Disseminated hydatid disease in the orbit and central nervous system
2021-09-14MingShenMaFanSuYanHeiMeiYanFengXinJiYang
Ming-Shen Ma, Fan Su, Yan Hei, Mei-Yan Feng, Xin-Ji Yang
1Orbital Diseases Institute, Chinese People’s Liberation Army General Hospital, Beijing 100853, China
2Department of Ophthalmology, Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010050, Inner Mongolia Autonomous Region, China
Dear Editor,
We are writing to present a rare case of disseminated hydatid disease (HD) in the orbit and central nervous system (CNS) leading to visual dysfunction, and an improved surgical technique.
This rare case demonstrates intracranial multiple hydatid cysts encroaching and penetrating the orbital wall leading to orbital hydatid cyst. Surgically reducing the cyst volume may be an excellent option to avoid rupture of orbital hydatid cyst.
ETHICAL APPROVAL
The experimental protocol was established, according to the ethical guidelines of the Helsinki Declaration and was approved by the Human Ethics Committee of Chinese PLA General Hospital. The patient and her parents gave informed consent and agreed to participate in the study. The patient and her parents have provided informed consent for the use of their information and images to publish. Written informed consent was obtained from the patient and her parents.
CASE PRESENTATION
A 16-year-old girl presented with edema in the left upper lid,and proptosis and pain in the left eye for 1mo. The patient reported a pulsating sensation in the left orbit. Visual acuity was 20/20, and infero-temporal displacement of the left globe with impaired ocular motility was apparent on examination(Figure 1). The patient had undergone intracranial hydatid cyst removal surgeries twice in 2009 and 2016. Postoperatively,the patient had albendazole treatment without evidence of recurrence over a two-year follow-up period. Having completed the hematological (hemoglobin and total red blood cells, leukocyte, and platelet counts) and biochemical(serum creatinine, bilirubin, alkaline phosphatase, and alanine transaminase) examinations, the patient’s alkaline phosphatase revealed mild abnormality of the liver. The patient self-elected to discontinue the medication. A computed tomographic(CT) scan showed a low-density mass in the left orbit and the side of the left eyelid. The 3D reconstruction scan revealed a defect connecting the left orbit and the intracranial space and considered likely to have been caused by local erosion from the mass. Magnetic resonance imaging (MRI) showed an orbital hydatid cyst and multiple intracranial hydatid cysts (Figure 2). CT scan of the abdomen and chest excluded systemic dissemination.

Figure 1 Appearance of the patient before the orbital surgery.

Figure 2 Imaging revealed multiple space-occupying lesions in the brain and orbit with a hydatid cyst A, B: CT scan associated with 3D reconstruction showed the cyst in the left orbit and the local erosion of the roof of the orbital bone. C, D: MRI showed a mass irregular shape and well-circumscribed, located in left orbit, with hypo-intensity in T1, and hyper-intensity in T2. Multiple lesions were apparent in the left frontal and temporal lobes, some of which invaded brain parenchyma.
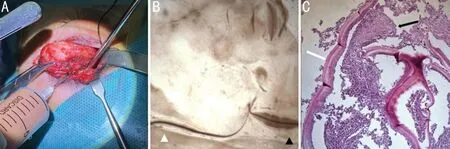
Figure 3 Surgical specimen of the hydatid cyst A: The hydatid cyst in orbit was strongly adhered to the surrounding tissues. To prevent the hydatid cyst from rupturing, the team reduce its volume with a syringe. B: The adult echinococcus (white triangle) and segment fragment of echinococcus (black triangle) are shown in liquid living tissue in a hydatid cyst with normal saline smear. C: Histopathological examination of the wall of echinococcus cyst showed the outer layer of chitosan (or fibrous layer) (white arrow) and germinal layer (black arrow).
The patient was initially diagnosed with orbital and intracranial multiple hydatid cysts. Due to the previous two intracranial excisional surgeries for hydatid cyst and the imaging findings that suggested cystic characteristic of the orbital mass and possible extension of the intracranial hydatid cysts through the evident bone defect to the left orbit, the primary diagnoses were multiple intracranial hydatid cysts with dissemination to the left orbit. On consultation with a neurosurgeon the recommendation was to not remove the intracranial lesions surgically, but to control the cysts brain using albendazole.The patient had received four weeks of albendazole treatment initially, but the eye movement obstruction and orbital swelling were not alleviated. The orbital lesions were relatively limited.The orbital cyst could be surgically reduced as much as possible to relieve the patient’s symptoms, combined with systemic medication to reduce the recurrence rate after surgery.A cystic mass was found in the orbicularis oculi muscle as shown in Figure 3A, with strong adhesion to the surrounding tissue. Moreover, the cyst had been separated, exposing its most posterior wall, and the orbital superior periosteum adhesion. Inferiorly, the cyst had strong adhesion to the levator palpebrae superioris and the two were challenging to separate.To avoid systemic anaphylaxis or local seeding caused by cyst rupture, volume reduction was performed, and the cyst contents were aspirated through a syringe. Pus-like fluid was visible, containing vesicle-like particles. The surgical team separated the cyst completely without magnifying visual aids.The intraorbital cyst was found to be relatively independent of intracranial cysts (Figure 3A). The tissue removed during surgery was assumed to be a hydatid cyst and was sent for pathological examination (Figure 3B). To prevent spillage of parasites into the surrounding tissue and to remove them if spillage occurred, the team irrigated the surgical location with hypertonic saline for 15min during the surgery. Bleeding was arrested using electrocoagulation, a drainage bar was used from the surgical location, and the surgical incision was sutured.
The postoperative period was uneventful. Seven days after the surgery, the left eye visual acuity was 20/20. Although the patient’s left eyelids were slightly swollen, the unilateral superior lid edema was less severe than pre-surgery appearance. One month after the surgery, left eye position and movements were normal in all directions. Proptosis was resolved and orbital pressure returned to normal levels.Echinococcus cysts were found in the specimen contents by pathological examinations, and the cyst wall consisted of inflammatory granulation tissue, which was confirmed to be a hydatid cyst. The patient was advised to maintain the application of albendazole and regular follow up. CT scan of the orbit was conducted post-operatively to exclude orbital hydatid cyst recurrence. The patient was followed for three months and showed no evidence of recurrence in the orbit.
DISCUSSION
In this report, we present a rare case of orbital hydatid cyst with asymptomatic CNS hydatid cysts in a 16-year-old girl. HD is a parasitic infection caused by the larvae of a tapeworm that is endemic in many regions worldwide including the Middle East, Mediterranean Basin, South America, and Australia.HD can affect any organ or soft tissue but the liver (70%),and lungs, followed by the CNS are the most frequent sites of hydatid cyst[1]. However, orbital hydatid cyst accounts for less than 2% of all hydatid cysts[2]. Some studies have shown that other hydatid cysts rarely occur concurrently elsewhere in the body, which suggests that secondary dissemination from CNS to the orbit is very rare[3-5].
The physical barrier of bony wall cannot entirely prevent the spread of HD between tissues. Hydatid cysts in the bony walls of the orbit are mostly from the bloodstream. Thinning of orbital bony walls due to hydatid cysts have been reported.However, in this case, intracranial hydatid cysts are extremely rare and spread directly into the orbit through erosion of the bony wall. A similar case has been reported previously, but the patient’s treatment process and prognosis were not reported[6].Orbital hydatid cysts, which threaten visual function, seem to respond well to surgical excision. In most cases, hydatid cysts in orbit occur singly and grow slowly[2,7-8]. Due to the possible rupture of orbital hydatid cysts, with the risks of anaphylaxis and seeding of parasites, albendazole has been recognized as a standard treatment for orbital hydatid cysts[9]. However, in the present case the orbital hydatid cyst grew and compressed the eyeball, obstructing eye movement. Urgent action is needed in such cases to alleviate symptoms and protect visual function.For these reasons, the team chose to surgically remove the cyst and treat with albendazole after surgery to control growth of the hydatid cysts in the brain.
When it is necessary to surgically excise a large hydatid cyst in the orbit, actively reducing the cyst volume may be a very good option to avoid rupture. In the current case, the wall of the hydatid cyst was very fragile and tightly adherent to surrounding tissues. To prevent rupture of the orbital hydatid cyst, we reduced the cyst’s tension through active volume reduction to ensure the complete excision of the cyst.
In summary, a case of disseminated HD in the orbit and CNS in a 16-year-old girl has been presented. HD in the orbit is a rare disease, especially since modernization of livestock production systems[1]. However, it should not be ignored that HD remains an epidemic disease, especially in developing countries[1].In clinical practice, space-occupying lesions occurring simultaneously in the orbit and CNS may suggest HD as a differential diagnosis. Surgical excision of the hydatid cysts supplemented by albendazole treatment may be considered as a rapid and effective modality in the management of cases in which compression by a cyst has altered visual function, ocular motility, or appearance of the patient.
ACKNOWLEDGEMENTS
We are very grateful to the patient and her parents for their patience and cooperation throughout the study.
Conflicts of Interest:Ma MS,None;Su F,None;Hei Y,None;Feng MY,None;Yang XJ,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Five-year results of refractive outcomes and visionrelated quality of life after SMlLE for the correction of high myopia
- Role of glycolysis in retinal vascular endothelium, glia,pigment epithelium, and photoreceptor cells and as therapeutic targets for related retinal diseases
- Predictive value of retinal function by the Purkinje test in patients scheduled for cataract surgery in Kinshasa, DR Congo
- Simultaneous pars plana vitrectomy, panretinal photocoagulation, cryotherapy, and Ahmed valve implantation for neovascular glaucoma
- Displacement of the retina after idiopathic macular hole surgery with different internal limiting membrane peeling patterns
- Analogs of microgravity: the function of Schlemm’s canal, intraocular pressure and autonomic nervous during the head-down tilt test in healthy subjects
