Three colonic cancers,two sites of complete occlusion,one patient:A case report
2021-10-09EricBergeronThibautManiereXuanVienDoMichaelBensoussanEricDeBroux
Eric Bergeron,Thibaut Maniere,Xuan Vien Do,Michael Bensoussan,Eric De Broux
Eric Bergeron,Department of General Surgery,Charles-LeMoyne Hospital,Greenfield Park J4V2H1,Quebec,Canada
Thibaut Maniere,Michael Bensoussan,Department of Gastroenterology,Charles-LeMoyne Hospital,Greenfield Park J4V2H1,Quebec,Canada
Xuan Vien Do,Department of Medical Imaging,Charles-LeMoyne Hospital,Greenfield Park J4V2H1,Quebec,Canada
Eric De Broux,Department of Digestive Surgery,Centre Hospitalier Universitaire de Montréal,Montreal H2X3E4,Quebec,Canada
Abstract BACKGROUND Synchronous colonic cancer incidence is uncommon,and awareness about this rare condition is improved recently.However,in the presence of acute colonic obstruction,investigation and management of synchronous colonic cancer can be difficult and challenging.CASE SUMMARY A patient presented with acute colonic obstruction with impending rupture and complete examination of this patient revealed the presence of three colonic cancers,of which two were completely occluding.CONCLUSION The presence of multiple colonic cancers must be ruled out in order to plan the best management.We present the case with a review of literature and discuss the management of the case.
Key Words:Colon cancer;Synchronous cancers;Colonoscopy;Obstructive cancer;Colostomy;Case report
INTRODUCTION
Colorectal cancer (CRC) is the third most commonly diagnosed malignancy and the fourth leading cause of cancer death in the world[1].The frequency of synchronous CRC (sCRC) may reach 20% in patients with familial adenomatous polyposis,hereditary non-polyposis colorectal cancer,chronic ulcerative colitis[2] and serrated polyposis syndrome[3].In patients without these risk factors,prevalence of sCRC is estimated to be 3.5%[4],while the current improved awareness increased these estimates from 5% up to 8.4%[5-7].
Reports on the occurrence of triple or more sCRC range from 0.1% to 0.7%[8-13],and up to 1.6% in a recent review[7].This review described a series of 1005 patients,of whom seven patients (0.7%) had four CRC and one patient (0.1%) had 5 CRC[7].In another case,up to seven CRC in the same patient have been reported[14].The importance of preoperative endoscopic examination of the entire colon to rule out polyps or secondary cancers is well established.However,in emergency situations such as obstruction,perforation or ischemic disease,management may become particularly challenging[1,15,16].
We report a patient who presented with acute and severe obstruction of the sigmoid colon due to a cancer,which was managed initially with a loop colostomy.The patient was subsequently discovered to have two more cancers on the right side,one of which was also completely occluding the caecum.The case and its management are discussed.
CASE PRESENTATION
Chief complaints
A 77-year-old patient presented at the emergency room on February 13th,2019,with an overly distended abdomen.
History of present illness
The patient was vomiting fecaloid material for the last 24 h.He passed no stools or gas in the last three days.
History of past illness
The patient reported rectal bleeding for almost one year.He never had colonoscopy.
Personal and family history
The patient is a diabetic male with obesity (Body mass index = 35).There is no personal or familial history of polyposis or inflammatory bowel disease.There was no colonic cancer in the family of the patient.
Physical examination
Upon arrival,vital signs were within the normal limits.The patient was afebrile.The abdomen was very tense but without signs of peritonitis.There was no mass on rectal exam.
Laboratory examinations
Hemoglobin,white cell count,liver and renal function tests were within normal limits.Carcinoembryonic antigen (CEA) was 2.3 µg/L;(Normal:0-4.9 µg/L).Colonoscopy was well tolerated.An obstructive cancer of the proximal sigmoid colon was confirmed.Two other cancers were found on the right side:one at the caecum and another one at the mid part of the ascending colon.No polyposis was found.
Imaging examinations
Computed tomography (CT)-scan showed significant dilatation of the small bowel loops and colon,secondary to a neoplastic sigmoid lesion (Figure 1).Some free fluid was also seen.There was no evidence of metastatic disease.Retrospectively,caecal(Figure 2A) and middle right colonic tumors (Figure 2B) could be identified on CTscan but were difficult to diagnose prospectively in an emergency setting without associated acute bowel caliber change.
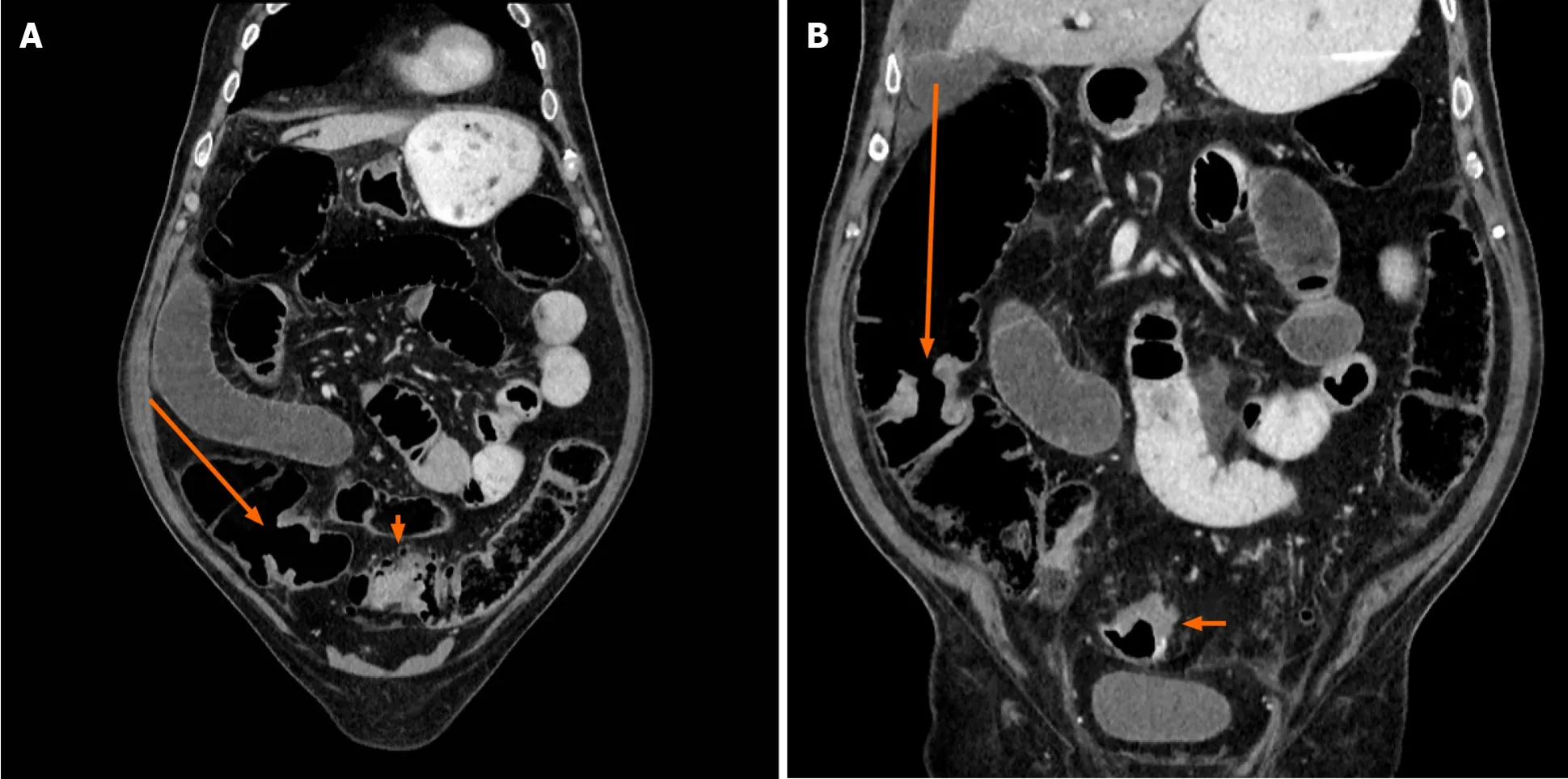
Figure 2 Coronal contrast-enhanced computed tomography image.
FINAL DIAGNOSIS
Three colonic cancers.Occlusive cancers at the ileocaecal valve and at sigmoid colon.Final pathology report identified three adenocarcinomas.The sigmoid cancer was a pT4 adenocarcinoma,invading the surrounding tissues.Incidentally,there was a concealed perforated diverticulitis.The cancer of the caecum was a pT3 obstructing adenocarcinoma at the ileocaecal valve.The lesion of the ascending colon was a circumferential pT3 adenocarcinoma.It was situated 10 cm distally from the cancer of the caecum.Seven nodes were positive for the presence of metastasis.There was no polyp and no evidence of inflammatory bowel disease.TNM classification was T4N2M0.
TREATMENT
The patient was initially hydrated.A nasogastric tube was installed,which evacuated brownish material.The patient was brought to the operating room during the evening and a left-sided loop colostomy was carried out.The colostomy was fashioned through a small left paramedian incision directly over the junction of the descending and sigmoid colon.
During the postoperative period,the colostomy was functional and allowed the stools to evacuate.The size of the abdomen significantly reduced.This window permitted the evaluation and stabilization of the medical condition of the patient.A colonoscopy was done through the rectum and to the proximal colonviathe colostomy.
The patient was planned for a total colectomy with ileorectal anastomosis,nine days after the first intervention.Meanwhile,there was recurrence of abdominal distension and the discharge from colostomy had become minimal.The intervention was done through a midline incision.It was technically difficult owing to the distended small bowel,secondary to an evident occlusion from the tumor of the caecum.The intestinal wall was diffusely thickened demonstrating a process originating for many weeks.There was no evidence of peritoneal metastases.A subtotal colectomy was carried out keeping as much distal sigmoid as possible to allow a side-to-side ileosigmoid anastomosis and alleviate potential postoperative diarrheas.
One week later,postoperative course became complicated with an anastomotic leak that was treated with reoperation,drainage and proximal ileostomy.The patient had a further complicated course with abdominal abscesses,pneumonia,and enterocutaneous fistula originating from small bowel proximal to the ileostomy.This latter was treated with bowel rest and parenteral nutrition.
OUTCOME AND FOLLOW-UP
Hospital stay was for almost six months.Before discharge,the patient was reoperated after ensuring that the ileocolonic anastomosis was free of leakage and permeable.A short resection of the small bowel was done at the site of fistula and the ileostomy was closed.Postoperative period was uneventful.Because of the complicated postoperative course and the delay at discharge from the surgery,adjuvant chemotherapy was not planned.
One year later,there was no clinical or radiologic evidence of recurrent or metastatic disease.CEA was 5.8 µg/L (Normal:0-4.9 µg/L).Endoscopic examination of the remaining 30 cm of the rectum and colon showed no lesion.An incisional hernia was repaired.Two years later,the patient is still functioning well and in good condition.However,CEA was found to be increased to 17.1 µg/L (Normal:0-4.9 µg/L)subsequently,but no recurrent disease could be demonstrated with thoracoabdominal CT scan and positron emission tomography-CT.However,favourable clinical evolution notwithstanding,locoregional recurrence remains of concern.
DISCUSSION
CRC is the second and third most common malignancy in males and females,respectively[1,3,7].Synchronous CRC is reported between 3% and 8% in recent reports on large groups of patients[5,6,11,12,17].Incidence of sCRC reaches 20% in patients with risk factors[2,3].Mean prevalence of sCRC is estimated at 3.5%[4].
Occurrence of three or more colon cancers at the same time in an individual is an unusual situation[7-13,15,18,19] but such incidence has been reported to be up to 1.6%[7].Reports of the occurrence of two or more sCRC up to 12%[20] emphasize the mandatory investigation of the entire colon to rule out synchronous tumors and plan proper management[21].
The more challenging cases occur in patients presenting with a surgical emergency.Fifteen to 30% of sCRC cases present as an emergency occlusive situation[1,22,23].The sigmoid colon is the most common location of CRC obstruction;75% of the tumours are located distal to the splenic flexure[21].
In the present case,initial management was dictated by the overly distended abdomen in the patient in bad condition.Facing an occlusive sigmoid cancer while unaware of the concurrent occlusive caecal cancer,the possible management options at this time were proximal colostomy,Hartmann’s procedure or total colectomy[1].However,the last two options take longer time and may be technically challenging,because of intestinal distension as well as potentially threatening procedures for the patient[1].
The colostomy allowed the patient to be stabilized and medically evaluated for subsequent procedure.Impending rupture of the colon and presence of stools contraindicated colonoscopy right after creating the colostomy.The colostomy should have allowed the obstruction to resolve but in this particular case,the occlusion of the ileocaecal valve,imperceptible at the time of initial intervention,eventually failed to achieve this goal.On the other hand,the necessity to investigate the entire colon and rectum was realized.Moreover,the obstruction at ileocecal valve was not complete initially since the oral preparation for the colonoscopy was effective.
It is important to completely visualize the proximal colon through the colostomy,as well as the distal part of the large bowel through the rectum.Colonic stenting as a bridge to definitive surgery[24-26] was not considered in this situation due to potential impending rupture and immediate unavailability of this modality.Moreover,stent of an obstructing cancer is yet to be recommended as a standard treatment,and colonoscopy may be dangerous through a colonic stent even though feasible[26].The colon may also be satisfactorily evaluated with imaging modalities (virtual coloscopy,CTcolonography,magnetic resonance colonography,intra-operative or post-operative coloscopy)[1,15,20,27].Thus,every reasonable effort should be made to evaluate the entire colon before planning definitive intervention[26].
If the obstructing lesion of the caecum had been identified initially,a total colectomy with or without ileostomy could have been carried out.However,due to the bad condition of the patient,such a procedure would have been technically difficult and potentially risky.A simple ileostomy would have left in place a close loop obstruction of the colon with a remaining risk of rupture.The proper management would have probably been damage control procedure with laparotomy,loop colostomy and ileostomy,leaving an open abdomen,stabilizing the medical condition,allowing the intestine to decompress,and proceeding with total or subtotal colectomy and ileocolonic anastomosis.Whatever the contemplated intervention,either of the options was associated with major concerns.
The complicated and prolonged postoperative course is unfortunate and beyond the scope of discussion.Consequently,the patient could not receive adjuvant chemotherapy.In spite of the complicated issues,primary ileocolonic anastomosis remained,in our opinion,the proper choice either at the first procedure or subsequently[1].The presence of two completely obstructing lesions at two different sites is very unique but complicated the management of the patient and surely contributed to the outcome.
This case emphasizes the importance to keep in mind,the possibility of additional colonic cancers that could be difficult to identify particularly in emergency and complicated situations.Reasonable efforts must be made to evaluate the entire colon in order to plan definitive management.A temporary colostomy in severe colonic obstruction allows the obstruction to resolve,the colon to be entirely evaluated,and the patient to be stabilized for definitive management.A total colectomy cannot be recommended straightaway[1] since a frequency of 3.5% for synchronous cancers[4]does not justify such an extensive procedure.Similarly,if a Hartmann’s procedure is done,investigation of the colon is mandatory before reoperation.
CONCLUSION
Considering this case and the review of literature,we can draw the following conclusions and recommendations:(1) Colon cancer has a high incidence,with a rate of sCRC between 3% and 12%,and thus represents a not so rare condition;(2)Obstructing colonic cancer is frequent at initial presentation and carries the same prevalence of sCRC;(3) A colostomy allows relieving obstruction of the colon and stabilization of a patient and gives access to the entire colon for investigation;(4) Every effort should be made to evaluate the entire colon and rectum before definitive treatment;and (5) The presence of two obstructing cancer at the same time remains a unique situation and management can be difficult.
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Trends of rapamycin in survival benefits of liver transplantation for hepatocellular carcinoma
- Role of minimally invasive techniques in gastrointestinal surgery:Current status and future perspectives
- Fluorescence in situ hybridization-based confirmation of acute graftvshost disease diagnosis following liver transplantation:A case report
- Perioperative steroid administration reduces overall complications in patients undergoing liver resection:A meta-analysis
- Literature review of the outcome of and methods used to improve transperineal repair of rectocele
- Quality of life after colorectal surgery:A prospective study of patients compared with their spouses
