Predictive value of retinal function by the Purkinje test in patients scheduled for cataract surgery in Kinshasa, DR Congo
2021-09-14SergeDinkuluNgoyJanvierKilangalangaEdithMukwansekeLongoFlavienLuteteAdrianHopkinsRudolfFriedrichGuthoffThomasStahnke
Serge Dinkulu, Ngoy Janvier Kilangalanga, Edith Mukwanseke, Longo Flavien Lutete,Adrian Hopkins, Rudolf Friedrich Guthoff , Thomas Stahnke
1Eye Department, Saint Joseph Hospital, Kinshasa P. O. 322,DR Congo
2Programme National de Santé Oculaire et Vision (PNSOV),Kinshasa P. O. 322, DR Congo
3Department of Ophthalmology, Rostock University Medical Center, Rostock 18057, Germany
Abstract
● KEYWORDS: Purkinje test; entoptic phenomena;cataract; retinal function; sub-Saharan Africa
INTRODUCTION
Indications for surgery in industrialized countries have changed dramatically over the last 50y. Instead asking whether a patient is still able to read and to fulfill his daily duties, considerations like visual performance for driving at night or increased glare in sunshine are sufficient to justify cataract surgery.
The surgery itself is regarded as a standard 10-minute office procedure with a minimal risk and nearly instant visual recovery which has led to cataract surgical rates increasing from 100 up to 11 000 per million inhabitants per year[1-2]. In most of these patients, the fairly limited lens opacification allows sufficient view of the fundus to estimate post-operative visual performance after the surgery. If trans-pupillary assessment of the retina is not possible, as in many sub-Saharan African cataract patients the evaluation of alternative methods is of importance. The poor results after surgery for whatever reason would not only be a disappointment for the patient, but also involve an unjustified investment of time and financial resources in view of the scarce surgical capacity.
In this pilot study the Purkinje tree optic phenomenon, which was used until the 1950’s as a prognostic test before cataract surgery in Europe, was investigated to evaluate its possible use in low income settings where other modalities, such as B-scan ultrasound, were not freely available. Even where the possibility of a preoperative ophthalmologic examination with B-scan ultrasound exists, there are patients with severe dystrophy or age-related macular degeneration (AMD) without marked thickening of the posterior coats. They would most likely not be detectable with B-scan ultrasound. In these cases the Purkinje entopic test might be helpful to prevent unnecessary cataract surgery.
The Purkinje tree entoptic tests can be used for the visualization of the retinal blood vessels in the posterior pole of the eye. Under ordinary circumstances, the shadows cast by the retinal vessels are not imposed on consciousness.Purkinje (1819)[3]however noted that light projected into the eye through the sclera at a particular angle, would produce shadows of these vessels on a different set of retinal receptors,and produce a retinal image of these vessels in an entoptic manner[3-4]. The light source must also be moved to prevent fading of the observed image[5]. In this way, the vessels can be perceived in the form of an enlarged image forming a complex and branched vascular tree called the “Purkinje tree”[3-9]. If the subject/patient recognizes disturbances in the pattern of the Purkinje tree or if it is not recognized at all, this indicates potential pathological damage such as retinal detachment,retinal vascular occlusion, or tapetoretinal degeneration[10].If the subject/patient notices completely vascular-free areas within the vascular pattern, apart from the center of the Purkinje tree, this would indicate the presence of a scotoma[10].This provides a simple method to evaluate visual performance even in patients with media opacities[10-11].
The method was further developed by paying attention to the so-called macular granular pattern first described by Müller in 1842[12]. This extra extension of the test is both more demanding for the patient and for the examiner[13].
Our aim was to reevaluate this method in sub-Saharan surroundings in investigate if its use preoperatively would be a reliable indication of the postoperative vision after cataract surgery. During the planning phase we found out that the Purkinje tree entoptic phenomenon was quite easy to trigger in healthy volunteers, but the perception (recognition) of the macular granular pattern was much more demanding. As a result, in this pilot study we focused on the Purkinje tree test to determine whether it is justified to promote this phenomenon as a simple and inexpensive technique for the management of cataract patients in our settings.
SUBJECTS AND METHODS
Ethical ApprovalThe study complied with local laws and the principles of the Declaration of Helsinki. Ethical approval was obtained from the Archidiocese de Kinshasa, Comité Scientifique, Saint Joseph’s Hospital. A consent form was presented, explained to patients, and their signature was required. Patients could stop participating in the study at any time without giving reasons.

Figure 1 Patient during the Purkinje entoptic test A: Penlight used; B: Light source on the eyelid in the upper outer quadrant during the examination. Note the halo around the penlight, which appears red through the tissue of the upper eyelid.
Figure 2 Representation of his own vascular patterns, drawn by the discoverer of the entoptic phenomena Purkinje fig 23: Right eye; fig 24: Left eye[3].
The Purkinje tree entoptic test was performed as part of the ophthalmological examination of cataract patients at Saint Joseph Hospital. A total of 92 patients were examined and underwent surgery of whom 86 had unilateral cataract and 6 had bilateral cataracts, making a total of 98 eyes examined and operated.
Each patient was examined in a dark room, the Purkinje entoptic test was performed using a penlight (3 V, 0.12 W).With the eye closed, the light source was placed on the eyelid in the upper outer quadrant. The light was moved in a straight line parallel and perpendicular to the limbus and the patient was asked to describe what he saw (Figure 1).
A description resembling a leafless or dead tree was accepted as a positive response (Figure 2).
Best corrected visual acuity (BCVA) postoperatively ≥6/60 was considered to indicate good retinal function, while the BCVA<6/60 was considered to indicate a poor result.
Responses to the Purkinje optical test were compared to the corrected postoperative visual acuity, and analyzed statistically using Microsoft Excel and IBM SPSS Statistics.
Non-inclusion CriteriaEyes with any of the following signs were not included in the study: no light perception,pupillary-motor reflex absent, central corneal opacity, retinal detachment.
Statistical AnalysisData analysis reviewed continuous and categorical variables. Mean and standard deviations of continuous variables and are presented as mean±SD,frequencies, and percentages of categorical factors.
Evaluation of diagnostic accuracy involves calculating four objective measures of test performance, namely, sensitivity,specificity, positive predictive value (PPV) and negative predictive value (NPV).
Analysis of a 2×2 contingency table was done by using Fisher’s exact-test.
RESULTS
Socio-demographic Characteristics and Retinal FunctionMean age was 66.3±13.7y (range 16-96y) and males were predominant (63%). Preoperatively, only 7 out of the 98 eyes(7.1%) had a visual acuity of ≥6/60. Of the remaining 92 eyes(93.9%), 43 (43.9%) were able to count fingers at different distances, 22 (22.5%) saw hand movements, and 26 (26.5%)visual acuity was only light perception (Figure 3).
Postoperatively, 89 eyes (90.8%) had a BCVA equal or better than 6/60. Retinal function was assessed in terms of visual acuity and was divided into two groups: 1) good retinal function corresponded to BCVA≥6/60 and included 89 from 98 eyes tested (90.8%); 2) poor retinal function corresponded to BCVA<6/60. This group included 9 from 98 eyes (9.2%).The postoperative outcome is shown in Figure 4.
Relationship Between the Purkinje Entoptic Test and Retinal FunctionOut of all 98 eyes there were 80 (81.6%)where the Purkinje entoptic phenomenon was reported by the patient. In 18 out of these 98 eyes (18.4%) despite repeated testing there was good light perception but no tree like pattern was seen by the patients.
After cataract surgery, of the 80 eyes (81.6%) positive for the Purkinje tree, there were 75 (93.8%) with a BCVA of better than 6/60, whereas in 5 eyes (6.3%) there was a BCVA of 6/60 or less.
Out of the 18 eyes (18.4%) where no Purkinje tree was recognized, there are 14 (77.8%) with BCVA of better than 6/60, whereas in 4 (22.2%) there was BCVA of 6/60 or less(Table 1).
Therefore, sensitivity of the test was 75/89=84.3% and specificity of 4/9=44.4%. For predictive values the results were 75/80=93.8% (PPV) and 4/18=22.2% (NPV).
Rates of “postoperative good retinal function” are not significantly different (P=0.056) between patients with different test results.
DISCUSSION
Our results demonstrated that many cataract patients give a positive response to the entoptic Purkinje tree test demonstrating acceptable retinal function (81.6%). This rate is slightly lower compared to the findings of another study by Sinclairet al[14], who found an amount of 90%. It is promising that a positive test preoperatively tells that there is a 93%likelihood of a good post-operative result in an unselected group of eyes where no other information but pupil reaction to light concerning visual prognosis was available.
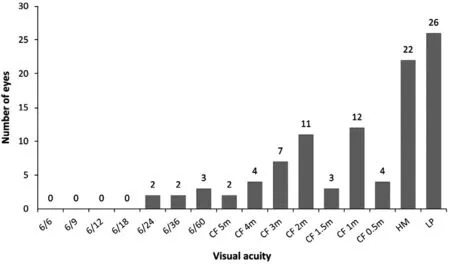
Figure 3 Distribution of preoperative visual acuity in the 98 eyes tested The 92.8% of patients had preoperative visual acuity less than 6/60. CF: Counting fingers; HM: Hand movement; LP: Light perception.

Figure 4 Distribution of postoperative best corrected visual acuity in the examined 98 eyes CF: Counting fingers.

Table 1 Preoperative responses to retinal function testing in 98 eyes of cataract patients
The reasons for false negative responses remain to be explained. If we consider the background of most of the patients who attend Saint Joseph Hospital possible reasons could include levels of education or a reduced observation sense. These reasons could be raised as hypotheses that could explain in part the false negative responses.
The fact that in eyes where no Purkinje tree was recognized also showed good post-operative results in 77.8% indicates,that there is only limited understanding by the patient of what the examiner asked for, which has also been reported by other authors[13]. Better communication between the examiner and the patient may improve this result. On the other hand, the probability of good retinal function is high if a patient gives a positive response to the Purkinje test,i.e., 93.8%, but results are not statistically significant. Conversely, if a patient gives a negative response to the Purkinje entoptic vascular test, the probability that this test predicts poor retinal function is low(22.2%).
Reviewing the literature there seem to be ways to improve the perception of entoptic phenomena. Not only the recognition of the Purkinje tree but also the foveal granular pattern can be improved by the application of red free light[15], by focusing the light beam[16], and by standardizing the application and motion of the light source[17]. There are suggestions in literature[18-19]to stimulate the recognition of both the Purkinje tree as well as the granular foveal pattern by showing the patient drawings based on retinal fluorescence angiograms and additionally creating a motion showing granules in the foveal area[18]. If it is possible to reach similar levels of recognition in low income settings as published in western literature, there will be definitely a place in the pre-operative evaluation of cataract patients in low income areas to avoid unnecessary surgery and patient disappointment.
Research is ongoing on this methodology, possibly incorporating the recognition of the so called foveal granular pattern (macula chagrin) entoptic test. As described in his Sanford Gifford Memorial Lecture in 1972 Goldmann states that if patients have a normal fovea not only are Purkinje vessel shadows visible, but the central vessel free area can be perceived as a small field covered with many dots[6].
It is reported in literature that its recognition is a reliable indicator having a postoperative visual acuity of better than 0.3 (6/18)[7,18,20]. Under highly selective conditions (50 ophthalmologists with good visual acuity) all appreciated the Purkinje vessel shadows, all but 2 perceived the vascular granular pattern[17].
In conclusion, the Purkinje entoptic test offers a simple test to assess retinal function in patients with dense cataract.Preoperatively there is good reliability in predicting acceptable retinal function. It is less reliable in predicting poor retinal function. Improvements, such as a more detailed investigation of the macular granular pattern, must be made to make it more accurate. As a result this inexpensive test could be a great alternative to help doctors decision making in areas without ocular ultrasound.
ACKNOWLEDGEMENTS
Conflicts of Interest: Dinkulu S,None;Kilangalanga NJ,None;Mukwanseke E,None;Lutete LF,None;Hopkins A,None;Guthoff RF,None;Stahnke T,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Five-year results of refractive outcomes and visionrelated quality of life after SMlLE for the correction of high myopia
- Role of glycolysis in retinal vascular endothelium, glia,pigment epithelium, and photoreceptor cells and as therapeutic targets for related retinal diseases
- Simultaneous pars plana vitrectomy, panretinal photocoagulation, cryotherapy, and Ahmed valve implantation for neovascular glaucoma
- Displacement of the retina after idiopathic macular hole surgery with different internal limiting membrane peeling patterns
- Analogs of microgravity: the function of Schlemm’s canal, intraocular pressure and autonomic nervous during the head-down tilt test in healthy subjects
- Association between cystatin C and diabetic retinopathy among type 2 diabetic patients in China: a Meta-analysis
