Predictors of in-hospital mortality by logistic regression analysis among melioidosis patients in Northern Malaysia: A retrospective study
2021-09-11KamaruddinMardhiahNadiahWanArfahNyiNyiNaingMuhammadRadziAbuHassanHuanKeatChan
Kamaruddin Mardhiah, Nadiah Wan-Arfah, Nyi Nyi Naing, Muhammad Radzi Abu Hassan, Huan-Keat Chan
1Faculty of Entrepreneurship and Business, Universiti Malaysia Kelantan, Kota Bharu, Kelantan, Malaysia
2Faculty of Health Sciences, Universiti Sultan Zainal Abidin, Gong Badak Campus, Kuala Terengganu, Terengganu, Malaysia
3Faculty of Medicine, Universiti Sultan Zainal Abidin, Kuala Terengganu, Terengganu, Malaysia
4Clinical Research Center, Hospital Sultanah Bahiyah, Ministry of Health Malaysia, Alor Setar, Kedah, Malaysia
ABSTRACT
KEYWORDS: Melioidosis; Infectious disease; Mortality;Predictors; Prognostic factors; Logistic model
1. Introduction
Melioidosis is affected by Gram-negative bacilli, Burkholderia(B.) pseudomallei. This bacteria is common in soil and freshwater saprophytes, generally found in rice paddy fields in tropical and subtropical areas. Melioidosis is an emerging infectious disease in developing countries, more likely in Southeast Asia and Northern Australia[1]. The disease is also found in developed countries due to the importation and traveling of the cases[2]. Firstly, it was documented in 1911 in Burma[2], followed by Malaysia and Singapore in 1913[3]. Despite the highest number of cases each year in Thailand, this country reported its first case in 1955[3], while the first case was reported in Australia in 1949[3]. In Australia's Northern Territory, the incidence rate is 50.2 cases per 100 000 population from 2009 to 2010[4]. Globally, the incidence of melioidosis per year was 165 000 people (95% CI 68 000-412 000), with a total of 89 000 (95% CI 36 000-227 000) deaths[5].
The exact incidence of melioidosis in Malaysia is unidentified as it is not a notifiable disease, although over a thousand cases have been reported all over Malaysia[6]. Around the 1980s in Malaysia,this disease was associated with hospitals' high mortality rate,particularly in the septicaemic form, which was 65.00%. The mortality rate reduced in the past 20 years after introducing the new treatment[7]. The incidence in Malaysia may vary between states,and even within the same state, there may be various hotspots[8]. The incidence of melioidosis in Pahang, where agriculture is the main economic activity, recorded culture-confirmed adult melioidosis of 6.1 per 100 000 population per year from 2000-2003. The state of Kedah, situated at the Malaysia-Thailand border and the largest rice producer in Malaysia, reported 16.35 per 100 000 population a year[9]. A recent study reported the direct medical cost of treating melioidosis patients in Kedah, Malaysia, was $233.61, and the cost increased with the increase of the length of hospital stay[10]. Another current study in the West Part of Pahang, Malaysia, compared the inhospital mortality between patients admitted for tropical acute febrile illness[11]. The tropical acute febrile illness includes in the study were leptospirosis, dengue, bacteremia, and melioidosis. The study reported that melioidosis patients increased the odds of in-hospital mortality by 5.002 times compared to patients with a diagnosis other than melioidosis. It showed that other acute febrile illnesses in the study had no significant associations with in-hospital mortality[11].
Previous studies in Malaysia defined melioidosis's risk factors,including pre-existing comorbid conditions, older age, occupational exposure, inappropriate treatment, and male[9]; these factors also lead to mortality and recurrence of melioidosis[12]. In Malaysia,Hassan et al.[9] had identified the incidence and risk factors of melioidosis in Kedah from 2005 to 2008 retrospectively. The present study performed in the same hospital and added another hospital.This study also updates the current status of melioidosis, expanding the survey from 2014 to 2017, and added additional reports on the risk factors of mortality from melioidosis using odds ratio (OR).Mardhiah et al. had reported using the Cox model of predicting the mortality of melioidosis based on the same population[13]. The current study was conducted to identify the overview of patients'characteristics of dying from melioidosis and their predictor variables from 2014-2017 in Hospital Sultanah Bahiyah, Kedah(HSB) and Hospital Tuanku Fauziah (HTF) using the logistic model.
2. Subjects and methods
2.1. Data collection
A retrospective cohort study research design was applied to review 453 melioidosis patients in HSB and HTF from 1 January 2014 to 31 December 2017. The documentation and data collection procedures followed the expert's suggestion, with Melioidosis Registry format guidance. The data on demographic data, clinical presentation,history of melioidosis, comorbidities, antibiotic received throughout the admission, and investigation findings were documented and analyzed. The patients' personal information, like name and hospital reference number, was not accessed in accordance with the institution's ethical standards and the Malaysian research committee.The final sample size obtained was 453 patients, calculated using the Power and Sample Size Calculation (PS) software. Multiple imputations were applied for the missing data of continuous variables.
2.2. Selection of study participants
All 510 melioidosis patients admitted to HSB and HTF were evaluated for the study's possible inclusion and exclusion criteria during the study period. The study includes all culture-confirmed melioidosis in HSB and HTF and adult patients aged over 15 years old. In order to reduce bias in the diagnosis of melioidosis, patients diagnosed by the serology only were excluded from the study. Other than that, patients who died within the 24 hours admission also were excluded from the study. Following these criteria, 18 patients (3.53%)aged less than 15 years old, four patients (0.78%) who had positive HIV, and 23 patients (4.51%) were not included in the final analysis.After excluding all 45 patients that did not fulfill the criteria, we included only 453 patients to study according to the sample size calculation stated in data collection part. The simple random sampling method was then applied in order to select 453 patients from 465 patients among those who fulfilled the criteria. Figure 1 illustrated the flow of the study.
2.3. Study definitions
The type of melioidosis distribution was categorized into bacteremic melioidosis (positive B. pseudomallei in the blood)and non-bacteremic melioidosis (positive B. pseudomallei in other than blood sites such as tissue, urine, wound, sputum, and stool).Variable jobs were classified into low and high risk according to the hazards of exposure to B. pseudomallei from the soil and water.The predictors of mortality were based on the socio-demographic,antibiotic received, comorbidities, previous history of melioidosis,and blood investigations. The patient's outcome was recorded as discharged well, "at own risk" discharge, transfer to other hospitals,or died in the data collection form. Then, it was categorized into died and survived to identify the logistic model of mortality from melioidosis.
2.4. Statistical analysis of baseline characteristics and risk factors
All the statistical analyses were performed by using IBM SPSS Statistics version 26.0. Descriptive analysis-the frequency (n) and percentage (%) used for the categorical variable, while mean and standard deviation were used for the numerical variables of the patient's overall outcome and clinical presentation. Correlation between each predictor variable and the survival outcome was identified using Pearson's Chi-square or Fisher's exact test for the categorical variables. For the continuous variable, the independent t-test was used. The normality assumption for the independent t-test was assessed by graphing the histogram for each group.
2.5. Advanced multiple logistic regression analysis

Statistical analyses were performed using STATA/SE 14.0 for Windows (SAS Institute, Inc., Cary, NC). Univariate logistic regression analysis was applied to screen the association between each associated factor (demographic data, history of melioidosis,comorbidities, antibiotic received throughout the admission, and investigation findings) with the patient's outcome. Only the variables associated with mortality that produced P-values less than 0.25 in the univariate analysis were input in the multivariate regression analysis.
Multivariate regression analysis was used to estimate the predictors of mortality from melioidosis. The stepwise selection method was applied to adjust the interaction between the predictor variables. A P-value of 0.05 was considered statistically significant. The final logistics models were concluded after possible multicollinearity and interactions were tested for the model, checking the Hosmer-Lemeshow test, classification table, area under the curve, and applied the regression diagnostic test and remedial measure. The final model interpreted the ORs and 95% confidence intervals (95%CIs) to estimate the association between death and the independent predictors of melioidosis mortality.
2.6. Ethics statement
Approval of the study was obtained by Universiti Zainal Abidin Human Research Ethics Committee (UHREC) (protocol code:UniSZA/UHREC/2019/119) and Medical Research and Ethics Committee (MREC), Ministry of Health Malaysia (MOH) [NMRR-19-3090-46158 (IIR)].
3. Results
3.1. Overview of melioidosis patients admitted to HSB and HSF
Between January 2014 to December 2017, a total of 227 (50.11%)patients died from melioidosis, 159 (35.09%) patients were discharged well, 16 (3.53%) patients were "at own risk" discharge,and 51 (11.25%) patients were transferred to another hospital.The majority of the patients (98.23%, 445/453) were cultureconfirmed, and a combination of culture and serology diagnosed 1.77% of patients (8/453). During the admission, the main clinical presentations among the melioidosis patients were fever and cough.The fever occurred in 387 patients (85.43%), and 226 patients(49.89%) presented with cough. Other clinical presentations, like the presence of sputum and abdominal pain, were reported in 95(20.97%) patients and 69 patients (15.23%), respectively (Table 1).
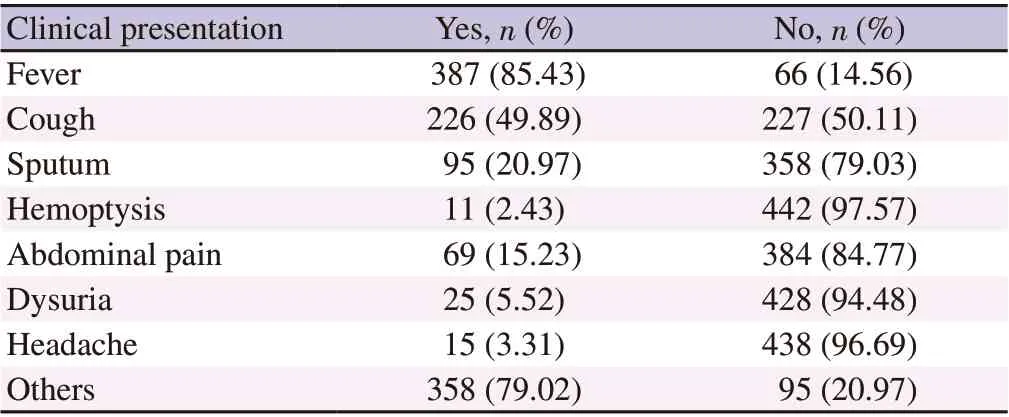
Table 1. Clinical presentation of melioidosis patients in HSB and HTF(n=453).
3.2. Comparison of baseline characteristics and risk factors based on patient's outcome
Table 2 compares the characteristics and risk factors between thesurviving and deceased (Table 2). A total of 161 patients (70.93%)did not receive any antibiotics during the admission and died, and 77 patients (34.07%) who received the antibiotics during the admission survived. A total of 219 patients (96.48%) died due to bacteremic melioidosis. Among patients who died, 153 patients had underlying diabetes mellitus, followed by 82 patients with hypertension, and 35 patients had chronic kidney disease. Also, 97 (42.73%), 178(78.41%), and 175 (77.09%) patients who died had an abnormal count of platelet, white blood cells, and urea, respectively.
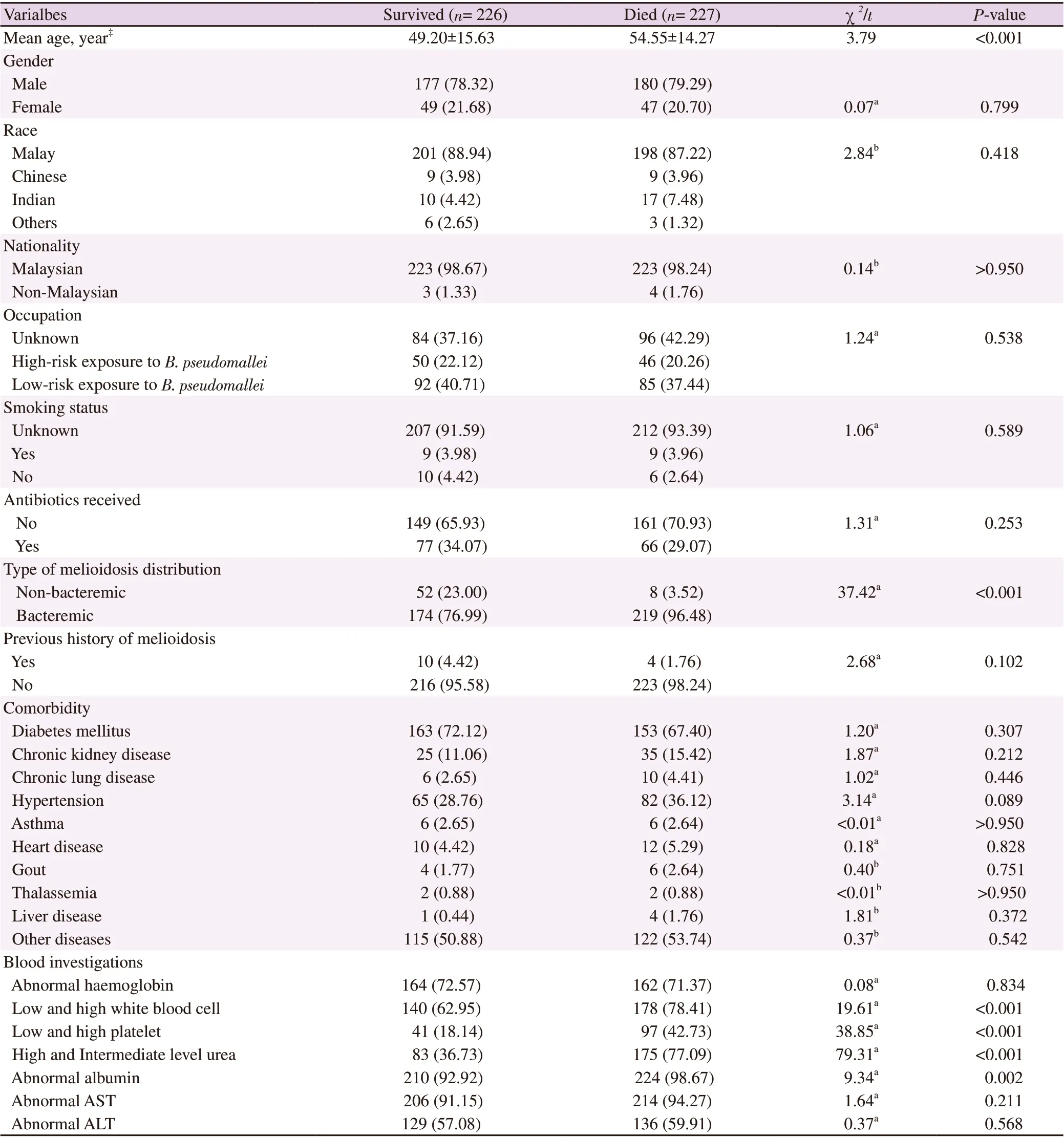
Table 2. Characteristics of melioidosis patients in HSB and HTF [n (%)].
3.3. Univariate analysis of predictors associated with mortality in melioidosis patient
In univariate logistic regression analysis (Table 3), the modelfound 13 significant factors (P<0.25) and one clinically important variable (diabetes mellitus) to be included in the multivariate logistic regression analysis: age, type of melioidosis, previous history of melioidosis, chronic kidney disease, hypertension, liver disease,white blood cell, platelet, urea, creatinine, albumin, and AST.

Table 3. Univariate analysis of predictors of mortality in melioidosis using simple logistic regression analysis (n=453).
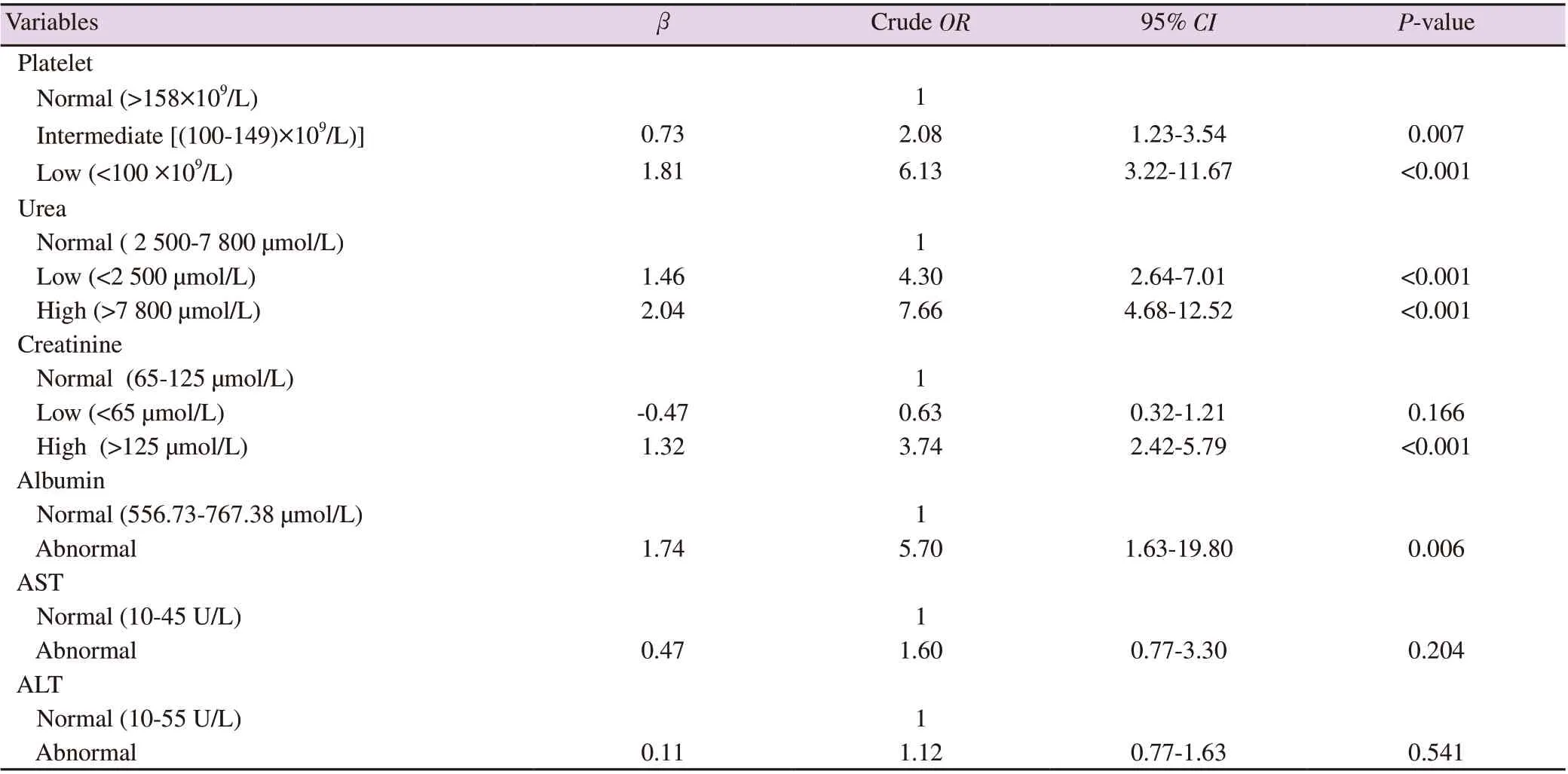
Table 3. Continued.
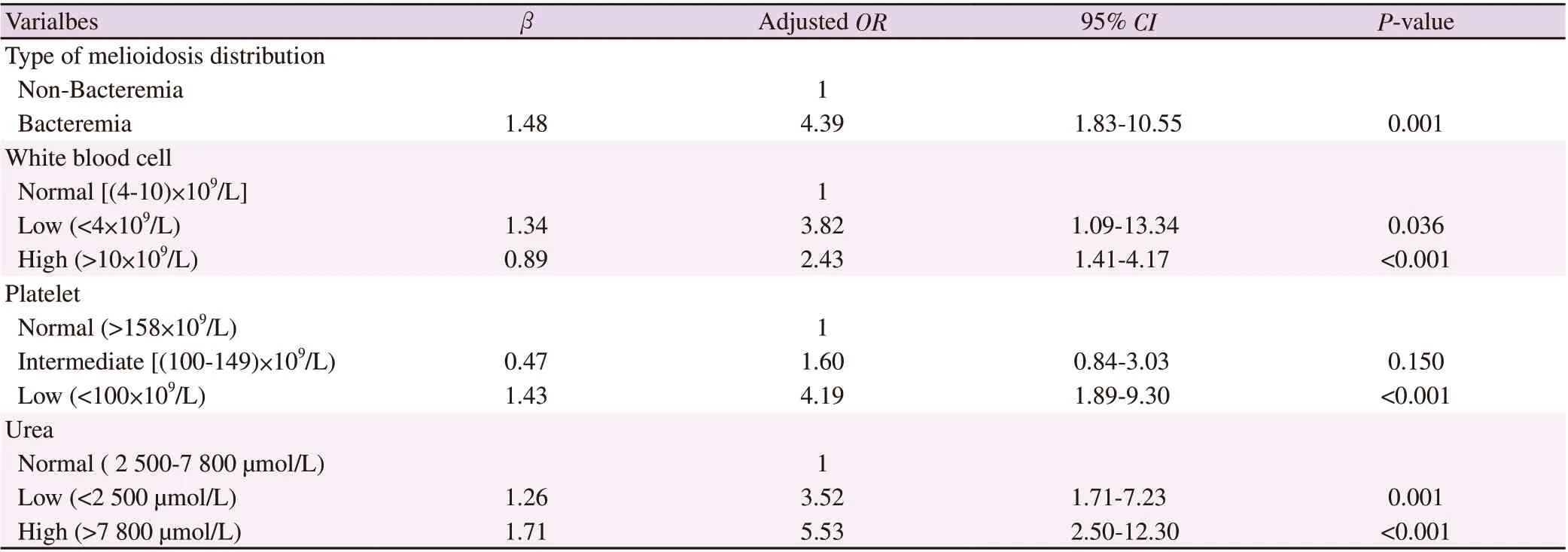
Table 4. The final model of predictors associated with mortality from melioidosis patients in HSB and HTF using multiple logistic regression analysis(n=453).
3.4. The final logistic model of mortality in melioidosis patients
In multivariate logistic regression analysis (Table 4), the model found four significant factors associated with mortality from melioidosis: the type of melioidosis distribution, white blood cell count, platelet count, and urea level. The results indicate bacteremic melioidosis increased the risk of dying from melioidosis by 4.39 (OR 4.39, 95% CI 1.83-10.55, P=0.001) compared to non-bacteremic melioidosis. Based on laboratory test, the adjusted ORs from the final model showed that all three blood investigations were included as the associated factors of mortality for the disease (low platelet:OR 4.19, 95% CI 1.89-9.30, P<0.001; high white blood cell: OR 2.43, 95% CI 1.41-4.17, P<0.001; low white blood cell: OR 3.82,95% CI 1.09-13.34, P=0.036; high urea: OR 5.53, 95% CI 2.50-12.30, P<0.001; and low level of urea: OR 3.52, 95% CI 1.71-7.23,P=0.001).
4. Discussion
In this study, melioidosis patients were presented with fever and cough during admission to the hospital. Fever and cough were reported as the most common presentation in melioidosis patients during admission in a study conducted at Hospital Universiti Sains Malaysia, Kelantan[14].
We agree with the previous study from Manipal that diabetes mellitus was not the factor that contributed to the mortality from melioidosis[15]. We found that underlying diabetes mellitus was not statistically significant with the mortality due to melioidosis.The finding contrasts with another study in Malaysia that reported diabetes mellitus was the predictor of mortality from melioidosis[9,12]. Another study by Mardhiah et al. reported based on the same population using the Cox model identified that diabetes mellitus becomes a protective variable towards mortality[13].
It is common for bacterial infection patients to have a high white blood count due to the fever and presence of sepsis[14]. Our finding showed that the chance of dying from melioidosis increased by 2.43 times when patients have higher white blood cells. Besides,our study observed a lower white blood count (< 4×10/mL) in dead patients compared to those who survived. The finding was similar to a study in Khon Kaen Hospital, Thailand, which found that decreasing the white blood cell count increased the chance of dying from melioidosis by 7%[16]. We also note a high mortality rate in bacteremic melioidosis with a total of 96.5%. From the literature,since the bacteria was present in the blood, most bacteremic patients will have a high white blood cell[17]. We agree with several studies that reported bacteremic increased the chance of melioidosis mortality[18,20]. Chien et al. found that patients with bacteremic melioidosis reduced the chance of getting survival by 98% (OR 0.02,95% CI 0.00-0.25)[17].
Here, we show that platelet count is another clinical blood investigation detected as a predictor of mortality from melioidosis.The correlation between thrombocytopenia and high mortality from melioidosis was reported in previous studies[19,20]. The thrombocytopenia was related to the lower immune system that reflects the severity of the disease[22]. Melioidosis patients with low platelet were observed to have the underlying disease, leading to mortality. Another study that was conducted among sepsis patients reported that sepsis was correlated with the low platelet count and increased the chance of dying[23,24].
In past studies, renal failure was reported as the risk factor of mortality from melioidosis[25-27]. Our result found that having the underlying renal disease was not correlated with mortality from melioidosis. Our finding shows that renal dysfunction based on the urea count was one of the predictors. The discovery is in line with a study that was conducted at Khon Kaen Hospital, Thailand, which reported the blood urea nitrogen was one of the predictor factors of mortality from melioidosis[16]. It was reported that the risk of death from melioidosis increased by 5.7% for every one mg/dL increase of blood urea nitrogen[16]. The importance of monitoring the renal function during hospital admission was highlighted in several studies as it was positively correlated with mortality in melioidosis patients.The high blood urea nitrogen level in patients demonstrating renal impairment and patients with these clinical features were more likely to die from the infection[16,28].
The study's findings have provided an updated major review of predictors of mortality among melioidosis patients in the Malaysian endemic area. The findings may be general in other endemic areas in Malaysia since similar clinical routines and investigations were applied in all hospitals in Malaysia. The strength of the study is the large sample size was used. All patients included in the study were culture-confirmed positive B. pseudomallei was considered as the gold standard in detecting these bacteria. The study's limitation is that we cannot identify the lack of information to identify either the patients received the delayed treatment or not. The data are very important to prevent bias in assessing the predictors of mortality from melioidosis. It is suggested to use a prospective study for future studies to collect more detailed information on this. Other than that,since the lower platelet and white blood cell may be the indicator of early sepsis in melioidosis[16,24,25,29], it is recommended to identify the correlation between these clinical factors and the presence of sepsis among melioidosis patients. There was not enough available data to investigate the relationship between these variables in the current study.
In conclusion, four predictor factors that were associated with mortality in melioidosis were bacteremic melioidosis, high and low white blood cell count, low platelet count, high and low urea level. The clinical blood investigations represent the majority of the predictor factors found in the current study. The physicians should be alert with the high mortality rate among the bacteremic melioidosis(96.47%, 219/227), and rapid treatment during admission may be needed among these patients. During hospital admission, routine blood investigations screening can be used as an early indicator of treating melioidosis patients without delay in reducing the mortality rate.
Conflict of interest statement
The author reports that no conflicts of interest are involved in this research. The datasets used for the current study are available from the corresponding author on reasonable request.
Funding
The project was supported by Universiti Sultan Zainal Abidin (grant number: UniSZA/2018/DPU/16).
Authors’ contributions
Nadiah Wan-Arfah and Nyi Nyi Naing were involved in planning and supervised the work, Kamaruddin Mardhiah processed the data, performed the analysis, drafted the manuscript and designed the figures. Muhammad Radzi Abu Hassan and Huan-keat Chan involved with the project administration and resources. All authors discussed the results and commented on the manuscript.
杂志排行
Asian Pacific Journal of Tropical Medicine的其它文章
- Prevalence and clinical significance of antiphospholipid antibodies among hospitalized COVID-19 patients
- EWMA control chart based on its first hitting time and coronavirus alert levels for monitoring symmetric COVID-19 cases
- Co-expression of HBZ, TAX and FOXp3 and HTLV-1-associated myelopathy/tropical spastic paraparesis development in HTLV-1-infected individuals: A systematic review
- Failure of space spraying to eliminate dengue virus-infected Aedes aegypti may explain failure to prevent secondary cases in Southern Thailand
- Determinants of COVID-19 vaccine acceptance and encountered side-effects among the vaccinated in Bangladesh
