Recurrence and survival following microwave,radiofrequency ablation,and hepatic resection of colorectal liver metastases:A systematic review and network meta-analysis
2021-09-23PshlisGvriilidisKeithRoertsNioldeAngelisLuAldrighettiRoertSutliffe
Pshlis Gvriilidis , ,Keith J Roerts ,Niol de’Angelis ,Lu Aldrighetti ,Roert P Sutliffe
a Department of Hepato-Pancreato-Biliary and Liver Transplant Surgery, Queen Elizabeth University Hospitals Birmingham NHS Foundation Trust, B15 2TH,United Kingdom
b Department of Digestive Surgery, University Hospital Henri Mondor (AP-HP), 94010 Créteil and University of Paris Est, Créteil, France
c Division of Hepatobiliary surgery, San Raffaele Hospital, Via Olgettina 60, Milan 20132, Italy
Keywords:Microwave ablation Radiofrequency ablation Hepatic resection Liver resection
ABSTRACT Background: Gold standard for colorectal liver metastases (CRLM) remains hepatic resection (HR).However,patients with severe comorbidities,unresectable or deep-situated resectable CRLM are candidates for ablation.The aim of the study was to compare recurrence rate and survival benefit of the microwave ablation (MWA),radiofrequency ablation (RFA) and HR by conducting the first network meta-analysis.Data sources: Systematic search of the literature was conducted in the electronic databases.Both updated traditional and network meta-analyses were conducted and the results were compared between them.Results: HR cohort demonstrated significantly less local recurrence rate and better 3-and 5-year diseasefree (DFS) and overall survival (OS) compared to MWA and RFA cohorts.HR cohort included significantly younger patients and with significantly lower preoperative carcinoembryonic antigen (CEA) by 10.28 ng/mL compared to RFA cohort.Subgroup analysis of local recurrence and OS of solitary and ≤3 cm CRLMs did not demonstrate any discrepancies when compared with the whole sample.Conclusions: For resectable CRLM the treatment of choice still remains HR.MWA and RFA can be used as a single or adjunct treatment in patients with unresectable CRLM and/or prohibitive comorbidities.
Introduction
Colorectal cancer is the third most common cancer worldwide.About 25%-30% of patients present with synchronous metastases at the time of diagnosis,and during the course of the disease a further 40% will develop metachronous metastases [1] .The 5-year overall survival (OS) after hepatic resection (HR) is around 40%-50% [1,2].However,from the whole cohort of patients with colorectal liver metastases (CRLM),only about 20% are eligible for upfront HR.Although HR is generally considered the only intervention associated with long-term survival and/or potential for cure,local disease control may be feasible using thermal ablative techniques (microwave,MWA or radiofrequency,RFA) particularly in patients with small,solitary metastases who are not fit for HR [3-6] .
Thermal ablation may also be utilized intraoperatively to target deep metastases in combination with HR in order to preserve hepatic parenchyma,and to reduce the perioperative morbidity compared to major hepatectomy [6-8] .For surgically fit patients with small,solitary liver metastases,it is not known which intervention (HR or thermal ablation) should be considered first-line treatment.Published data are limited to single-centre,retrospective cohort studies and there is currently a lack of randomized data in this field.The colorectal liver metastases (LAVA) trial failed to recruit [9],and the HELARC (trial ID:NCT02886104) and COLLISION trials are currently recruiting patients [10] .The aim of this study was to compare the local recurrence rate and long-term survival in patients undergoing HR,RFA or MWA using a network metaanalysis.
Methods
The PRISMA Statement checklist for reporting a systematic review and meta-analysis was used in this study [11] .
Literature search
Using both free text and MESH terms (microwave,radiofrequency ablation,liver or hepatic resection,colorectal liver metastases or hepatic metastases),Embase,PubMed,Medline,and Google Scholar databases were systematically searched from inception up to September 2020.References of the selected articles were investigated manually for further studies.Any discrepancies between the authors were resolved by dialogue.
Study selection, and inclusion and exclusion criteria
Only studies that compared a) MWA vs.RFA,b) MWA vs.HR and c) RFA vs.HR were included in the review.
Data extraction and outcomes
Two researchers (PG and RPS),independently extracted the following summary data for the included studies:name of authors;country;number of patients included in MWA,RFA and HR;age;sex;primary tumor;tumor size;preoperative carcinoembryonic antigen (CEA);chemotherapy;synchronous metastases;node positive primary;tumor number at time of ablation more than one;follow-up;hepatic recurrence;1-,2-,3-year disease-free survival(DFS);and OS.
Sensitivity analysis
Analyses of both the primary and secondary outcomes were performed using fixed-and random-effects models to assess the impact of heterogeneity on the conclusions.Subgroup analysis of the local and systemic recurrences was performed.
Definitions
Local recurrence was considered any recurrence in the Couinaud segment treated or at the margin of resection.Systemic recurrence or distant metastasis was defined as any metastasis outside of the Couinaud segment treated.DFS was considered the time after intervention during which no sign of tumor was found.OS was referred to the fact that the patient had not died from any cause.Peribiliary tumors were considered those situated ≤5 mm to the common hepatic duct,main right,or left hepatic duct.Perivascular tumors were considered those situated ≤5 mm from a vessel at least 4 mm in diameter.
Statistical analysis
The Newcastle-Ottawa scale (NOS) was used to evaluate the methodological quality of all included studies [12] .Studies scoring≥7 were considered high quality.
Analysis of the results was conducted using methodologies described in our previous publications [13,14].
First,a pairwise meta-analysis was conducted for studies that compared two of the treatment approaches.Subsequently,a network meta-analysis was conducted to compare MWA,RFA,and HR.Statistical analysis was performed using both the Review Manager 5.3 software (Cochrane Collaboration,Oxford,England),and General mixed treatments comparisons (GeMTC) software [15,16].Dichotomous variables were assessed based on odds ratios (ORs)with 95% confidence intervals (CIs).
The method described by Parmar et al.was used to estimate the long-term survival,where possible [17] .For studies that did not report the means and variances of the two groups,these values were estimated from the median,range and sample size,using the technique described by Hozo et al.[18],where possible.
For all analyses,the point estimate was considered significant atP<0.05.
Results
Search strategy and study characteristics
Twenty-six studies,which included 3401 patients,were selected from the pool of 527 studies [19-44] (Fig.1).This MWA cohort included 350 (10%) patients,RFA 1253 (37%) and HR cohort 1798 (53%) patients.Furthermore,there were three studies comparing MWA vs.RFA consisting of 385 patients [19-21] ;five studies comparing MWA vs.HR consisting of 449 patients [22-26] ;and 18 studies comparing RFA vs.HR consisting of 2567 patients [27-44] (Table 1).Twenty-two studies (85%) scored more than 7 and were characterized as high quality (Table 1).
Results of pairwise meta-analysis
MWAvs.RFA
More patients with MWA had chemotherapy compared to the RFA cohort (OR=2.79;95% CI:1.25,6.22;P=0.01;I2=81%)(Table 2).
Demographic parameters demonstrated nonsignificant differences between the two cohorts.Furthermore,tumor size,lymph nodes positive primary,vasculo-biliary proximity,clinical risk score and hepatic recurrences demonstrated nonsignificant differences between the MWA and RFA cohorts (Table 2).
MWAvs.HR
Patients with MWA had significantly fewer synchronous metastases compared with the HR cohort (29% vs.51%;OR=0.49;95%CI:0.29,0.85;P=0.01;I2=0%) (Table 2).
Sex,tumor size,pre-intervention CEA,major morbidity,multiple metastases,and hepatic recurrences demonstrated nonsignificant differences between the MWA and HR cohorts.Furthermore,3-,5-year DFS and OS demonstrated nonsignificant differences between the MWA and HR cohorts (Table 2).
RFAvs.HR
Patients with RFA were significantly older (MD=1.41;95% CI:0.31,2.51;P=0.01;I2=63%) and more males compared to the HR cohort (OR=1.54;95% CI:1.27,1.87;P<0.001;I2=2%).
Parameters of the synchronous metastases,lymph nodes positive primary,tumor number at time of ablation>1,and tumor size demonstrated nonsignificant differences between the RFA and HR cohorts.
The recurrences were significantly less in the HR cohort compared to the RFA cohort.
In addition,there was evidence that 3-,5-year DFS and OS were significantly higher in the HR cohort compared to the RFA cohort(Table 2).
Results of network meta-analysis
Age,tumor size,primary tumor,synchronous metastases,lymph node positive primary and preoperative CEA demonstrated nonsignificant differences between the three interventions (Table S1).
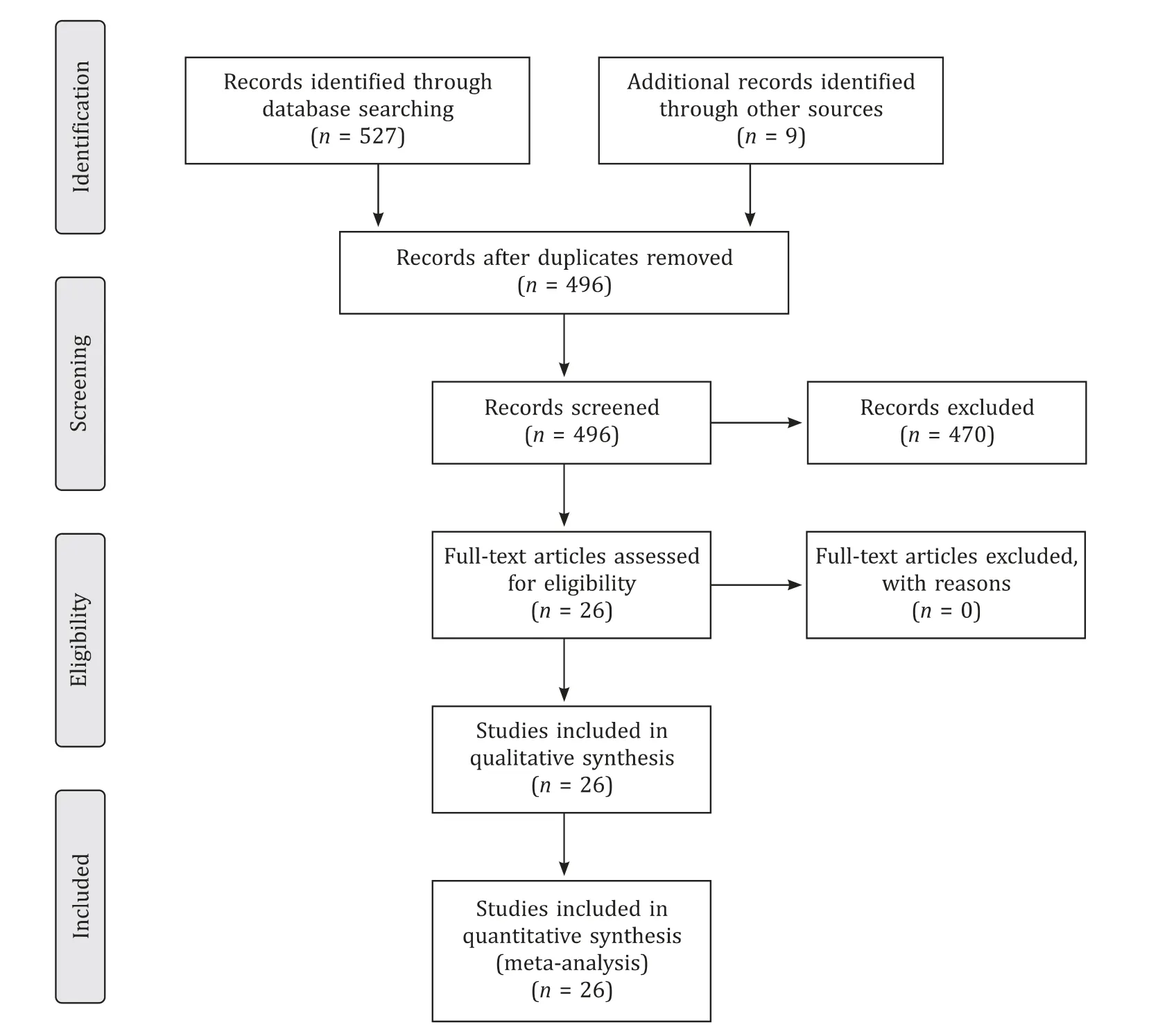
Fig.1.Diagram of the search strategy.
The HR cohort demonstrated significantly fewer hepatic recurrences and higher 3-,and 5-year DFS and OS when compared with the RFA cohort.On the other hand,there were nonsignificant differences between the HR cohort and the MWA cohort.Furthermore,nonsignificant differences were demonstrated in DFS and OS between the MWA and RFA cohorts (Table S1).
Sensitivity analysis
There was no evidence of any major discrepancies between fixed-and random-effects model results.In pairwise meta-analysis,age,sex,and preoperative CEA demonstrated marginally significant differences;whereas in network meta-analysis these differences disappeared.The statistically significant differences of hepatic recurrences and 3-and 5-year DFS and OS in favor of HR compared to RFA were further confirmed by network meta-analysis (Table 2,Table S1).
Subgroup analysis demonstrated that local recurrence rate was significantly higher in the RFA cohort compared to that of the HR cohort (39% vs.6%;OR=7.54;95% CI:4.72,12.05;P<0.001;I2=46%).Furthermore,the HR cohort demonstrated significantly fewer distant recurrences compared to the RFA cohort (34% vs.50%).However,there was evidence of discrepancy of the statistical significance between fixed-effects and random-effects model.Under fixed-effects model the result was statistically significant,whereas under random-effects model it became nonsignificant.
Further analysis with funnel plot detected two outliers namely the studies by Park et al.[38] and Lee et al.[39] which demonstrated the smaller effect in favor of the RFA cohort (Table 2,Fig.2).
Furthermore,subgroup analysis of the local recurrence rate and OS of the groups including solitary CRLM and CRLM ≤3 cm did not demonstrate any discrepancies when compared with the whole sample (Table 2).Of note,the above results should be interpreted cautiously,because the sample size of local recurrence and 5-year OS included 556 and 585 patients,respectively.Therefore,underpowered sample size might have influenced the results.

Discussion
The evidence of this network meta-analysis demonstrates that recurrence rate,3-and 5-year DFS and OS were significantly better in the HR cohort compared to those in the RFA cohort.Furthermore,the HR cohort included significantly younger patients and the preoperative CEA was significantly lower by 10.28 ng/mL compared to the RFA cohort.Of note,in the sensitivity analysis,the outcome of distant recurrences demonstrated discrepancy between the fixed-and random-effects models.Further subgroup analysis detected outliers studies by Park et al.[38] and Lee et al.[39] .Common characteristic of both studies was the underpowered sample size of the RFA cohort compared to that of the HR cohort.Moreover,there were high heterogeneity and variety of the definitions.Therefore,the above bias might have influenced the result to become nonsignificant in the random-effects model.On the other hand,the results of the 3-and 5-year OS demonstrated 0% heterogeneity and no discrepancies detected between the fixed-and random-effects models (Table 2).
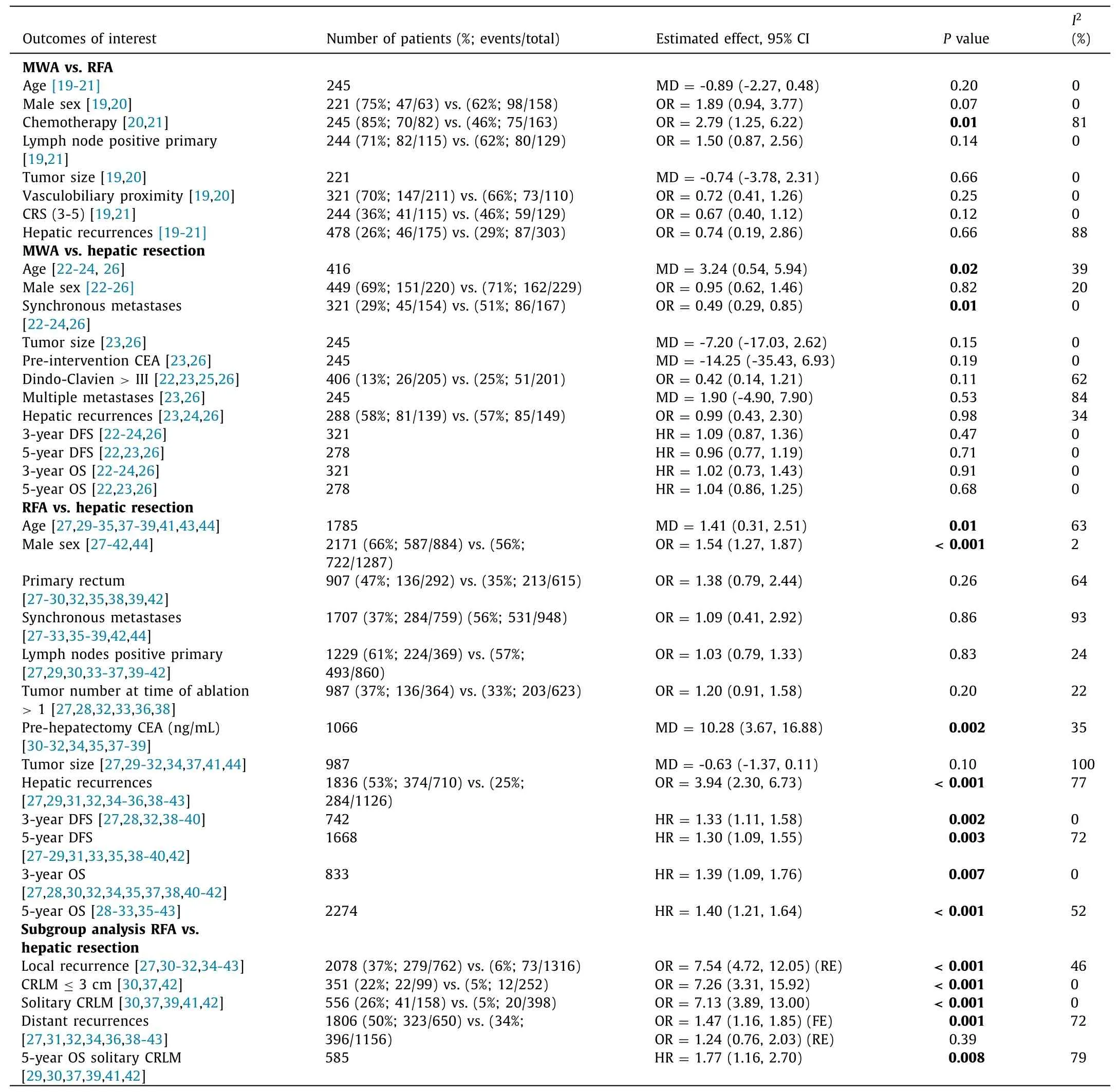
Table 2 Outcomes of interest:MWA vs.RFA vs.HR.
It has been reported that complete destruction occurred with MWA ofexvivohuman livers and CRLM [45] .In the present study,nonsignificant differences were detected in intrahepatic recurrence rate between the MWA and HR cohorts and MWA and RFA cohorts as well;the result produced by three studies consisting of 288 and 478 patients,respectively,and the heterogeneity between the studies was 34% for the MWA vs.HR and 88% for the MWA vs.RFA,respectively.Furthermore,there was no upfront comparison of the MWA approach to the HR only.In the three studies,the HR cohort included patients who have been treated with both HR and MWA.In particular,the study by Philips et al.[23] included CRLM in MWA,HR and combined resection cohorts (50%,59% and 64%,respectively).The rest of the patients were diagnosed with hepatocellular carcinoma (HCC) and other metastases.Therefore,the above results should be interpreted very cautiously,because high heterogeneity between and within the studies,and underpowered sample size might have influenced the results.
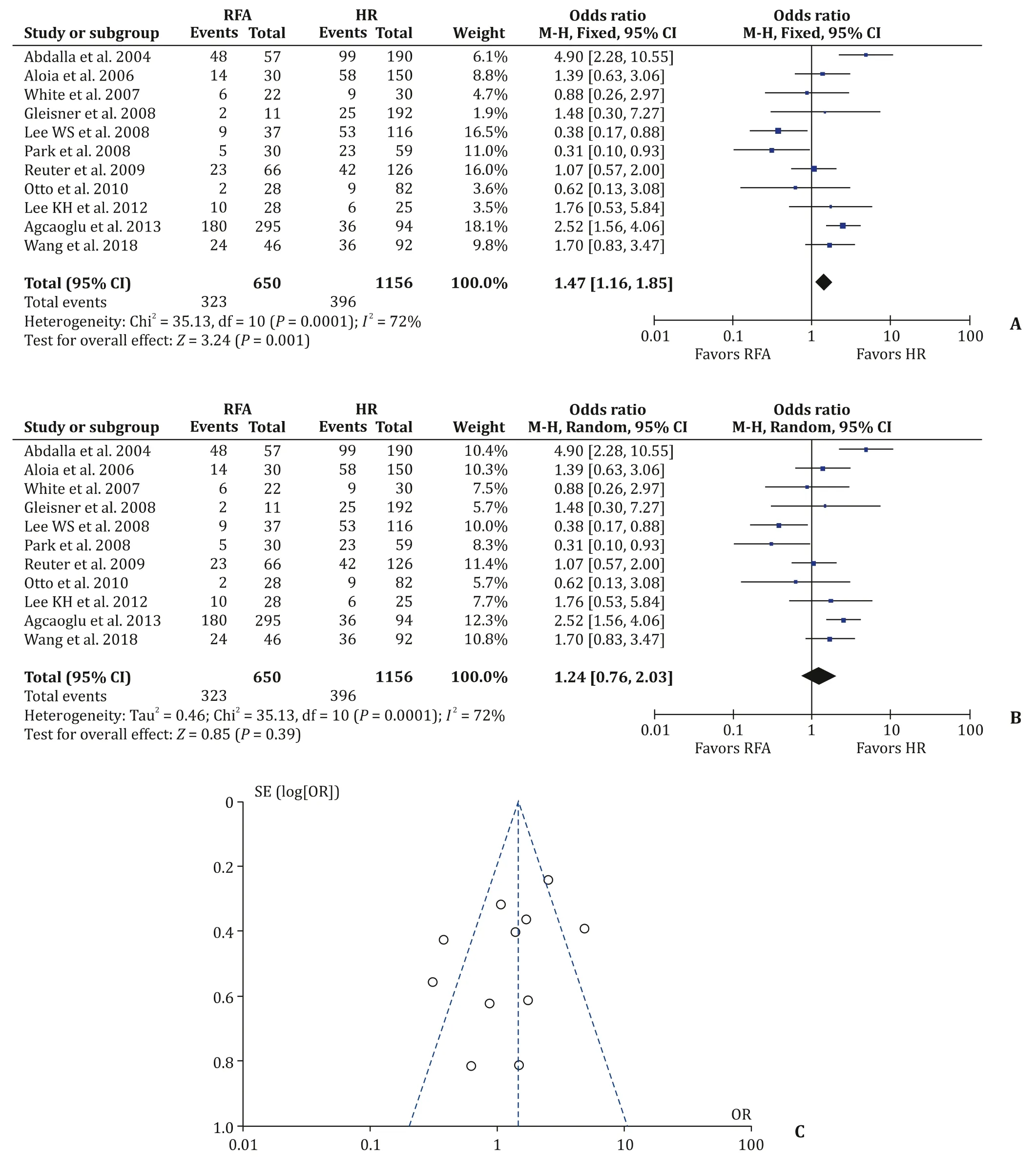
Fig.2.Distant recurrences.A:Fixed-effects model;B:random-effects model;C:funnel plot.
Of note,subgroup analysis of the CRLM ≤3 cm and solitary metastasis demonstrated that HR had significantly reduced local recurrences (5%) compared to RFA cohort (22% and 26%,respectively).In addition,5-year OS was significantly better for the HR cohort compared to the RFA cohort.The above results demonstrate that even for solitary and small metastases HR is the gold standard treatment.Moreover,these findings further support the recommendations of the guidelines of the American Society of Clinical Oncology which recommends that resection should remain the gold standard treatment for resectable disease [46] .However,we would like to underline that the results were produced with small sample sizes.In particular,the group of CRLM ≤3 cm consisted of 351 patients and those of solitary CRLM of 456 patients(Table 2).Furthermore,from the included studies 33% of the RFA procedures were performed by radiologists and 11% by surgeons.There were no data about the experience of the radiologists.In addition,a meta-analysis reported that percutaneous approach is an independent risk factor for increased local recurrences in RFA [47] .Therefore,underpowered sample,learning curve and selection bias might have influenced the results.
In nutshell this network meta-analysis demonstrates that HR has significantly less recurrence rate and consequently,significantly better 3-and 5-year DFS and OS.However,the results of the present study should be interpreted in the context of its limitations.In particular,the included studies were retrospective studies conducted in single center with varied definitions and follow-up.Obviously,the RFA patients represented cases with prohibitive comorbidities and with different oncological profile;in particular,the present study demonstrated that the preoperative CEA was lower in the HR cohort compared to that in the RFA cohort.In addition,the HR cohort included significantly younger patients compared to the RFA cohort.Therefore,institutional,national,selection,varied follow-up and learning curve bias might have influenced the results.
In 2012,it has been reported that stereotactic RFA with multiple probes achieved 97% local control rates in CRLM>5 cm [48] .Moreover,promising results of the stereotactic RFA were reported for CRLM up to 13 cm situated in unfavorable positions [49] .However,there are no studies to compare directly the stereotactic RFA with the HR in order to evaluate the superiority of the one approach over the other.So far,there are no completed randomized controlled trials to compare HR with the ablative approaches.The HELARC trial comparing HR to ablative approaches in patients with resectable synchronous CRLM will be completed in 2026.The surgical community also eagerly anticipates the results of the COLLISION trial which compares resectable and ablatable CRLM less than 3 cm.
In conclusion,this network meta-analysis demonstrates that HR remains the gold standard treatment for CRLM.MWA and RFA can be used as an adjunct or single treatment in adequately selected patients and can be a useful alternative treatment for patients with prohibitive comorbidities.
Acknowledgments
None.
CRediTauthorshipcontributionstatement
PaschalisGavriilidis:Conceptualization,Formal analysis,Investigation,Methodology,Software,Validation,Writing -original draft,Writing -review &editing.KeithJRoberts:Formal analysis,Investigation,Methodology,Validation,Writing -original draft,Writing -review &editing.Nicolade’Angelis:Formal analysis,Investigation,Methodology,Validation,Writing -original draft,Writing -review &editing.LucaAldrighetti:Formal analysis,Investigation,Methodology,Validation,Writing-original draft,Writing -review &editing.RobertPSutcliffe:Formal analysis,Investigation,Methodology,Supervision,Validation,Writing -original draft,Writing -review &editing.
Funding
None.
Ethicalapproval
Not needed.
Competinginterest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Supplementarymaterials
Supplementary material associated with this article can be found,in the online version,at doi:10.1016/j.hbpd.2021.05.004 .
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Mitochondria:A critical hub for hepatic stellate cells activation during chronic liver diseases
- Symptomatic Val122del mutated hereditary transthyretin amyloidosis:Need for early diagnosis and prioritization for heart and liver transplantation
- The growth rate of hepatocellular carcinoma is different with different TNM stages at diagnosis
- Overexpression of anillin is related to poor prognosis in patients with hepatocellular carcinoma
- Micro-positron emission tomography imaging of angiogenesis based on 18 F-RGD for assessing liver metastasis of colorectal cancer
- Fisetin mitigates hepatic ischemia-reperfusion injury by regulating GSK3 β/AMPK/NLRP3 inflammasome pathway