Vision loss as the initial presentation during primary pulmonary hypertension treatment
2021-09-14HaiJiangZhangRongHuangLiangLiangFeiZhouPingWuXiangYiChen
Hai-Jiang Zhang, Rong Huang, Liang Liang, Fei Zhou, Ping Wu, Xiang-Yi Chen
1The First College of Clinical Medical Science, China Three Gorges University, Yichang 443002, Hubei Province, China
2Institute of Ophthalmology and Visual Science, China Three Gorges University, Yichang 443002, Hubei Province, China
3Department of Ophthalmology, Yichang Central People’s Hospital, Yichang 443003, Hubei Province, China
4Department of Cardiology, Yichang Central People’s Hospital,Yichang 443003, Hubei Province, China
Dear Editor,
As we all know, pulmonary hypertension is a state of persistent pulmonary artery pressure above 25 mm Hg at rest and greater than 30 mm Hg during exercise. Based on the mechanism or underlying etiology, pulmonary hypertension was classified as primary with no identifiable cause or secondary because of increased pressure in the pulmonary venous or pulmonary capillary system[1]. Continues pulmonary hypertension not only influences other organs such as liver engorgement, edema of the extremities, exertional dyspnea,etc[2], but also can lead to ocular complications including ciliary, choroid, retinal detachment, central retinal vein occlusion, secondary glaucoma, transient myopia,etc[3].These ocular abnormalities occur as a result of elevated venous pressure in the superior vena initially and followed with increases of ophthalmic veins pressure. Here we firstly report a case who complained vision loss bilaterally as the initial presentation during primary pulmonary hypertension(PPH) treatment by sildenafil, and these pathological features reversed spontaneously through adjusting medicine timely.
Ethical ApprovalThis study complied with the tenets of the Declaration of Helsinki. Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
CASE REPORT
A 60-year-old female visited the Department of Ophthalmology,Yichang Central People’s Hospital (Yichang, China) on January 2, 2019, complained distorted and blurred vision in both eyes for 3d. According to her medical history, she was diagnosed as PPH over 5y, and has taken sildenafil (Viagra)orally 50 mg daily, as well as oral administration of warfarin for anticoagulation, but she had no ophthalmological history including laser, surgery, and trauma.
The comprehensive ophthalmic examination was addressed including visual acuity (VA) and the best-corrected visual acuity (BCVA), intraocular pressure (IOP), axial length(Zeiss IOL-Master 500) and anterior-chamber central depth[Ultrasound biological microscope (UBM), Tianjin Maida,China] measured. These parameters are shown in Table 1.Beyond those, slit-lamp biomicroscopic examination exhibited dilated conjunctiva and episcleral vessels, especially in nasal and temporal area of both eyes (Figure 1). And the corneal,pupils, lens transparency, and vitreous body were normal,but narrow anterior periphery chamber is found in both eyes(Topocon, Japan). The ocular fundus showed that macular light reflection wasn’t clear and slightly retinal folding in both eyes (Canon, Japan; Figure 2). In addition, optical coherence tomography (OCT; Heidelberger, Germany)showed the macular were cystoids edema and neuroepithelial detachment in both eyes (Figure 3A). UBM examination on both eyes exhibited narrow anterior periphery chamber and the 360-degree annular ciliochoroidal detachment (Figure 4A). B-Scan (Tianjin Maida, China) was showed chorioretinal detachment due to effusion on bilateral eyes (Figure 5A).
After case discussion and intra-hospital consultation,our cardiologist gave further examination and treatment.Echocardiography revealed a systolic pulmonary arterial pressure of 80 mm Hg, then she was given novel treatment with anlishentan (5 mg, daily) and tadalafil (Cialis, 20 mg, daily)orally to reduce pulmonary artery pressure. At the same time,we treated by timolol (twice a day) and brinzolamide (Azopt,three times a day) to control IOP. After one month of treatment,VA and BCVA were gradually improved, the anterior-chamber central depth was deepen, IOP were decreased and maintained by timolol alone (Table 1). The ocular fundus was returned to normal in both eyes. In particular, macular OCT revealed that subretinal nerve epithelium fluid of both eyes had absorbed(Figure 3B). UBM showed that annular, long, dark liquid area of the ciliary body had disappeared, and choroidal detachment had reset (Figure 4B). B-Scan also revealed that chorioretinal detachment had disappeared on bilateral eyes (Figure 5B).However, the dilated conjunctiva and scleral vessels didn’t get any improvement. With 20mo follow-up, these signs haven’t change remarkably.
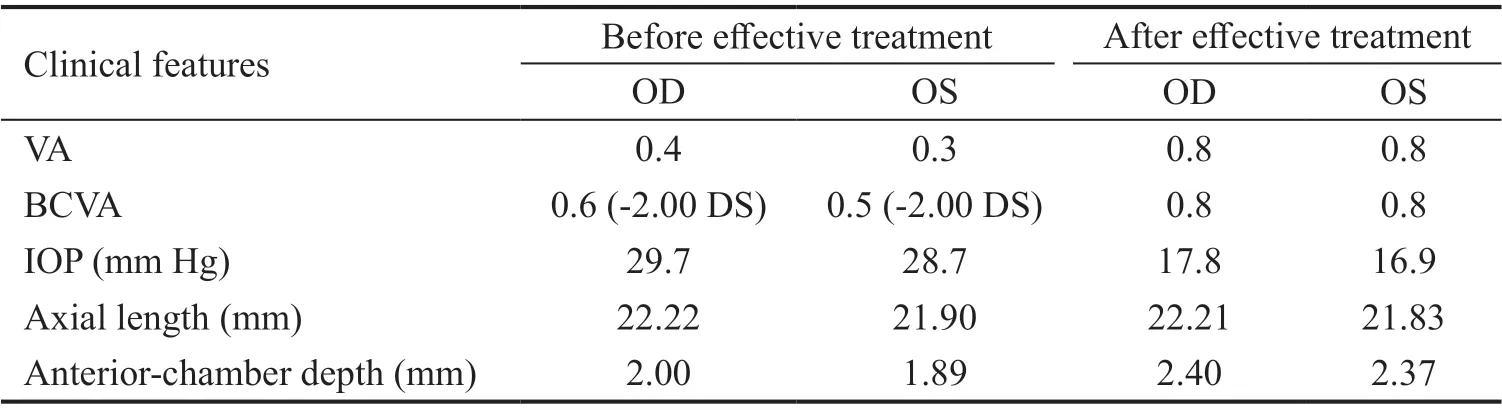
Table 1 The clinical features of this patient

Figure 1 Anterior segment photograph Conjunctiva and scleral vasodilation (arrow).
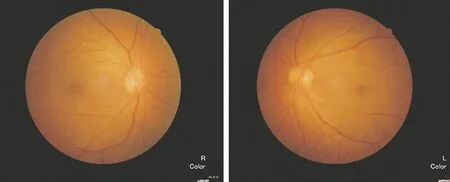
Figure 2 Fundus photograph The macular light reflection weren’t clear and slightly retinal folding in both eyes.

Figure 3 Macular OCT before and after effective treatment A: Macular edema and neuroepithelial detachment in both eyes(asterisk); B: The subretinal fluid of macular region had absorbed.

Figure 4 UBM photograph before and after effective treatment A: The 360-degree full-circumference ciliary body cavity of bilateral eyes has a long and narrow liquid dark area, with a strong echogenic spot, suggesting ciliochoroidal detachment (asterisk);B: The liquid area of the ciliary body has disappeared on the peripheral right eyeball, and the cilichoroidal detachment has reset(asterisk).

Figure 5 B-Scan photograph before and after effective treatment A: Chorioretinal detachment due to effusion was shown on bilateral eyes (meniscus liquid chamber, asterisk); B: Chorioretinal detachment had disappeared on bilateral eyes.
DISCUSSION
PPH is a rare but fatal medical condition that leads to right heart failure by idiopathic occlusion of the pulmonary arteries.Although the etiology and pathogenesis has yet to be precisely elucidated, it may decrease superior vena cava backflow. PPH,if left untreated or poor controlled, may result in reducing venous blood backflow from the eye. These are responsible for elevated venous pressure in the ophthalmic veins, and lead to congestion of the episcleral, retinal and choroidal circulation.Patients always complained some nonspecific ophthalmological symptoms including decreased vision, red eyes or pain caused by high IOP. Although some ocular complications of PPH have reported, the most characteristic features are uveal exudation syndrome and secondary glaucoma, which would affect the visual function and sometime lead to blindness[4].
Different form idiopathic uveal exudation syndrome which was characterized by small eyes, short axial and thick sclera, PPH developed ciliochoroidal exudation because of abnormally dilated choroidal vessels, occlusion of choroidal precapillary arterioles, and obstruction of blood flow within the choriocapillaris[5]. In the same time, IOP was always elevated because of two aspects. On the one hand, raised episcleral venous pressure prevents the aqueous humor outflow from the anterior chamber to trabecular meshwork.On the other hand, suprachoroidal effusiont may bring about the pronation of ciliary body. The forward rotation of the lensiris diaphragm made the anterior chamber shallower, with like angle closure changes not associated with pupillary block and a secondary increase in IOP[6]. Of course, patients may also develop neovascular glaucoma as a complication of retinal neovascularization, which was caused by increased systemic venous pressure[7].
With regard to this patient, the cause of both eyes vision loss due to anterior chamber shallower and transient myopia,macular edema and neuroepithelial detachment, ciliochoroidal leakage[8]. One line of evidence supporting the connection is that after adjusting the kinds and doses of medicine,the refractive inappropriate (-2.00 DS) were disappeared,the anterior chamber central depth became deeper form 2.0 to 2.4 mm (OD), 1.89 to 2.37 mm (OS) respectively,the chorioretinal detachment had reset, and the macular subneuroepithelium fluid began to absorb. In a word, VA and BCVA on bilateral eyes were gradually improved by successful control pulmonary hypertension.
In general, patients with PPH should be taught careful selfobservation of visual function, if their vision worsened, they should immediately contact an ophthalmologist. Periodical ocular examination is helpful to comprehend the pressure of pulmonary artery from the side. If incipient symptoms were detected timely and more effective approaches were given,VA would restored and ocular disorders were spontaneously reversed. So it’s remarkable that the favorable multidisciplinary cooperation is very necessary.
ACKNOWLEDGEMENTS
Conflicts of Interest: Zhang HJ,None;Huang R,None;Liang L,None;Zhou F,None;Wu P,None;Chen XY,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Five-year results of refractive outcomes and visionrelated quality of life after SMlLE for the correction of high myopia
- Role of glycolysis in retinal vascular endothelium, glia,pigment epithelium, and photoreceptor cells and as therapeutic targets for related retinal diseases
- Predictive value of retinal function by the Purkinje test in patients scheduled for cataract surgery in Kinshasa, DR Congo
- Simultaneous pars plana vitrectomy, panretinal photocoagulation, cryotherapy, and Ahmed valve implantation for neovascular glaucoma
- Displacement of the retina after idiopathic macular hole surgery with different internal limiting membrane peeling patterns
- Analogs of microgravity: the function of Schlemm’s canal, intraocular pressure and autonomic nervous during the head-down tilt test in healthy subjects
