Low-pressure pulse flushing choledochoscopy combined with neodymium laser lithotripsy for the treatment of intrahepatic bile duct stones
2021-09-23WenLongZhngZhePingFngBinYoShiTingChenShngDongLvChengWngPengHuBioZhng
Wen-Long Zhng ,Zhe-Ping Fng ,Bin-Yo Shi ,Ting Chen ,Shng-Dong Lv ,Cheng Wng ,Peng Hu ,F-Bio Zhng ,*
a Department of Hepatobiliary Surgery, Taizhou Hospital of Zhejiang Province, Wenzhou Medical University, Taizhou 3170 0 0, China
b Department of Hepatobiliary Surgery, Enze Hospital, Wenzhou Medical University, Taizhou 3180 0 0, China
Cholelithiasis is a common and frequently occurring disease in East Asia.Intrahepatic bile duct stone is a benign disease,but the recurrence rate is high.The incidence of postoperative residual stones after traditional manual stone removal can be 30%-96% [1] .The emergence of endoscopes is therefore a milestone in the treatment of hepatolithiasis.Among the various approaches,choledochoscopy combined with laser lithotripsy has become the main procedure for intrahepatic bile duct stone removal [2] .Lithotripsy alone has the disadvantages of low stoneremoving efficiency and blurred choledochoscope vision while performing the procedure.Currently,our team has achieved satisfactory results in the removal of intrahepatic bile duct stones with low-pressure pulse flushing and neodymium laser lithotripsy.
This retrospective study included 23 patients (10 males and 13 females),with a median age of 58.5 (range:34-78) years,who underwent choledochoscopic neodymium laser lithotripsy between January 2018 and May 2020.The selection criteria were:1) aged 18 years and above;2) a diagnosis of intrahepatic and extrahepatic bile duct stones via ultrasound,computed tomography (CT),magnetic resonance cholangiopancreatography (MRCP),etc.;3) Child-Pugh liver function classified as grade A or B;and 4) patient can tolerate this procedure.The exclusion criteria were:1) malignant diseases of intrahepatic and extrahepatic bile ducts;2) severe abnormal heart and lung function;and 3) abnormal coagulation function and obvious bleeding tendency.
We performed bile duct exploration to determine for which cases choledochoscopic neodymium laser lithotripsy was feasible.Firstly,the tip of the ureteral catheter was placed in the posterior of the stone through the working channel of the choledochoscope.Next,the ureteral catheter was retained,and we exited the choledochoscope.Then,the choledochoscope was re-entered along the ureteral catheter to the front of the stone.Finally,the end of the ureteral catheter was connected to joint.At the same time,a 50 mL syringe for low-pressure pulse water injection was connected by the assistant,while the choledochoscope channel water injection was suspended and supplemented by intermittent suction.Continuous suction and active irrigation throughout the lithotripsy were successfully used to maintain adequate visibility during the procedure (Fig.1 A-H).The low-pressure pulse flushing laser lithotripsy device consisted of an F5 ureteral catheter and a joint (Fig.1 I).A needle was employed to puncture holes into the side wall of the tip of the F5 ureteral catheter,without cutting off its head (Fig.1 J).
Patients were followed up after treatment with neodymium laser lithotripsy.Follow-up examinations included T-tube cholangiography,ultrasonography,abdominal CT,and laboratory tests.Stones detected in the intrahepatic bile duct within three months after therapy were considered residual stones.The occurrence of any operative complication was recorded during patient follow-up or telephone interview.
All the patients underwent low-pressure pulse flushing laser lithotripsy.During laser lithotripsy,the low-pressure pulse flushing device allowed great vision,and the neodymium laser enabled continuous lithotripsy with no stone migration observed.The mean stone size was 20 mm and measurement was based on the maximum length.Of the 23 cases,3 had>10 stones.There were 8 cases with stones in the left intrahepatic bile ducts,7 in the right intrahepatic bile ducts,8 in the bilateral bile ducts,and 22 cases complicated with cholangitis (Table 1,Fig.2 A-C).No complications occurred except for one patient having an infected incision after operation.Five of the 23 patients underwent segmental hepatectomy combined with low-pressure pulse flushing laser lithotripsy.The median operative time,hospital stay,and postoperative hospital stay for patients undergoing low-pressure pulse flushing laser lithotripsy were 270.1 (range:135.0-470.0) min,15.0 (range:10.0-27.0) days and 9.8 (5.0-23.0) days,respectively.The stones were removed from the T-tube sinus choledochoscope three months after the operation.After the first operation,the imaging examination showed that stone-free rate of the low-pressure pulse flushing laser lithotripsy was 43% (10/23),with thirteen patients failed because the stones were impacted in the bilateral bile duct,stag horn calculi,or associated with bile duct stricture.All the failed patients underwent a second operation,and the final stone-free rate was 91% (21/23) with 2 patients failed because of bile duct stricture of the right liver (Fig.2 D).No postoperative mortality (within 30 days) or recurrence of stones was observed (Fig.2 E,F),and the median follow-up was 14.9 (range:3.1-30.7) months (Table 2).
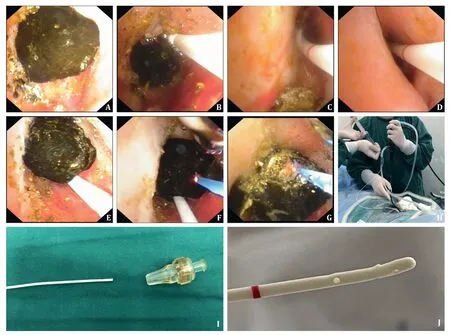
Fig.1.A:Choledochoscope to detect intrahepatic bile duct stone.B:An F5 ureteral catheter was inserted through the choledochoscope channel,and the tip of the ureteral catheter was placed 2 cm above the distal end of the stone.C:The ureteral catheter was fixed and maintained and then the choledochoscope was exited.D:Choledochoscopy was again performed along the ureteral catheter.E:Detection of intrahepatic bile duct stones.F:Insertion of the neodymium laser to prepare lithotripsy.G:Low-pressure pulse flushing choledochoscopy combined with holmium laser lithotripsy,clear vision of lithotripsy,continuous lithotripsy.H:Operation using a choledochoscope and ureteral catheter.I:Low-pressure pulse flushing laser lithotripsy device consisted of an F5 ureteral catheter and a joint.J:A 5 mL needle was used to puncture a hole into the side wall of the head end of the F5 ureteral catheter without cutting off its head.
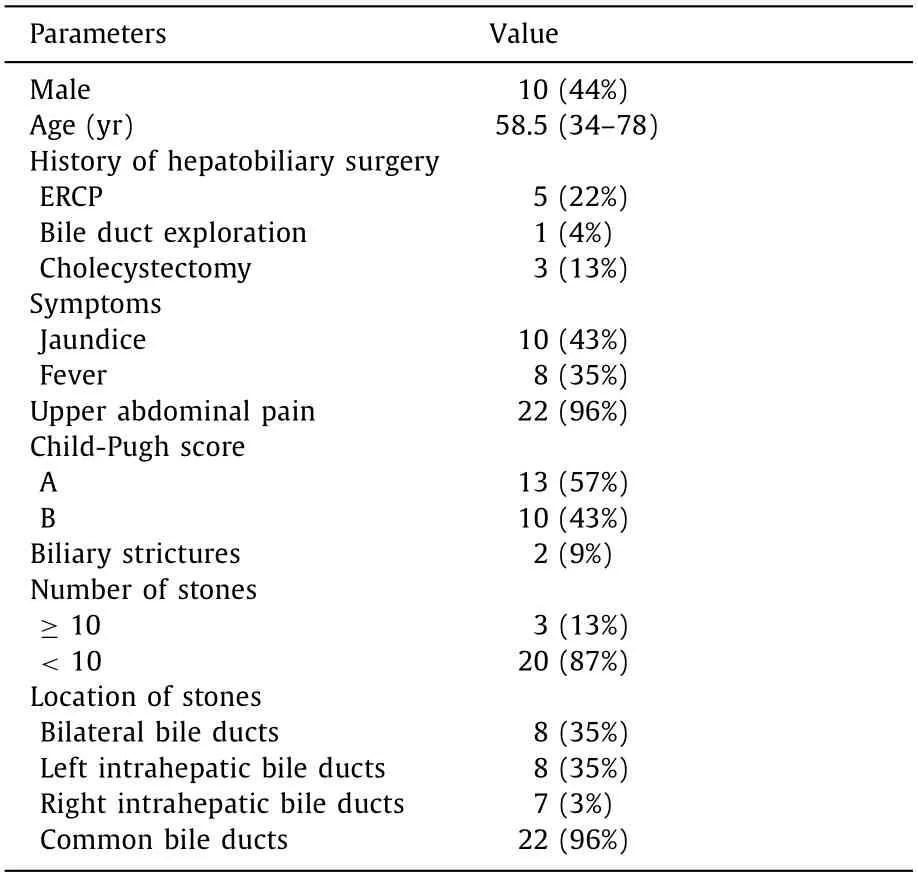
Table 1 Demographic and clinical features of patients (n=23).

Table 2 Treatment results of low-pressure pulse flushing choledochoscope combined with neodymium laser lithotripsy (n=23).
The current common treatment for intrahepatic bile duct stone is surgical incision of the bile duct to remove stones,partial hepatectomy,and intraoperative and postoperative choledochoscopy combined with laser lithotripsy.The application of fiber choledochoscopy has brought hope for resolving high residual stone rate after intrahepatic bile duct stone surgery and high reoperation rate.It has been widely conducted in clinical practice and positive effects have been reported [3,4].Neodymium laser is currently one of the most popular laser lithotripsy techniques.It has the advantages of small trauma,accurate positioning,comprehensive lithotripsy,no damage to normal soft tissues,and hemostasis [5] .
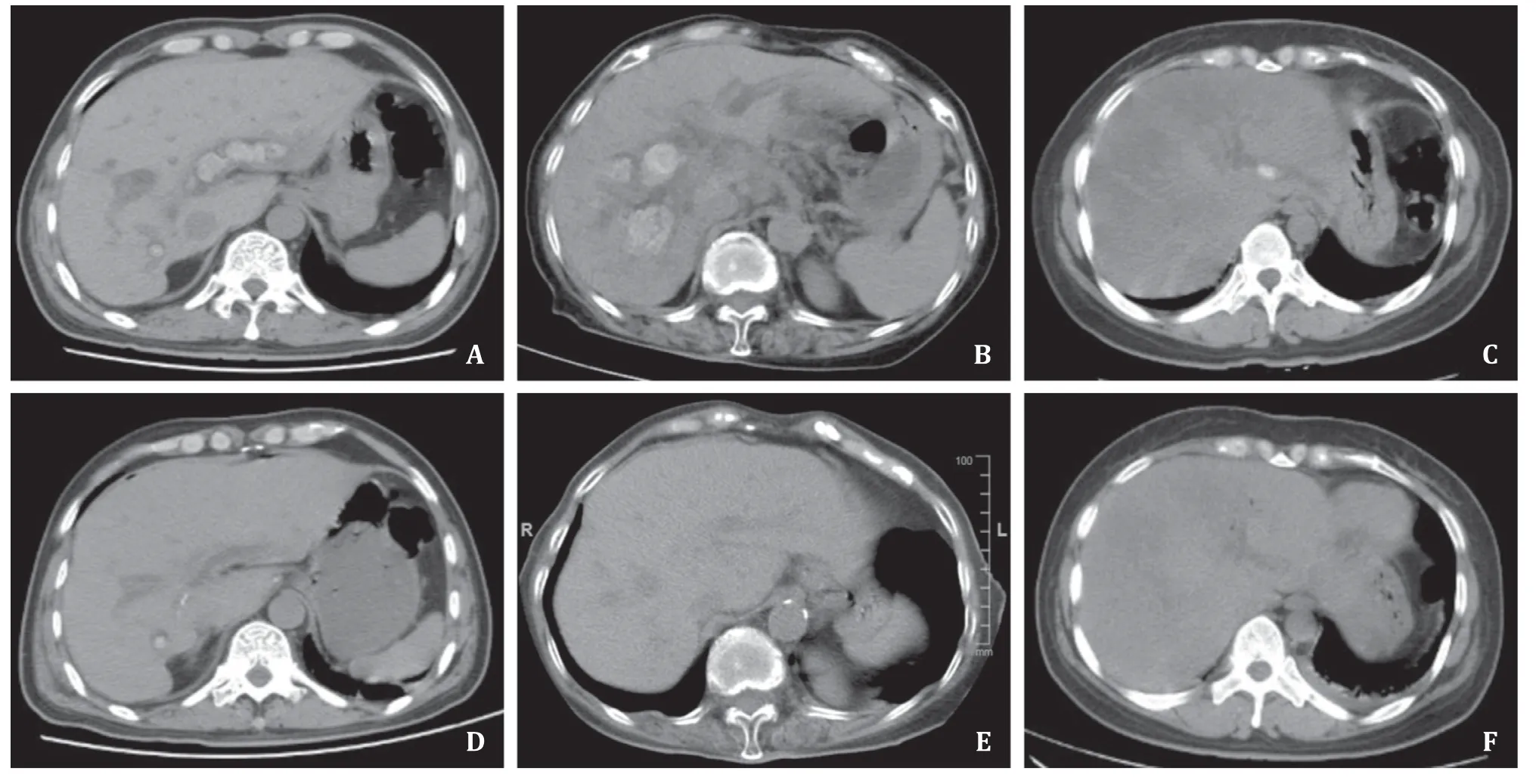
Fig.2.A-C:Abdominal CT showing numerous stones located in the bilateral intrahepatic bile duct before laser lithotripsy.D:Abdominal CT showing right intrahepatic bile duct stones after laser lithotripsy because of bile duct stricture.E -F:Abdominal CT showing no intrahepatic bile duct stones after laser lithotripsy.
Jiang et al.reported that choledochoscope holmium laser lithotripsy combined with partial hepatectomy is a safe and effective method for the treatment of intrahepatic bile duct stones [6] .In laser lithotripsy,the main problem is that during the lithotripsy process,the large number of stone chips and flocs cause unclear vision [7] .This drawback is particularly prominent.Studies [7-9]have shown that the application of a ureteral catheter in the process of ureteral calculi lithotripsy is safe and effective.Moreover,it can shorten the operative time and improve the stone removal rate.
In this study,we applied a ureteral catheter to lithotripsy of intrahepatic bile duct stone to observe its effect.We improved the standard choledochoscopy laser lithotripsy with low-pressure pulse irrigation,and choledochoscopy suction,thereby reducing biliary pressure [10] .The choledochoscope combined with ureteral catheter can be regarded as a dual channel choledochoscope.The key feature of laser lithotripsy under low-pressure pulse flushing of ureteral catheter with choledochoscope is that it allows simultaneous inflow and outflow (inflow through the ureteral catheter,and outflow through the working channel of the choledochoscope).
The F5 ureteral catheter low-pressure pulse flushing choledochoscope combined with a neodymium laser lithotripsy device does not require other special equipment or additional training.We performed choledochoscopy combined with neodymium laser lithotripsy on 23 patients with low-pressure pulse flushing of ureteral catheter.All cases were successfully operated within a reasonable time.
Since this is only our primary experience,we do recognize the limitations of this research.One of the main limitations is the lack of biliary pressure measurement.In addition,there was no blood culture tested after surgery.This study lacked a control group;a randomized study is needed to determine whether choledochoscopy combined with neodymium laser lithotripsy under continuous ureteral catheter irrigation has any benefit over conventional lithotripsy.
In conclusion,we employed a novel simple and efficient way to perform lithotripsy.Our practice indicated that ureteral catheter low-pressure pulse flushing combined with neodymium laser lithotripsy is safe,reliable,convenient and could improve the vision of field and shorten the operative time.
Acknowledgments
None.
CRediTauthorshipcontributionstatement
Wen-LongZhang:Project administration,Writing -original draft.Zhe-PingFang:Methodology,Funding acquisition.Bin-Yao Shi:Validation.TingChen:Data curation.Shang-DongLv:Supervision.ChengWang:Data curation.PengHu:Resources.Fa-Biao Zhang:Supervision,Writing -review &editing.
Funding
This study was supported by grants from the National Natural Science Foundation of China (81872237),the Science Technology Program of Zhejiang Province on the Scientific Research Project (LGF19H160018,LQ18H160028 and LY17H160069),Zhejiang Provincial Health Department Project (2017KY161 and 2015KYB434).
Ethicalapproval
This study was approved by the Ethics Committee of Taizhou Hospital of Zhejiang Province,Wenzhou Medical University.Written informed consent was obtained from all participants.
Competinginterest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Recurrence and survival following microwave,radiofrequency ablation,and hepatic resection of colorectal liver metastases:A systematic review and network meta-analysis
- Mitochondria:A critical hub for hepatic stellate cells activation during chronic liver diseases
- Symptomatic Val122del mutated hereditary transthyretin amyloidosis:Need for early diagnosis and prioritization for heart and liver transplantation
- The growth rate of hepatocellular carcinoma is different with different TNM stages at diagnosis
- Overexpression of anillin is related to poor prognosis in patients with hepatocellular carcinoma
- Micro-positron emission tomography imaging of angiogenesis based on 18 F-RGD for assessing liver metastasis of colorectal cancer