risk factor associated with prolonged ICU LOS in the current study.The risk of prolonged ICU LOS in patients who underwent combined CABG with valve surgery was 2.240 times higher than that of patients who underwent CABG or valve surgery alone (P=0.018).Ghotkar et al.[29] analyzed data from 5,186 patients who underwent combined CABG,and reported that those with hypertension tended to have longer ICU LOS,which is consistent with the results of the current study.
Two independently significant intraoperative risk factors for prolonged ICU LOS were identified in this study:duration of CPB and RBC during surgery.Further,this study showed that intraoperative blood infusion is a factor influencing prolonged ICU LOS,along with RBC during surgery.In an observational study that included 20,377 patients who underwent cardiac surgeries at 39 hospitals in the USA,transfusions were administered to 36.8% of patients [30].Similar to previous investigations [31,32],in this study,the use of blood products due to hemorrhage was identified as a predictor of ICU LOS >72 h.In addition,in the present study,CPB duration contributed to prolonged ICU LOS,indicating that patients with more complex conditions or undergoing complicated operations are more likely to have prolonged ICU LOS.This is consistent with previous reports [5,33,34].
In this study,the rate of prolonged ICU LOS after cardiac surgery with CPB was high,which suggests that healthcare workers should pay attention to and strengthen the management of such patients.The risk factors identified in this study can serve as a reference for the identification or intervention of prolonged ICU LOS.Firstly,it suggests that clinical workers should pay more attention to patients with these risk factors,strengthen care management,reduce the impact of these factors on patients,and thus reduce the incidence of prolonged ICU LOS.Secondly,it suggests that clinical workers can evaluate the risk of ICU LOS in patients after cardiac surgery with CPB in advance.Moreover,it can also provide references for medical staff to formulate appropriate treatment and nursing plans.Finally,the findings of this study may inspire clinicians to develop a risk prediction tool for prolonged ICU LOS after cardiac surgery with CPB in order to increase the efficiency of patient care.
The current study has some limitations.As it was a retrospective investigation,the associations identified do not necessarily imply causation.The study participants were all derived from a single,comparatively well-resourced,urban tertiary hospital,potentially limiting the broader applicability of the study results.In addition,there are potential omitted risk factors in this study.Furthermore,because of the limited research sample,we only included CABG and valve surgery in this study.Other types of cardiac surgery performed with CPB were excluded,such as heart transplant,atrioventricular deficiency repair,etc.Thus the generalization of the results needs further examination.Finally,the sample size was relatively small.
5.Conclusions
The incidence of prolonged ICU LOS after cardiac surgery with CPB is high and influenced by numerous factors.These preoperative,intraoperative,and early postoperative independent risk factors suggest that a comprehensive assessment should be conducted with early evaluation.Combined CABG with valve surgery,infusion during surgery,and longer duration of CPB may be useful factors for identifying cardiac surgery patients at risk of increased ICU LOS.Close attention should be paid to indicators during early postoperative monitoring to facilitate correction of atrial and ventricular arrhythmia as soon as possible,maintain the stability of respiratory circulation,and prevent complications.To reduce ICU LOS,we need to identify patients at risk of prolonged ICU LOS.
Funding
This work was supported by the Science and Technology Planning Project of Guangdong Province,China [grant numbers 20160910].
Data availability statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Credit authorship contribution statement
Xueying Zhang:Conceptualization,Formal analysis,Writingoriginal draft preparation.Wenxia Zhang:Data curation,Formal analysis,Writing-original draft preparation.Hongyu Lou:Conceptualization,Investigation,Writing-original draft preparation.Chuqing Luo:Data curation,Validation,Writing-original draft preparation.Qianqian Du:Methodology,Investigation,Writingoriginal draft preparation.Ya Meng:Methodology,Data curation,Writing-original draft preparation.Xiaoyu Wu:Investigation,Software,Writing-original draft preparation.Meifen Zhang:Conceptualization,Supervision,Writing-reviewing and Editing,Project administration,Funding acquisition.
Declaration of competing interest
The authors declared no conflict of interest.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2021.09.002.
杂志排行
International Journal of Nursing Sciences的其它文章
- Second-order problem solving:Nurses’ perspectives on learning from near misses
- Exploring the employment readiness and return to work status of breast cancer patients and related factors
- Resilience of nurses at the epicenter of the COVID-19 pandemic in Lebanon
- A study of the relationship between nurses’ experience,structural empowerment,and attitudes toward computer use
- Mobile health applications for the care of patients with breast cancer:A scoping review
- Nursing students’ attitudes toward mobile learning:An integrative review
