Vitreous haemorrhage as the first presentation of undiagnosed Waldenstrom macroglobulinemia
2021-11-08ChristinaLimHuzaifaMalickSomnathBanerjee
Christina S Lim, Huzaifa Malick, Somnath Banerjee
Dear Editor,
Waldenstrom macroglobulinemia (WM) is a rare type of non-Hodgkin’s lymphoma, commonly associated with hyperviscosity syndrome. Unlike non-Hodgkin’s lymphoma,its ocular manifestations are less well described in the literature. Here we present the first case of undiagnosed WM presenting with dense vitreous haemorrhage. The study was conducted in accordance with the principles of the Declaration of Helsinki. The informed consent was obtained from the subject.
CASE HISTORY
A 67-year-old man presented to eye casualty with one day history of sudden reduction in vision in the right eye. Visual acuity (VA) was hand movement. He reported no symptoms in the left eye (VA 6/6). There was no history of trauma. He had no past medical history and ophthalmic history except for mild myopia. On examination, anterior segments were unremarkable. Intraocular pressures were 16 mm Hg in both eyes. There was a dense vitreous haemorrhage in the right eye with very little fundal view. In the left eye, there were some scanty retinal haemorrhages over the inferior arcade with clear vitreous. B-scan ultrasonography of the right eye showed flat retina with no obvious retinal or choroidal lesions (Figure 1A).Two days later, he developed Roth spots in the left fundus. On systemic review, it was discovered that he recently experienced epistaxis. On blood tests, his haemoglobin was 56 g/L, white blood cell count 85.2×103/mL, plasma viscosity 5.45 mPa/s,and IgM paraprotein level 4160 mg/dL. He was referred to haematology and was diagnosed with WM. He received two plasma exchanges to remove paraproteins and to reduce plasma viscosity. He was followed up again in the eye clinic in just over two weeks following presentation and the vision was 0.0 logMAR in both eyes. Fundus examination showed reducing vitreous haemorrhage in the right eye along with central and peripheral retinal haemorrhages with tortuous veins and venous “sausaging” but no intraocular masses (Figure 1B).In the left eye, the retinal haemorrhages previously noted were also improving. He later received chemotherapy and his IgM paraprotein level was 520 mg/dL and plasma viscosity 1.61 mPa/s. The fundus examination following chemotherapy was normal.
DISCUSSION
Non-Hodgkin lymphoma (NHL) represents a diverse spectrum of immune system malignancies where 85%-90% are derived from B cells[1]. It is the eleventh commonest cancer in the world in incidence[2]. More than 90% of lymphomas with ocular involvement are NHL[3]and it is reported that intraocular involvement is seen in 1% of NHL[4]. It is difficult to estimate the incidence and trend of intraocular lymphomas[3]but one study estimates to be 21 per 100 000 patients who require referral to the eye hospital per year[5]. Typical symptoms of intraocular lymphomas include floaters and blurred vision[6].Ocular manifestations of NHL are well described in the literature. Non-Hodgkin’s intraocular lymphoma typically masquerades as intermediate or posterior uveitis and affects the vitreous, the retina, the retinal pigment epithelium and the optic nerve[7].
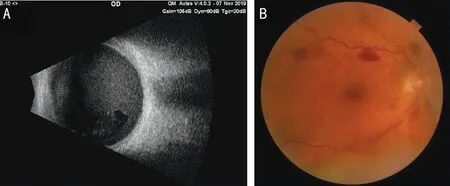
Figure 1 Further imaging of the left eye demonstrating ophthalmic manifestations of WM A: B-scan ultrasonography of the right eye showed flat retina with no obvious retinal or choroidal lesions; B: Fundus photograph of the right eye showing reducing vitreous haemorrhage with central and peripheral retinal haemorrhages with tortuous veins and venous “sausaging”.
WM is a B-cell lymphoproliferative disorder characterised by bone marrow infiltration, a rare type of NHL[8]. The incidence is reported to be between 2-6 per million per year in the United States[9]. Extramedullary sites are rarely involved but include lungs, central nervous system and soft tissues[8]. In contrast to NHL in general, its ocular involvements are less well reported. There are few studies reporting conjunctival involvement[8], the superior rectus muscle[10], bilateral central retinal vein occlusions[11-12], birdshot chorioretinopathy[13],adnexal mass involving extraocular muscles[14], and serous retinal detachment[15]. However, none of the cases report such dramatic, sudden reduction in vision by vitreous haemorrhage as a clinical feature nor as a presenting complaint of undiagnosed WM. The most notable feature of WM is the hyperviscosity syndrome which is a haematological condition where blood, plasma or serum viscosity are elevated[16]. It is present in 10%-30% of patients with WM[17], associated with paraproteinemia[18], where its level has a direct effect on the plasma viscosity[19]. Associated retinal findings include dot and blot haemorrhages and tortuous, dilated blood vessels(venous “sausaging”)[16]. Menkeet al[20]classified the patient cohort with WM into three groups: group 1 included patients with no retinal changes; group 2 had those with dilated retinal veins and/or peripheral retinal haemorrhages (mean serum IgM 5442 mg/dL, mean serum viscosity level 3.1 mPa/s);group 3 with peripheral and central retinal haemorrhages accompanied by dilated veins, optic nerve head oedema or venous sausaging (mean serum IgM 8515 mg/dL, mean serum viscosity level 5.6 mPa/s). The retinal signs and serum viscosity (5.45 mPa/s) of our patient would be classified as group 3 but his IgM paraprotein level (4160 mg/dL) as group 2 (range 2950-8440 mg/dL). Although this does not explain the unusual presentation of our patient, it is interesting to note that the white cell count was extremely high 85.2×103/mL.The white blood cell also contributes to serum viscosity and extreme concentrations of white blood cells can also cause hyperviscosity. This would explain the high serum viscosity in our patient (group 3) compared to the lower the IgM paraprotein level (group 2). With high serum viscosity, the blood flow slows down, however, autoregulation of retinal vasculature ensures a constant rate of flow[21]. This leads to the dilatation of both retinal arteries and veins. When the retinal arteries and arterioles dilate, this results in higher intravascular pressures to be carried over to the venous side,hence retinal haemorrhages[20]. In our patients, it is possible that the extremely high white cell count has contributed to the higher serum viscosity than what it would be given the IgM paraprotein level and caused vitreous haemorrhage from a high intravascular pressure without new vessel formation.
To our knowledge, this report describes the first case of vitreous haemorrhage leading to the diagnosis of WM with good vision outcome with systemic treatment.
ACKNOWLEDGEMENTS
Conflicts of Interest:Lim CS, None; Malick H, None;Banerjee S, None.
杂志排行
International Journal of Ophthalmology的其它文章
- lmpact of intraocular pressure fluctuations on progression of normal tension glaucoma
- Effective treatment for secondary angle-closure glaucoma caused by traumatic lens subluxation:phacoemulsification with capsular-tension-ring implantation combined with ophthalmic endoscopecontrolled goniosynechialysis
- Efficacy and safety of newly developed preservativefree latanoprost 0.005% eye drops versus preserved latanoprost 0.005% in open angle glaucoma and ocular hypertension: 12-week results of a randomized,multicenter, controlled phase III trial
- Progressive restrictive strabismus in an infant
- Association of peripheral anterior synechia, intraocular pressure, and glaucomatous optic neuropathy in primary angle-closure diseases
- Protective effect of LIF-huMSCs on the retina of diabetic model rats