Socio-economic disparity in visual impairment from cataract
2021-09-14ZhiFangXinYiChenLiXiaLouKeYao
Zhi Fang, Xin-Yi Chen, Li-Xia Lou, Ke Yao
1Eye Center of the Second Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou 310009, Zhejiang Province, China
2Eye Institute of Zhejiang University, Hangzhou 310009,Zhejiang Province, China
Abstract
● KEYWORDS: visual impairment; socioeconomics;cataract burden
INTRODUCTION
As the leading causes of blindness, cataracts are also the second leading cause of visual impairment worldwide[1].Global moderate to severe visual impairment (MSVI) and blindness caused by cataract has been growing dramatically in recent years[1-2]. Given the increasing number of people and the aging of the population, the prevalence rates of global MSVI and blindness caused by cataract are estimated to be 57.1 million and 13.4 million, especially in 2020[1].
Because the problem of visual impairment brings a further financial burden, impairs quality of life, and increases humanistic burden or causes mental illness development[3-4].The so-called disability-adjusted life years (DALYs) are the combination of years of life lost due to premature death and years of disabled life. In general, the number of DALYs and the years lived with disability (YLDs) of cataracts were the same. The 204 countries were involved in the published study on the global burden of disease in 2019, which revealed that the DALY rates of cataract decreased from 93.2 in 1990 to 82.9 in 2019. Moreover, cataract showed the largest burden of 6.68 million DALYs in 2019. That’s more than 6.57 million DALYs for uncorrected ametropia[5].
However, the imbalance in the global burden of cataract is a major concern in efforts to reduce preventable blindness owing to cataract. The factors involved include gender[6], ethics[7], and socioeconomic state[8]. Compared with male patients, women have a higher proportion of cataract caused visual impairment,a higher age-standardized DALY rate, and a lower coverage rate of cataract surgery[6,9]. There is a negative correlation between age-standardized DALY rate of cataract and human development index (HDI)[8]. Visual impairment is more common in low- and middle-income countries. However, the economic burden on high-income countries remains heavy[10].However, the trend of cataract burden by different degrees of visual impairment or different income levels and the intrinsic association with socioeconomic status remain unknown.Thus, identifying the underlying inequality of cataract burden by different degrees of visual impairment would provide important reference for health care decision making to reduce preventable blindness and meet the global action plan (GAP).The purpose of this study was to investigate the differences in the global burden of cataract among populations according to degrees of visual impairment over time and across countries and the association of the global burden with socioeconomic status by analyzing the YLD data from the Global Burden of Disease (GBD) 2019 study[5].
SUBJECTS AND METHODS
Ethical ApprovalThe data in this study was accessed from the public databases and websites without human participants or animals. Thus, no ethical problems was involved.
Study DesignThis work is an international, comparative study focusing on disease burden.
Global Burden of CataractThe age-standardized YLDs per 100 000 population was used to estimate global burden of cataract (ICD-10 codes H25-H26 and H28-H28.210) of 204 countries in the GBD 2019 study[5]. In the study, the calculation methods of age-standardized YLDs have been described[5].GBD data concerning cataract were collected from the Global Health Data Exchange (Global Health Data Exchange. GBD Results Tool. Available at http://ghdx.healthdata.org/gbdresults-tool. Accessed on October 29, 2020). These data included 1) global age-standardized YLD rates among populations according to world bank income levels from 1990 to 2019 and 2) national age-standardized YLD rates of populations according to degrees of visual impairment (i.e., moderate vision loss, blindness, and severe vision loss) in 2019.
National Socioeconomic StatusThe HDI is a measure of income, health and education. Therefore, for a country, its social and economic indicators are usually measured by HDI,which ranges from 0 to 1. A larger value indicates a higher level of social and economic development. Data on the 2019 HDI can be found in the 2020 Human Development Report released by the United Nations in 2019. We can find that in 2019, the world HDI values can be divided into four groups:low HDI (<0.554), medium HDI (<0.703 to ≥0.554), high HDI(<0.804 to ≥0.703), and very high HDI (≥0.804).
Statistical AnalysisKruskal-Wallis test was conducted to assess the difference of age-standardized YLD rates between HDI-based country groups considering the non-normal distribution of YLD data[11]. The Mann-WhitneyUtest with Bonferroni correction was used in multiple comparison tests.The effect of HDI on the age-standardized YLD rate was analyzed by linear regression analysis. All statistical data were analyzed with SPSS 23 (USA). When the bilateralPvalue of<0.05, it represents the statistical significance.

Figure 1 Trends in the global burden of cataract resulting in visual impairment and blindness among populations with different World Bank income levels from 1990 to 2019 YLDs:Years lived with disability.
RESULTS
Trends in the Global Burden of Cataract by Visual ImpairmentIf the population size and age structure are controlled, the agestandardized YLD rates of population visual impairment and blindness caused by cataracts gradually decreases from the 102.7 in 1990 [95% uncertainty interval (UI): 70.4-142.5] to 91.6 in 2019 (95% UI: 63.7-126.7), with an obvious decrease from 260.5 (95% UI: 179.3-360.2) to 203.6 (95% UI: 140.7-283.3) among those with World Bank lower middle income,implying global health progress in cataract. This is especially true among low- and middle-income groups (Figure 1).
We obtained age-standardized YLD rates for the period 1990 to 2019 from three groups, depending on the severity of visual impairment: blindness, moderate vision loss, and severe vision loss. As shown in Figure 2A, the age-standardized YLD rates of populations with blindness due to cataract declined from 54.7 (95% UI: 36.9-78.5.0) to 36.9 (95% UI: 24.9-53.9),with obvious decrease among those with World Bank lower middle income from 146.9 (95% UI: 98.8-208.8) to 87.2 (95%UI: 58.9-125.3), implying great health progress in cataract blindness among the lower middle-income population. As observed in Figure 2B, 2C, the age-standardized YLD rates of populations with severe and moderate vision loss due to cataract increased from 1990 to 2017 and decreased rapidly after 2018.
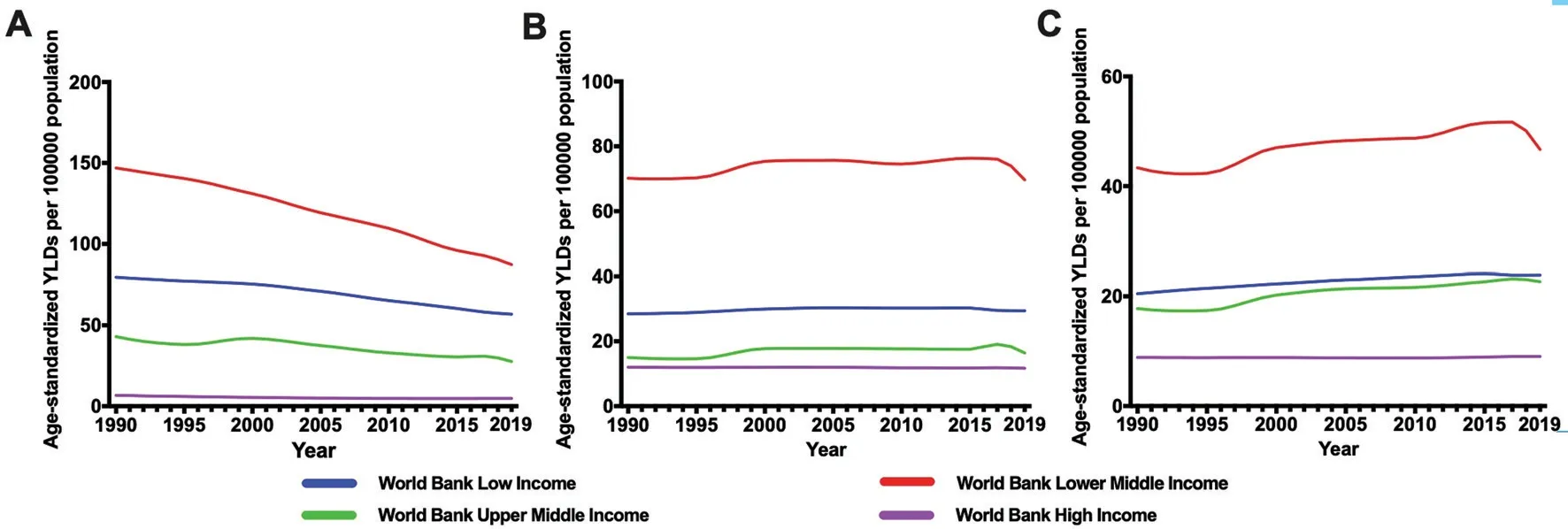
Figure 2 Trends in the global burden of cataract among populations with different World Bank income levels from 1990 to 2019 Trends in the global burden of cataract resulting in blindness (A), severe vision loss (B), and moderate vision loss (C) were shown respectively. YLDs:Years lived with disability.
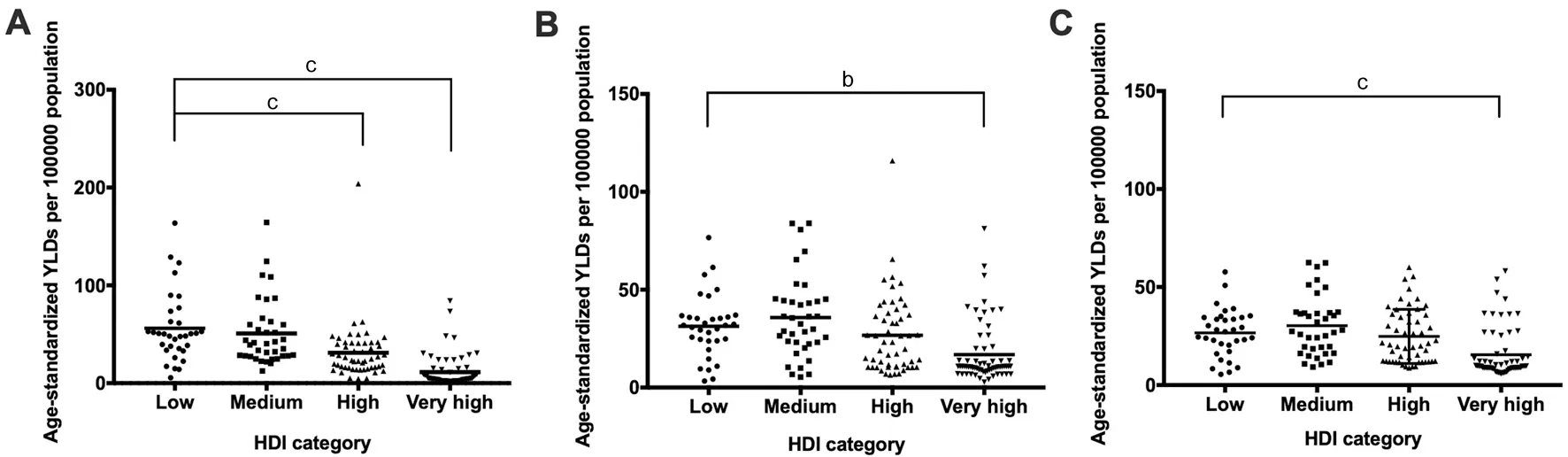
Figure 3 Cataract burden differed significantly across countries with different levels of socioeconomic development Age-standardized YLDs for patients with blindness (A), severe vision loss (B), and moderate vision loss (C) were analyzed respectively. The lines represent medians. The bars represent 95% confidence interval. YLDs: Years lived with disability; HDI: Human development index. Compared with low HDI group: bP<0.01, cP<0.001.
Socioeconomic Difference in Cataract Burden of Visual ImpairmentHDI in 2019 were available for 187 countries among 204 countries in global burden disease study, which included 33 low-HDI countries, 37 medium-HDI, 53 high-HDI and 64 very high-HDI.
According to the results of Kruskal-Wallis test, for countries with different levels of economic development, the corresponding age-standardized YLD rate also has a significant difference(P<0.001). According to multiple comparison analyses of the Mann-WhitneyUtests, countries with lower HDI had higher age-standardized YLD rates of blindness burden due to cataracts compared with countries with higher HDI (P<0.001)and countries with very high HDI (P<0.001, Figure 3A). The burden of severe vision loss due to cataract in countries with low HDI showed significantly higher age-standardized YLD rates than those with very high HDI (P<0.01, Figure 3B) and significantly higher age-standardized YLD rates of moderate vision loss than those with very high HDI (P<0.001, Figure 3C). The medians (interquartile ranges) of the age-standardized YLD rates of blindness in low-HDI, medium-HDI, high-HDI,and very high-HDI countries were 50.3 (35.4-62.9), 40.5 (27.9-60.0), 24.9 (15.9-41.0), and 4.4 (2.4-12.4), respectively.
Association Between HDI and Visual Impairment due to CataractThe age-standardized YLDs rates among populations with blindness (r=-0.588, adjustedR2=0.346,standardizedβ=-0.588,P<0.001), severe vision loss (r=-0.378, adjustedR2=0.143, standardizedβ=-0.378,P<0.001),and moderate vision loss (r=-0.389, adjustedR2=0.151,standardizedβ=-0.389,P<0.001) inversely correlated with HDI. According to Pearsonr[12], fair correlations were found between age-standardized YLDs rates with HDI among populations with blindness, severe vision loss, and moderate vision loss (Figure 4).
DISCUSSION
This study revealed the trends and association between cataract burden according to degrees of visual impairment and socioeconomic state. The cataract burden of populations with different degrees of visual impairment was inversely associated with national socioeconomic development. Although cataract health care has improved in recent years, countries with low HDIs were still found to have significantly higher cataract burden than those with high HDIs, especially among those with blindness.
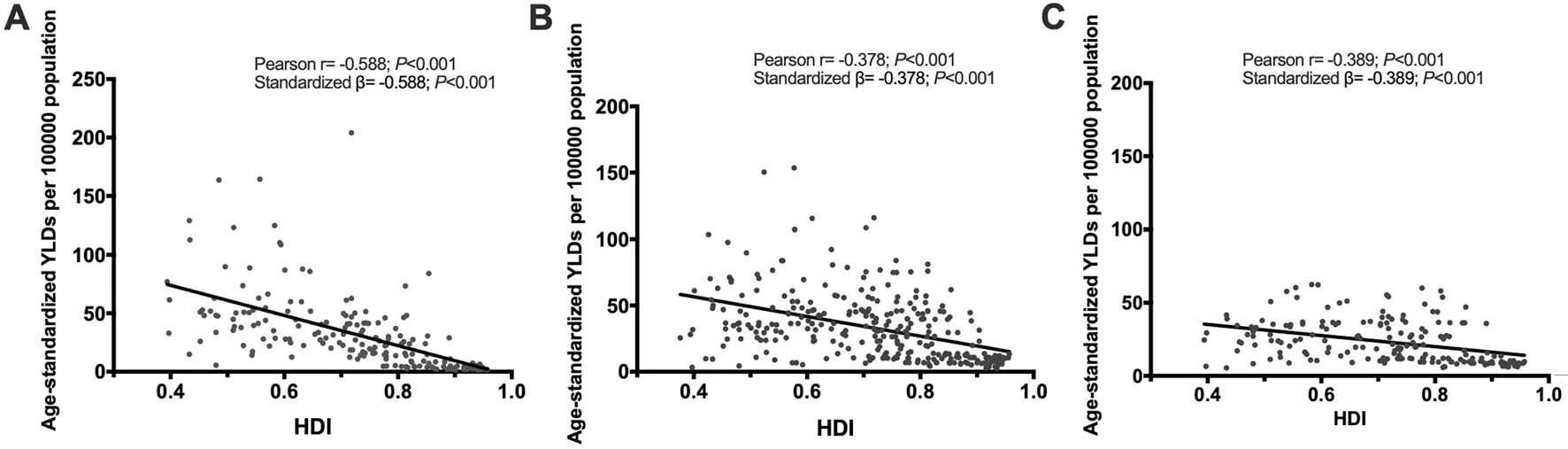
Figure 4 Cataract burden was inversely associated with the national socioeconomic development Cataract burden among populations with blindness (A), severe vision loss (B), and moderate vision loss (C) were analyzed respectively. The best-fitted line by linear regression analysis is presented. YLDs: Years lived with disability; HDI: Human development index.
The age-standardized YLD rates of lower middle-income populations with blindness caused by cataract decreased rapidly since 2000, which was consistent with the reported improved cataract surgery access and increased concentration indexes of cataract burden across countries since 2000[8].Multiple comparison tests revealed that countries with low HDI had significantly higher age-standardized YLD rates of blindness due to cataract than those with high and very high HDI among populations with blindness. Interestingly, no differences were found between low-, medium-, and high-HDI groups among those with severe or moderate vision loss.These results indicated that the difference in cataract burden across countries was mainly concentrated in populations with blindness. The timely identification of blind people,appropriate surgery criterion for cataract surgery[13], sufficient ophthalmologists, increased cataract surgery rate (CSR)[14], and health care report and screen system[15]are important points of focus to effectively decrease preventable cataract blindness in countries or areas with low socioeconomic states.
According to a 2019 GBD study, we found a fair association between HDI and age-standardized YLDs rates in people with moderate vision loss, those with severe vision loss, and those with blindness. Despite socioeconomic, gender, and regional differences, there was a negative correlation between HDI and cataract burden due to visual impairment. Even though visual impairment is more common in middle- and low-income countries, the economic burden in high-income countries is still significant[16], which may relate to increasing life expectancy and easy access to health service. Considering the unequal distribution of GDP between and within countries and the inaccurate reports of cataract surgery among low-income populations, improved health care and cataract surgery access are beneficial in areas with low socioeconomic states.
The visual impairment caused by cataract can be restored by surgical intervention effectively. CSR is a proxy measure of eye care delivery and access to cataract surgery services and is closely associated with socioeconomic status[17-18]. CSR is mainly determined by three factors—visual acuity cut-off for cataract surgery, the age structure of a community, and cataract surgical coverage from need-based estimates. HDI is strongly associated with the prevalence of cataract blindness,CSR, proportion of intraocular lens implantation, and proportion of cases with good vision outcomes[19]. The CSR of developing countries is approximately 500-2000, which is far behind that of developed countries (i.e., 4000-10 000). For enterprises in most countries, corporate social responsibility is also improving as time goes on. However, from a global perspective, the inequality between CSR remains relatively stable[17]. Given the uneven distribution of ophthalmologists across and within countries[20], the correlation between high GDP and high CSR may not reflect the true access to cataract surgery, especially for patients in low socioeconomic areas.Therefore, eliminating cataract blindness in those in low socioeconomic areas is the key to achieve the goal set by the GAP.This study mainly focuses on GBD 2019 study, mainly including data sources and statistical assumptions in the research report[5]. There might be bias coming from the use of aggregate data as national instead of district because geographic variations in YLD estimates may occur. Although this study provided an international view of differences between countries in cataract burden by visual impairment,the conclusions may not be applicable to a specific district,given that inequality existed even within countries. Given that the GBD study will update annually and considering the percentage change of visual impairment, changes in the global burden of cataract due to visual impairment in the long term need further investigation as the GAP is being carried out and efforts to improve cataract surgery access are being made.
ACKNOWLEDGEMENTS
Foundations:Supported by the National Key Research and Development Project of China (No.2018YFC1106104); the National Natural Science Foundation of China (No.82000948;No.81870641; No.82070939); the Zhejiang Provincial Key Research and Development Project under Grant(No.2020C03035); the Natural Science Foundation of Zhejiang Province under Grant (No.LQ20H120007).
Conflicts of Interest: Fang Z, None; Chen XY, None; Lou LX, None; Yao K, None.
杂志排行
International Journal of Ophthalmology的其它文章
- Five-year results of refractive outcomes and visionrelated quality of life after SMlLE for the correction of high myopia
- Role of glycolysis in retinal vascular endothelium, glia,pigment epithelium, and photoreceptor cells and as therapeutic targets for related retinal diseases
- Predictive value of retinal function by the Purkinje test in patients scheduled for cataract surgery in Kinshasa, DR Congo
- Simultaneous pars plana vitrectomy, panretinal photocoagulation, cryotherapy, and Ahmed valve implantation for neovascular glaucoma
- Displacement of the retina after idiopathic macular hole surgery with different internal limiting membrane peeling patterns
- Analogs of microgravity: the function of Schlemm’s canal, intraocular pressure and autonomic nervous during the head-down tilt test in healthy subjects
