Complications of common bile duct stones:A risk factors analysis
2021-09-23DongJunOhJiHyungNamDongKeeJangJunKyuLee
Dong Jun Oh,Ji Hyung Nam,Dong Kee Jang,Jun Kyu Lee
Department of Internal Medicine, Dongguk University Ilsan Hospital, Goyang 10326, Korea
Keywords:Common bile duct stone Risk factors Obstructive jaundice Pancreatitis Cholangitis
ABSTRACT Background: The latest guidelines recommended that common bile duct stones (CBDSs) should be removed,preferably endoscopically,regardless of the presence of symptoms or complications.However,the removal of CBDSs may not be feasible in very old patients or those with co-morbidities.In these cases,it is important to understand the risk factors for the development of CBDSs-related complications to decide whether or not to treat high-risk patients.Herein,we aimed to identify the risk factors for the development of complications after the diagnosis of CBDSs.Methods: The medical records of patients with CBDSs between October 2005 and September 2019 were retrospectively analyzed.All patients with radiologically-diagnosed CBDSs,including those who received treatment and those who did not,were analyzed.Results: A total of 634 patients were included and 95 (15.0%) patients had CBDS-related complications during the mean follow-up period of 32.6 months.Forty-four (6.9%) high-risk patients remained asymptomatic and did not receive treatment during the follow-up period.In multivariate analyses,size of CBDSs≥5 mm and no treatment within 30 days were independent risk factors for the development of complications.The spontaneous passage of CBDSs was proved radiologically in 9 out of 81 (11.1%) patients within 30 days.Conclusions: It is recommended treating CBDSs within 30 days from the diagnosis,even in high-risk patients,especially if the size is larger than 5 mm.
Introduction
The latest guidelines recommend that common bile duct stones(CBDSs) should be removed,preferably by endoscopic retrograde cholangiopancreatography (ERCP),regardless of the presence of symptoms or complications [1-4] .However,ERCP-related adverse events (AEs),such as perforation,bleeding,infection,post-ERCP pancreatitis,and cardiovascular events,occur in about 10% of the patients [5] .Moreover,the performance of ERCP may be unfeasible in very old patients or those with co-morbidities [6] .Although percutaneous approach or surgery may be considered as alternative,severe complications including hemobilia by percutaneous transhepatic cholangioscopy were reported in about 8% of the patients [7] and the overall morbidity from common bile duct exploration was reported to be 3% -20% [8] .
CBDSs have inevitable concerns regarding the development of complications,such as obstructive jaundice,biliary pancreatitis,or acute cholangitis if not treated,which may lead to unfavorable morbidity or even mortality [3] .In this situation,physicians fall into trouble when planning management strategy for high-risk patients with untreated CBDSs.In addition,with the widespread use of radiologic technology with enhanced resolution,CBDSs are also incidentally found during radiologic studies conducted for other medical indications.
Therefore,it is important to clarify the risk factors for CBDSrelated complications to determine whether or not to treat highrisk patients.In this study,we aimed to identify the risk factors for the development of complications after the diagnosis of a CBDS to select high-risk patients for whom the removal of CBDSs should be performed despite the risk of procedure-related AEs.
Methods
Study population
This study was a single-center,retrospective,cohort study conducted at Dongguk University Ilsan Hospital,Korea.From October 2005 to September 2019,patients with clearly-identified CBDSs byimaging modalities such as transabdominal ultrasonography (US),computed tomography (CT),endoscopic ultrasonography (EUS),and magnetic resonance imaging (MRI) were selected and those who did not perform interventional treatment at the time of diagnosis were included.Patients without follow-up or with a follow-up period less than one month after CBDS treatment,no definite CBDS on the imaging modalities,cholangiography by ERCP or percutaneous transhepatic cholangiography,and those referred from other hospitals were excluded from the study.
The following variables were thoroughly reviewed in the electronic medical records:age,sex,social and medical history,American Society of Anesthesiologists (ASA) class,prior abdominal surgery (especially cholecystectomy),the presence of gallbladder stones (GBSs),characteristics of the CBDSs (size,number,accompanied bile duct dilatation),symptoms and complications from the diagnosis to the latest follow-up,and treatment outcomes(Table 1).This study was approved by the Institutional Review Board (DUIH-IRB 2020-03-048).
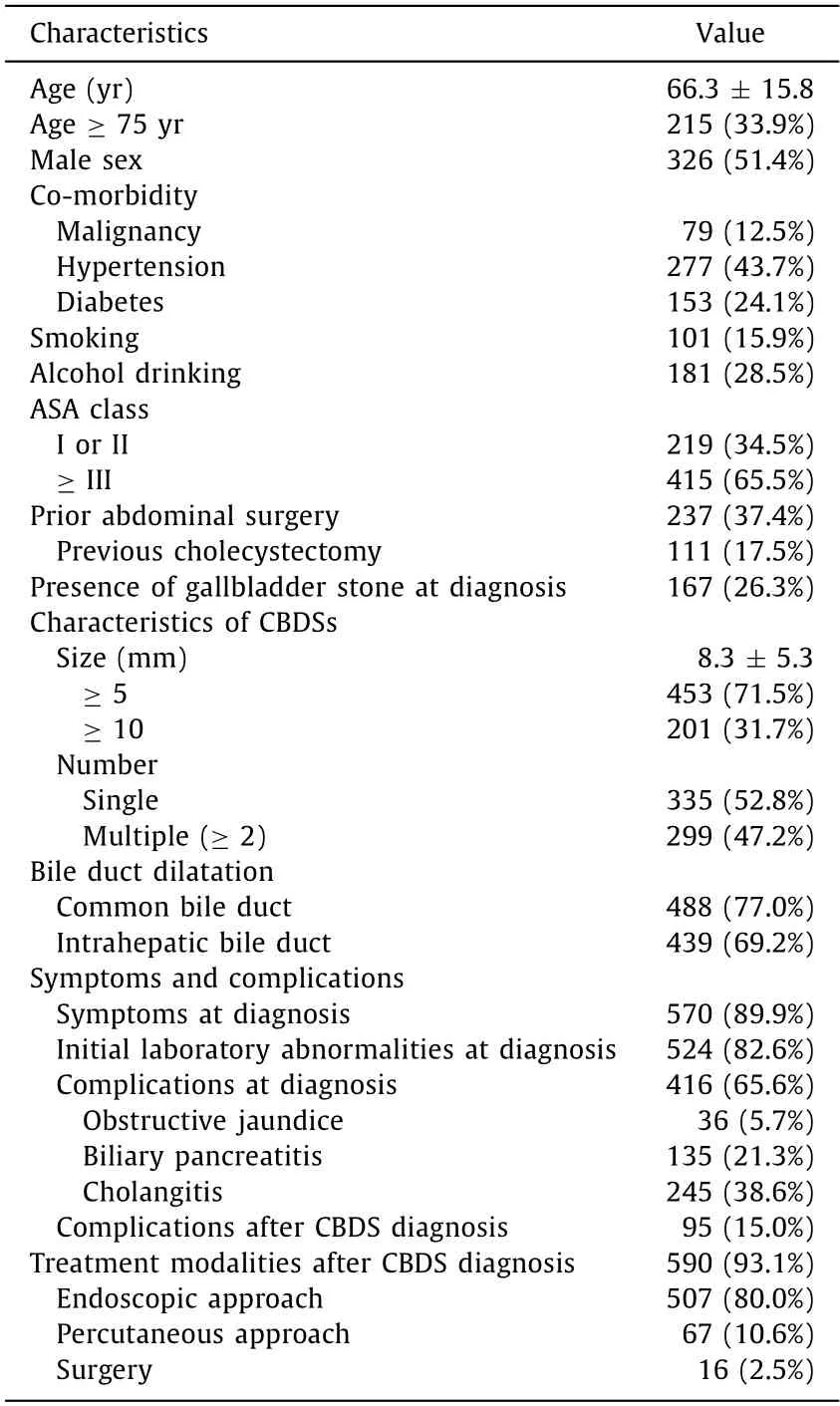
Table 1 Baseline characteristics of patients at the time of diagnosis of common bile duct stones (n=634).
Treatment strategy
A consistent treatment strategy for CBDSs was maintained throughout the study period.All endoscopic,percutaneous,and surgical procedures were performed by experienced endoscopists,interventional radiologists,and surgeons,respectively.The patient’s condition was checked and,if possible,endoscopic treatment was attempted first.After endoscopic sphincterotomy,stone removal was performed with baskets or retrieval balloon catheters with papillary balloon dilatation for huge CBDSs.When complete removal was not possible,pigtail plastic stents were placed for biliary drainage and subsequent attempts for clearance were planned.If the endoscopic treatment failed,percutaneous and/or surgical treatment was performed after the multidisciplinary approach.If an emergent ERCP was not possible in patients with altered anatomy or intubated status or the inability to open the mouth due to neurological sequelae,percutaneous transhepatic biliary drainage (PTBD) was performed first,followed by ERCP.Cholecystectomy was recommended after the removal of CBDSs for patients with GBSs.Patients who could not receive interventional treatment due to high risk or rejected treatment were discharged after providing the appropriate antimicrobial therapy and followed up regularly.Usually,liver function was checked every six months and US or CT was performed annually.
Outcomes
The outcome of interest was risk factors related to the development of complications of CBDSs which were defined as follows:obstructive jaundice evidenced by elevated serum bilirubin levels(>5 mg/dL) without symptoms of biliary colic or cholangitis;biliary pancreatitis observed as abdominal pain associated with increased serum pancreatic enzymes (amylase and lipase) greater than three times the upper limit of normal (ULN);acute cholangitis observed as abdominal pain,jaundice,fever,and/or the confirmation of inflammatory response such as an abnormal serum white blood cell count or increased serum C-reactive protein [9,10].The laboratory abnormalities were determined to be higher than the ULN in at least one of the following markers:total bilirubin,alanine aminotransferase,aspartate aminotransferase,amylase,and lipase.
Statistical analysis
Multiple variables were analyzed by Pearson’s Chi-squared test to analyze the differences in distribution frequency.Continuous variables were analyzed by the Student’st-test.A two-sidedPvalue of<0.05 was considered statistically significant.To assess factors significantly associated with the development of complications of CBDSs,univariate analysis was performed.All binary variables with aPvalue of<0.05 in univariate analysis were analyzed by multivariate logistic regression to test if the risk factors were predictors of complications.Also,logistic regression analysis was used to estimate the odds ratios (ORs).The cumulative hazard associated with complications during the follow-up period was evaluated by the Cox proportional hazards model.
Results
Baseline characteristics
There were 674 patients who met the inclusion criteria during the study period.Forty patients were excluded because they were lost to follow-up and the remaining 634 patients were finally included (Fig.1).The mean age was 66.3 years,and 51.4% were male(Table 1).The mean period from diagnosis to CBDS treatment was 27.9 days.For treatment beyond the mean period,the treatment interval varied from 31 days to 69 months.After the diagnosis of CBDS,590 patients (93.1%) were treated.Among them,553 underwent interventions within 30 days,and 37 underwent intervention after 30 days.
Of the remaining 44 patients (6.9%) who did not receive treatment,the median follow-up period was 19.5 months (range:1-140 months).These patients refused or could not receive the intervention because of serious comorbidities.Among the 44 patients,one developed cholangitis during the follow-up period.She was a 94-year-old female patient in a bed-ridden state who received only conservative treatment and improved finally.

Fig.1.Patient selection and treatment outcomes.CBDSs:common bile duct stones.
Initial treatment modalities after the diagnosis of CBDSs
The 590 patients with CBDSs initially underwent ERCP (507 patients,80.0%),percutaneous approaches such as PTBD (67 patients,10.6%),and surgical removal (16 patients,2.5%).In the group that initially underwent ERCP,15 unstable patients and 8 patients with altered anatomy were converted to the percutaneous approach or surgery.In the group that initially underwent a procedure by the percutaneous approach,5 patients with altered anatomy were converted to the surgery.Ten patients with no or mild symptoms but accompanying altered anatomy and 6 patients with malignancies received surgery.
Risk factors associated with the development of complications after diagnosis of CBDSs
Ninety-five (15.0%) patients experienced complications during the mean follow-up period of 32.6 months (range:2 weeks to 88 months) (Fig.2).In univariate analyses,age ≥75 years,poor health status (ASA class ≥III),no alcoholic history,previous cholecystectomy,CBDS size ≥5 mm,and no treatment within 30 days from the time of diagnosis were associated with the development of complications (allP<0.05) (Table 2).In multivariate logistic regression,CBDS size ≥5 mm (OR=1.827,P=0.045) and no treatment within 30 days (OR=3.115,P=0.001) were independent risk factors for the development of complications.The cumulative risk of complications was significantly higher in the group with no treatment within 30 days compared to that in the group with treatment within 30 days (P=0.025,Fig.3).

Fig.2.Cox proportional hazards model for the cumulative hazard rate of complications after the diagnosis of common bile duct stone.
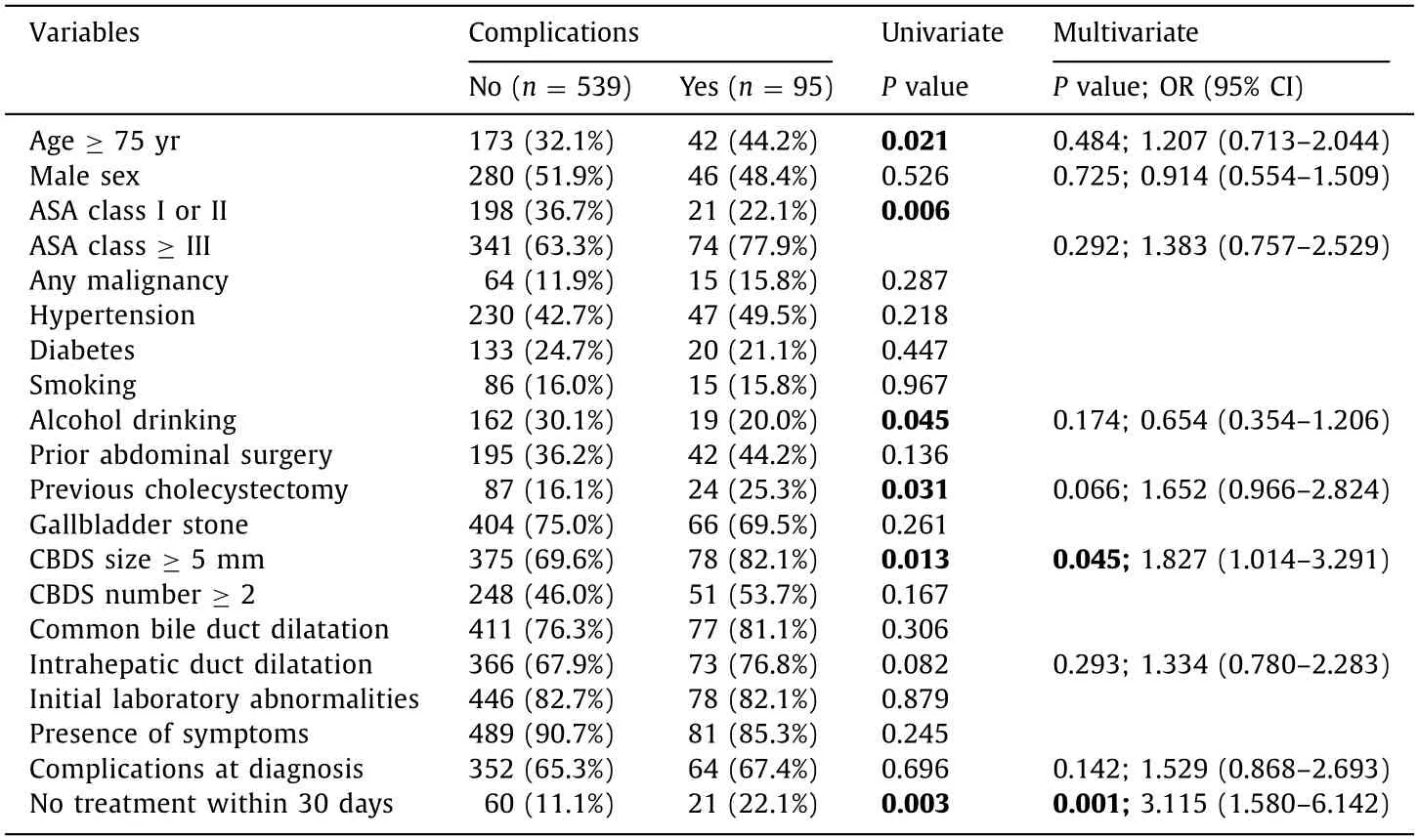
Table 2 Univariate analysis and multiple logistic regression analysis of risk factors predicted to be associated with the development of complications after common bile duct stone diagnosis (n=634).

Fig.3.Cox proportional hazards model for the cumulative hazard rates of complications according to the initial treatment status of common bile duct stones.
Subgroup analysis was performed for 81 patients not treated within 30 days,41 (50.6%) of whom had abdominal pain,and 11(13.6%) had complications at the time of diagnosis (Table 3).The most common reason for no treatment was patient refusal (64.2%),followed by cerebrovascular disorders (11.1%) and anatomical abnormalities (7.4%).During the median follow-up period of 25.0 months in the group of patients not treated within 30 days,21(25.9%) experienced complications.The complication rate after diagnosis of CBDSs was higher in the group not treated within 30 days compared to that of the group treated within 30 days [25.9%(21/81) vs.13.4% (74/553),P=0.003].Spontaneous passage of CBDSs was confirmed in nine (11.1%) patients radiologically.

Table 3 Characteristics of patients with common bile duct stones untreated within 30 days (n=81).
Discussion
Gallstone disease is a common medical condition affecting 10% to 15% of the adult population [11] .Although 1% -4% patients develop symptoms or complications per year,the majority remain asymptomatic [12] .Therefore,prophylactic cholecystectomy for silent GBSs is reserved only for young patients,stone sizes>3 cm,and porcelain gallbladder [13,14].In contrast,CBDSs need special attention because of the poorer prognosis [15],although about 10% of the patients with GBSs have asymptomatic CBDSs [16] .The latest guidelines commonly recommend the removal of CBDSs once the diagnosis is made even in asymptomatic patients [2-4] .However,in real-world practice,patients are encountered not uncommon who have high risks due to very old age or co-morbidities that caution should be used in decisions for invasive versus conservative treatment.For this purpose,understanding the natural course of untreated CBDSs is important,whereas related studies are lacking.
Several guidelines state the timing of treatment according to the severity of cholangitis or biliary pancreatitis [2,3,17,18].However,evidence is still lacking regarding how soon elective treatment should be performed for CBDSs without cholangitis or pancreatitis.Our study identified no treatment within 30 days as an independent risk factor for the development of complications.Therefore,it would be better to treat CBDSs as early as possible.
The rate of spontaneous pass out in our study was relatively lower compared with those reported in other studies [19-21] .The reason might be due to the different diagnostic method.Most CBDSs were evaluated by US and CT in our study,while other studies performed EUS or cholangiography for identifying the spontaneous CBDSs passages.Of course,MRCP and EUS are superior methods for the diagnosis of CBDSs rather than US and CT.However,EUS and MRCP are more invasive and expensive,which are not reimbursed by medical insurance for CBDSs in Korea.
Post-ERCP pancreatitis is prone to develop in patients with asymptomatic CBDSs [22,23],for whom a wait-and-see approach may be planned,especially for high-risk patients.However,among 81 patients with CBDSs not treated within 30 days,21 patients experienced complications.It seems important to plan a prudent strategy balancing the risk of CBDSs complications and procedurerelated AEs.
Our study was limited by the retrospective and uncontrolled design.However,since it may be not ethical to randomize and observe without treatment of CBDSs,a prospective controlled study cannot be performed.Also,because the number of patients who were observed without treatment in this study was insufficient,a large-scale study is needed to clearly identify the natural course of untreated CBDSs.
In conclusion,it is recommended that CBDSs should be removed as early as possible,even in unsuitable patients,especially for those with CBDS sizes of larger than 5 mm.
Acknowledgments
None.
CRediTauthorshipcontributionstatement
DongJunOh:Data curation,Formal analysis,Writing -original draft.JiHyungNam:Formal analysis,Methodology.DongKee Jang:Formal analysis,Methodology.JunKyuLee:Conceptualization,Supervision,Writing -review editing.
Funding
This study was supported by the Dongguk University Research Fund of 2020.
Ethicalapproval
This study was approved by the Institutional Review Board(DUIH-IRB 2020-03-048).
Competinginterest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Recurrence and survival following microwave,radiofrequency ablation,and hepatic resection of colorectal liver metastases:A systematic review and network meta-analysis
- Mitochondria:A critical hub for hepatic stellate cells activation during chronic liver diseases
- Symptomatic Val122del mutated hereditary transthyretin amyloidosis:Need for early diagnosis and prioritization for heart and liver transplantation
- The growth rate of hepatocellular carcinoma is different with different TNM stages at diagnosis
- Overexpression of anillin is related to poor prognosis in patients with hepatocellular carcinoma
- Micro-positron emission tomography imaging of angiogenesis based on 18 F-RGD for assessing liver metastasis of colorectal cancer