Complications in growth-friendly spinal surgeries for early-onset scoliosis:Literature review
2021-08-23MichaLatalskiMarekFatygaIreneuszSowaMagdalenaWojciakGrzegorzStarobratAnnaDanielewicz
Michał Latalski,Marek Fatyga,Ireneusz Sowa,Magdalena Wojciak,Grzegorz Starobrat,Anna Danielewicz
Michał Latalski,Anna Danielewicz,Children Orthopaedic Department,Medical University of Lublin,Lublin 20-093,Poland
Marek Fatyga,Grzegorz Starobrat,Children Orthopaedic Department,University Hospital for Children,Lublin 20-093,Poland
Ireneusz Sowa,Magdalena Wojciak,Department of Analytical Chemistry,Medical University of Lublin,Lublin 20-093,Poland
Abstract BACKGROUND The treatments for early-onset scoliosis(EOS),defined as curvature of the spine with onset before 10 years of age,continue to pose a great challenge for pediatric orthopedics.The treatment goals for EOS include minimizing spinal deformity while maximizing thoracic volume and pulmonary function.Different surgical techniques have different advantages and drawbacks;however,the two major concerns in the management of EOS are repeated surgeries and complications.AIM To review the current literature to assess the safety of EOS surgical treatment in terms of the rate of complications and unplanned surgeries.METHODS In January 2021 two independent reviewers systematically searched three electronic medical databases(PubMed,the Cochrane Library,and Embase)for relevant articles.Every step of the review was done according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.Due to the heterogeneity of articles and topics after data analysis,a descriptive(synthetic)analysis was performed.RESULTS A total of 2136 articles were found.Forty articles were included in this systematic review,after applying our inclusion and exclusion criteria.EOS surgery has a varying but high rate of complications.The most frequent complications were categorized as implant(54%),general(17%),wound(15%)and alignment(12%).The rate of complications might have been even higher than reported,as some authors do not report all types of complications.About 54% of patients required unplanned surgeries due to complications,which comprised 15% of all surgeries.CONCLUSION The literature concerning the definitions,collection,and interpretation of data regarding EOS surgery complications is often difficult to interpret.This creates problems in the comparison,analysis,and improvement of spine surgery practice.Additionally,this observation indicates that data on the incidence of complications can be underestimated,and should be interpreted with caution.Awareness of the high rate of complications of EOS surgery is crucial,and an optimal strategy for prevention should become a priority.
Key Words:Scoliosis;Spine;Growth-friendly implant;Surgery;Complications;Treatment
INTRODUCTION
Early-onset scoliosis(EOS)is defined as curvature of the spine ≥ 10° in the frontal plane with onset before 10 years of age[1].EOS is not a diagnosis,but can rather be defined as the age of onset of a coronal plane spinal deformity.As such,EOS includes spinal deformities resulting from congenital malformations,neuromuscular conditions,inherited bone dysplasias and syndromes,and,in idiopathic cases,with no underlying disorder.As EOS has such a wide variety of etiologies,its natural history varies widely,and in many cases is established at the time of the child’s diagnosis which reveals the spinal deformity[2].The natural history of untreated progressive EOS was reported on by Scott and Morgan in 1955[3].They documented the progression of curves from 30 to 100 degrees.Moreover,4 patients out of 28 died before the age of 20 years,of cardiorespiratory disease.Relentless curve progression,in the absence of treatment,results in increasing chest wall deformity.Rib rotation and curve progression produce restrictive pulmonary disease,with worsening pulmonary function,as documented by diminishing forced vital capacity and total lung volume.If left untreated,the spinal deformity produces chest wall rotation,which obliterates the space available for the lungs[4].The treatment for EOS remains a great challenge for pediatric orthopedics.The treatment goals for EOS,regardless of the diagnosis,are the same:minimizing spinal deformity while maximizing thoracic volume and pulmonary function[5].When conservative treatment is ineffective,the option is surgery[6].Different techniques have different advantages and drawbacks.Those most often used are traditional growing rods(TGR),vertical expandable prosthetic titanium ribs(VEPTR),magnetically controlled growing rods(MCGR),and the Shilla growth guidance system(SGGS).Repeated surgeries and complications are two major concerns in EOS management.The aim of the study was to review the current literature to assess the safety of EOS surgical treatment in terms of the rate of complications and unplanned surgeries.
MATERIALS AND METHODS
Literature search strategy
The systematic review was conducted according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses(PRISMA)[7](Figure 1).In January 2021,a search of three electronic medical databases(PubMed,the Cochrane Library,and Embase)was performed by three independent authors.We combined the terms:“early-onset scoliosis” OR “eos” OR “juvenile scoliosis” OR “infantile scoliosis”OR “tgr” OR “veptr” OR “MCGR” OR “Shilla” OR “growth-friendly” AND“complication”.The reference lists of all retrieved articles were reviewed for the further identification of potentially relevant studies,and assessed using the inclusion and exclusion criteria.

Figure 1 Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart of the method of selection and screening.
Selection criteria
The eligible studies for the reference review included those dealing with complications in the operative treatment of EOS.The initial screening of titles and abstracts was made using the following inclusion criteria:studies of any level of evidence,reporting clinical results,published in peer review journals,and dealing with complications in operative EOS treatment.Exclusion criteria were:studies with complications in the non-operative treatment of EOS,in vitro,or animal model studies.We also excluded all the remaining duplicates,articles dealing with other topics,and those with poor scientific methodology,or without an accessible abstract.Reference lists were also manually searched for further relevant studies.Reviews,abstracts,case reports,conference presentations,and expert opinions,were excluded.
All papers were tagged:(1)according to the system used:TGR,VEPTR,MCGR,Shilla(guided growth);(2)the number of cases as a “big group” – more than 30 cases,“medium group” – 10-29 cases,and “small group” – less than 10 cases;and(3)the time of follow-up – “short” – less than 2 years,“minimum” – more than 2 years,and“optimum” – more than 5 years.The final inclusion criteria were primarily limited to“big group” and “optimum follow-up”.During the paper extraction,no papers with VEPTR,and only one with Shilla and MCGR,were found,so that the groups’ extracted papers had to be extended with “medium group” and “minimum” follow-up.
Data extraction and criteria appraisal
Three investigators independently reviewed each article.Discrepancies between the reviewers were resolved by discussion and consensus.All data were extracted from article texts,tables,and figures,and put into tables in an Excel sheet.
Complications were categorized as wound-related,implant-related,alignmentrelated,and general(surgical or medical).Surgical procedures were classified as planned [implantations,lengthenings,final fusions(FF)],and unplanned(revisions).Implantation procedures were included as equal to the number of patients.Not-given information was calculated using specific formulas based on the known data,i.e.,the mean number of operations per patient,the number of patients,and the number of operations.Some data – especially in TGR-group patients - like the number of lengthenings and derived information – were estimated based on the mean duration between lengthenings,using formulas,i.e.,the mean duration between lengthenings,and follow-up,i.e.the number of lengthenings.The mean durations between lengthenings,if not specified,were taken as the mean value of durations between lengthenings specified in other papers.These data were marked in the table with the symbol “1”.In some papers the number of unplanned surgeries was not provided.In those cases,such complications as deep infections and implant fractures were estimated as an indication of at least one revision/unplanned surgery.Some fields were left empty when there were not enough data to estimate the value.When the data in the main text and the tables did not match,the higher value was taken.
RESULTS
Included studies
A total of 2136 articles were found.After the exclusion of duplicates,1300 articles were selected.At the end of the first screening,following the previously described selection criteria,we selected 615 articles eligible for full-text reading.Ultimately,after full-text reading and reference-list checks,we selectedn= 40 articles,following previously adopted criteria.A PRISMA flowchart of the method of selection and screening is presented in Figure 1.The included articles focus on complications in the most commonly used systems – TGR(17 papers),VEPTR(13 papers),MCGR(8 papers),and Shilla(guided growth)(7 papers).Data extracted from these papers were assigned to the appropriate system.Harriset al[8],2020,in their paper analyzed the impact of patient and surgical factors on the proximal complications and revision rates of earlyonset scoliosis patients using a multicenter database.Total 353 patients met the inclusion criteria:growing rods = 318 and VEPTR = 35.Heleniuset al[9],2018,analyzed the outcomes of surgeries using growing rods in patients with severevsmoderate early-onset scoliosis.From the group of 214 patients,198 were treated with TGR and 14 with MCGR.As in the main texts,the data were not separated out,so we included them in the TGR group,as the vast majority were treated with this system.Papers by Akbarniaet al[10],Bachabiet al[11],Haapalaet al[12],Andraset al[13],and Luhmannet al[14],dealt with comparisons between TGR and MCGR,TGR,and VEPTR,Shilla and MCGR,and TGR and Shilla,respectively,so they appear in the table for the applicable system.The demographic findings of the included articles are summarized in Table 1.
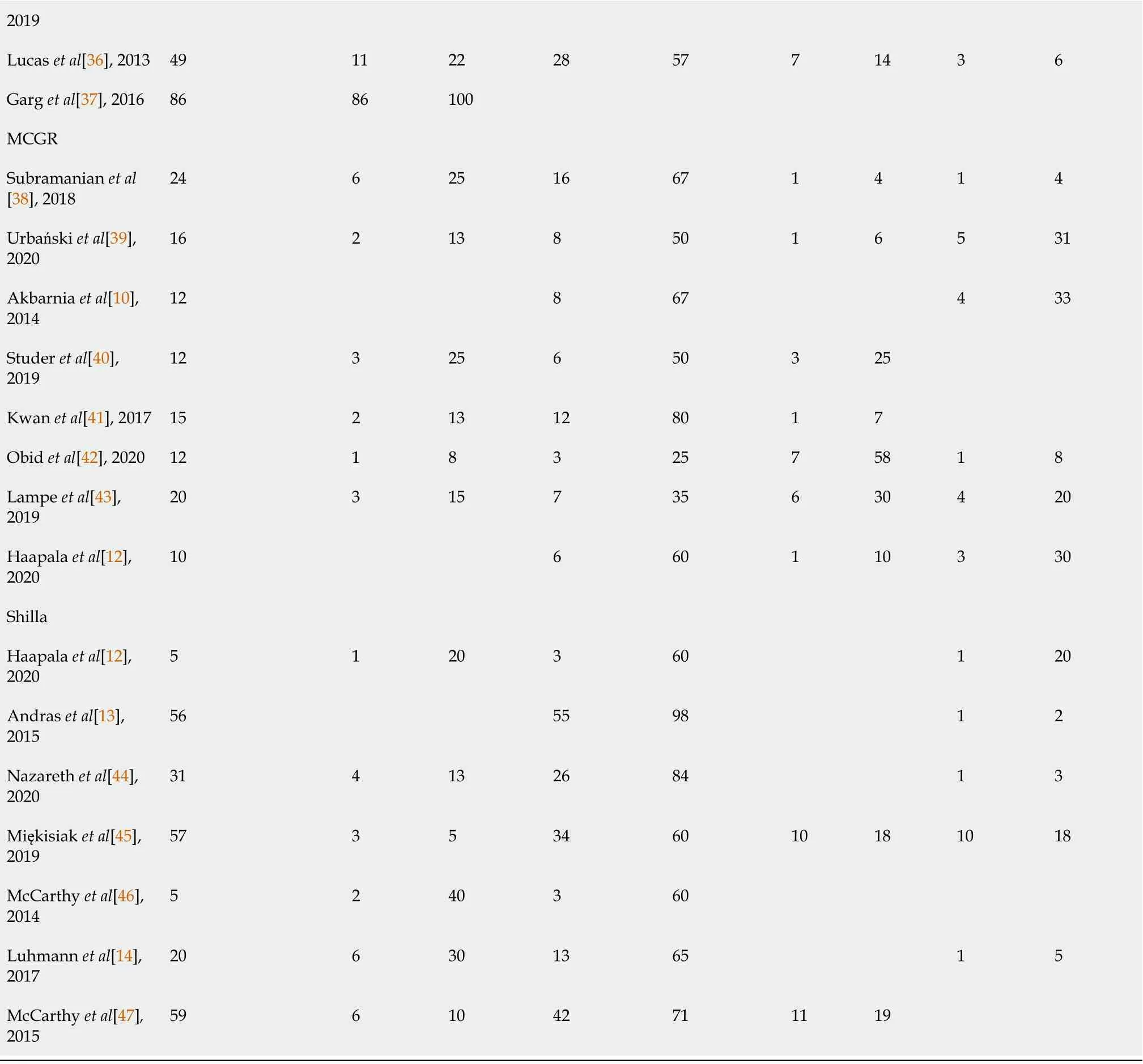
Tables 2-5 present the number of surgical procedures(planned and unplanned).The number of patients is re-listed for easier reference to the remaining data.As the quantitative data depends on the number of analyzed patients,the second part of the table presents the percentage data.It shows the percentage of unplanned surgeries,the percentage of unplanned surgeries to all surgeries,the percentage of unplanned surgeries to patients with at least one complication,and the ratio of planned to unplanned surgeries.Eight papers were excluded from these tables,as there were no data on unplanned surgeries.Some fields were left empty if there were insufficient data.From the 40 analyzed papers 12 described all 4 complications(wound and implant-related,alignment,and medical/surgical).These data are marked in the table with the symbol “2”.In the others,some of these complications were not described.Itprobably means that the number of unplanned surgeries was understated.

Table 1 Demographic data from the reviewed articles

[11],2020 20 Crews et al[27],2018 151 16/6 7.1 3+nd nd Only SSIs following VEPTR implant or revision surgeries were identified 21 Murphy et al[28],2016 25 12/13 5.7 4.5 Congenital(n = 25)nd W,I,M 22 Berger-Groch et al[29],2020 13 7/6 2.2 7.6 Congenital(n = 13)nd W,I,M 23 Hasler et al[30],2010 23 8/15 6.5 3.6 Early onset idiopathic scoliosis(n =1),neuromuscular(n = 11),postthoracotomy scoliosis(n = 2),Sprengel deformity(n = 1),hyperkyphosis(n = 2),myopathy(n= 1),syndromic(n = 5)nd W,I,A,M 24 Latalski et al[31],2011 12 nd 5.25 2.5 Congenital(n = 3),neuromuscular(n = 9)0 W,I,A,M 25 Hell et al[32],2005 15 8/7 6 nd Congenital(n = 9),neuromuscular(n = 6)0 W,I,M 26 Garg et al[33],2014 103 57/46 5.3 Neuromuscular(n = 30),congenital(n = 44),syndromic(n = 18),idiopathic(n = 11)Only wound complications following VEPTR implant or revision surgeries were identified 27 Waldhausen et al[34],2016 65 nd 6.9 6.9 Congenital(n = 23),neuromuscular(n = 12),syndromic(n = 14),idiopathic(n = 2),other(n = 14)28 W,I,M 28 Striano et al[35],2019 166 6.81 Neuromuscular(n = 61),syndromic(n = 38),congenital(n = 64),idiopathic(n = 3)nd Only wound complications following VEPTR implant or revision surgeries were identified 29 Lucas et al[36],2013 54 21/33 7 2.0 Neuromuscular(n = 19),congenital(n = 30),syndromic(n = 7),idiopathic(n = 3)nd W,I,A,M 30 Garg et al[37],2016 38 22/16 5.51 4.1 Neuromuscular(n = 18),congenital(n = 13),syndromic(n = 5),idiopathic(n = 2)nd Only wound complications following VEPTR implant or revision surgeries were identified 31 Subramanian et al[38],2018 MCGR 31 15/16 7.7 3.9 Neuromuscular(n = 4),syndromic(n = 19),idiopathic(n = 6),congenital(n = 2)nd W,I,A,M 32 Urbański et al[39],2020 47 14/18 8.8 1-2.5 Neuromuscular(n = 10),syndromic(n = 11),idiopathic(n = 20),congenital(n = 6)0 W,I,A,M 33 Akbarnia et al[10],2014 12 5/7 6.8 2.5 Neuromuscular(n = 4),syndromic(n = 4),idiopathic(n = 3),congenital(n = 1)nd I,M 34 Studer et al[40],2019 30 10/20 9.4 2.1 Congenital(n = 11),neuromuscular(n = 10),syndromic(n = 4),idiopathic(n = 5)nd W,I,A 35 Kwan et al[41],2017 30 11/19 7.3 3.0 Syndromal(n = 8),idiopathic(n =8),congenital(n = 6),neuromuscular(n = 8)5 W,I,A,36 Obid et al[42],2020 22 4/18 9.5 4.0 Idiopathic(n = 14),neurofbromatosis(n = 2),neuromuscular and syndromic(n =6)9 W,I,A,M 37 Lampe et al[43],2019 24 7/17 10.5 3.5 Syndromal(n = 4),idiopathic(n =9),congenital(n = 1),neuromuscular(n = 10)nd W,I,A,M

Type of complications:Wound(W),implant-related(I),alignment(A),and medical/surgical complications(M).FF:Final fusions;GGS:Growth guidance system;VEPTR:Vertical expandable prosthetic titanium ribs;TGR:Traditional growing rods;MCGR:Magnetically controlled growing rods.
Excluded from these tables were papers in which the number of unplanned surgeries was not specified,and were not calculated;some cases referred to final fusion,but it was not specified when,so the total number based on the duration between lengthenings was not possible to estimate.
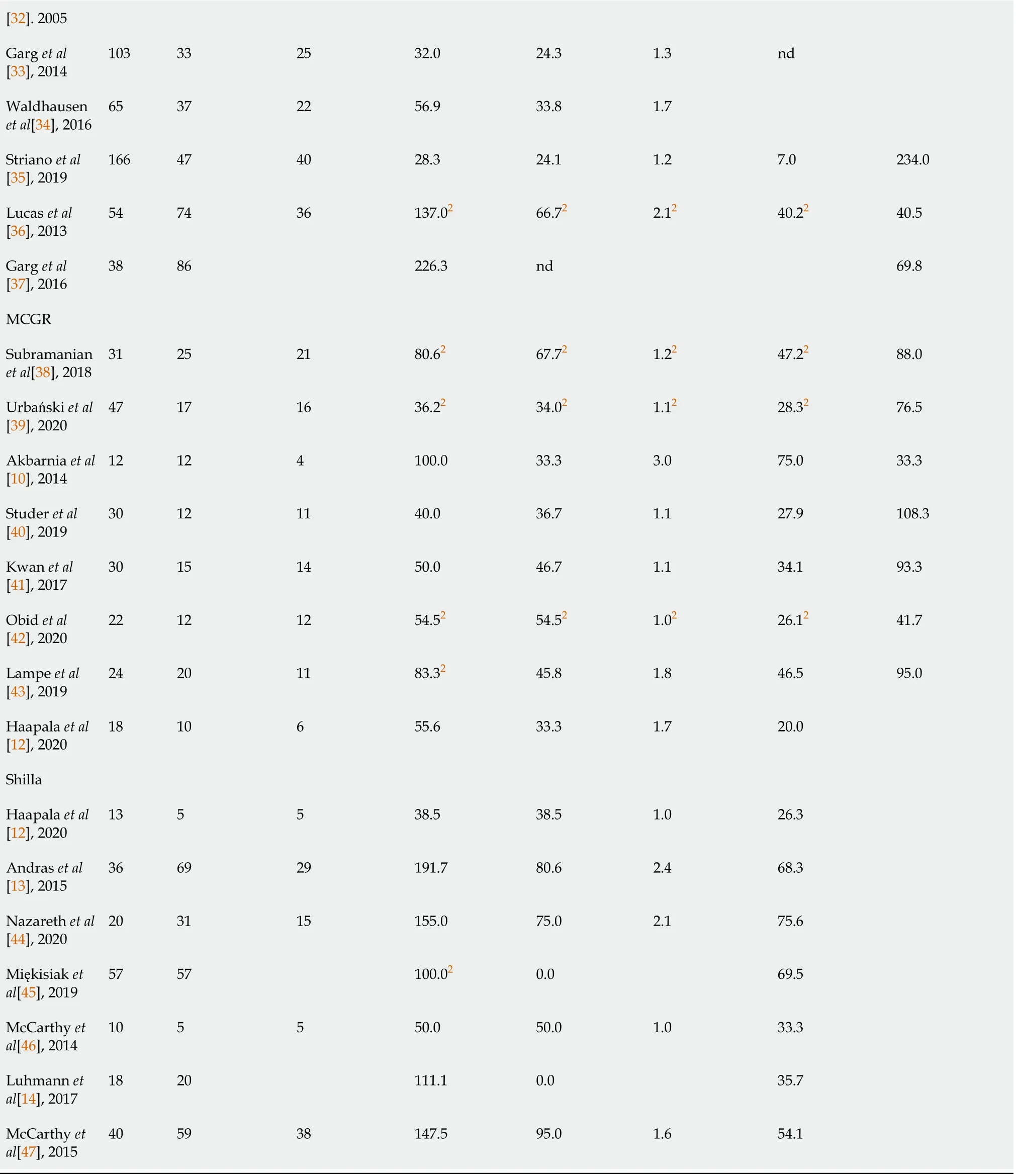
Unplanned surgeries are due to complications which cannot be resolved conservatively.The total number of complications is much higher.Table 6 presents the total number of complications,the number of patients with a minimum of one complication,the percentage of complications in all patients,the percentage of patients with a minimum of one complication,the number of complications in complicated patients,the complication rate per surgical procedure in percentage terms,and the percentage complications requiring surgical procedures.Some cells in the table are empty because of insufficient data in the corresponding papers.
In Table 7 the total number of complications are divided into wound-related,implant-related,alignment,and surgical/medical-related.Only 12 out of 40 papers include analyses of all these types.The paper by Johnstonet al[25],2013,did not differentiate the types of complications,so this reference was excluded from Table 7.
Smithet al[48] published in 2015 a New Classification System to Report Complications in Growing Spine Surgery,and only 4 out of 23 papers published in 2016 used this system(Table 8).

Table 2 The number of planned and unplanned surgical procedures in the traditional growing rods group

Table 3 The number of planned and unplanned surgical procedures in the vertical expandable prosthetic titanium ribs group
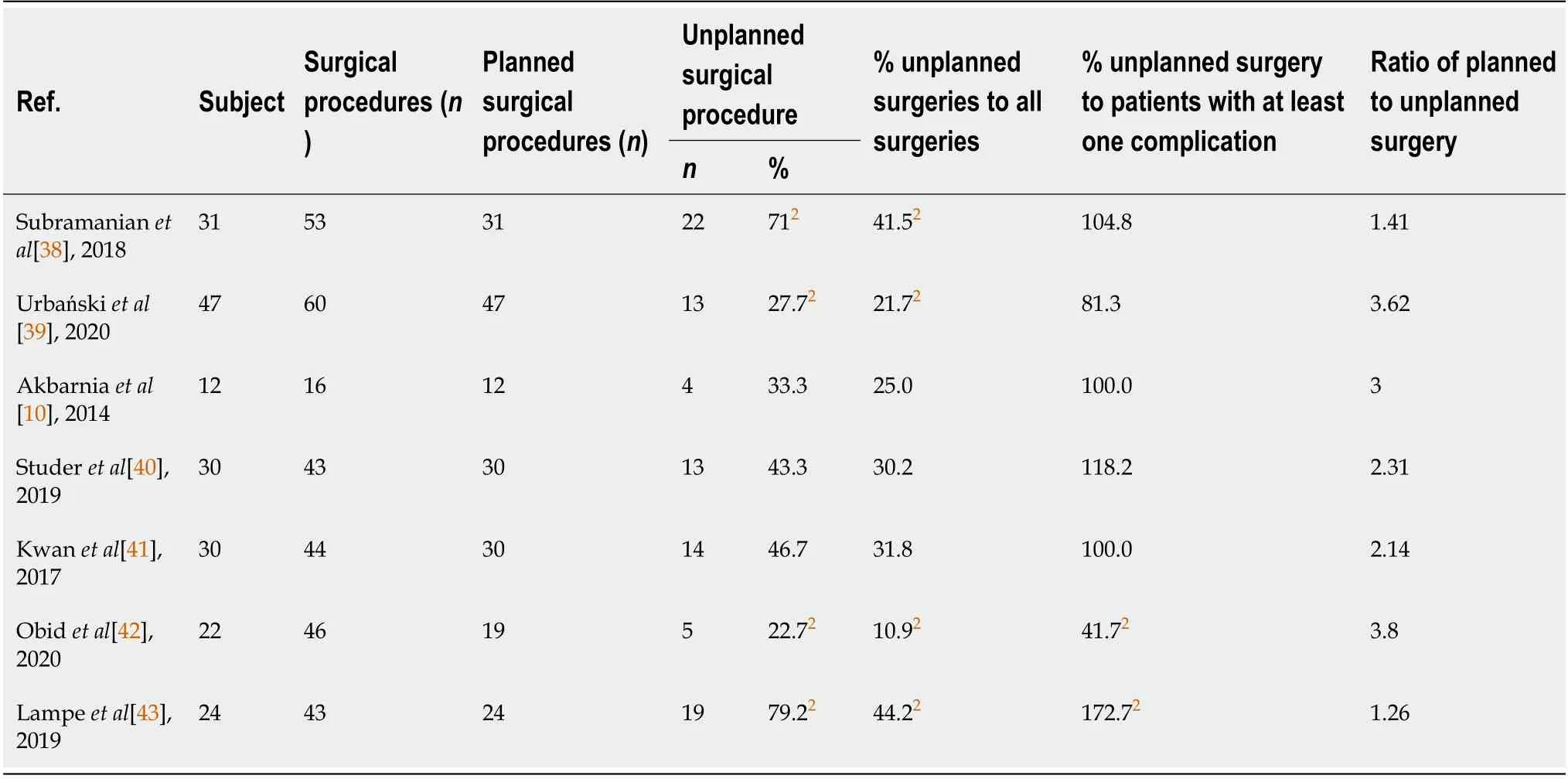
Table 4 The number of planned and unplanned surgical procedures in the magnetically controlled growing rods group

Table 5 The number of planned and unplanned surgical procedures in guided growth group – the Shilla and growth guidance system groups
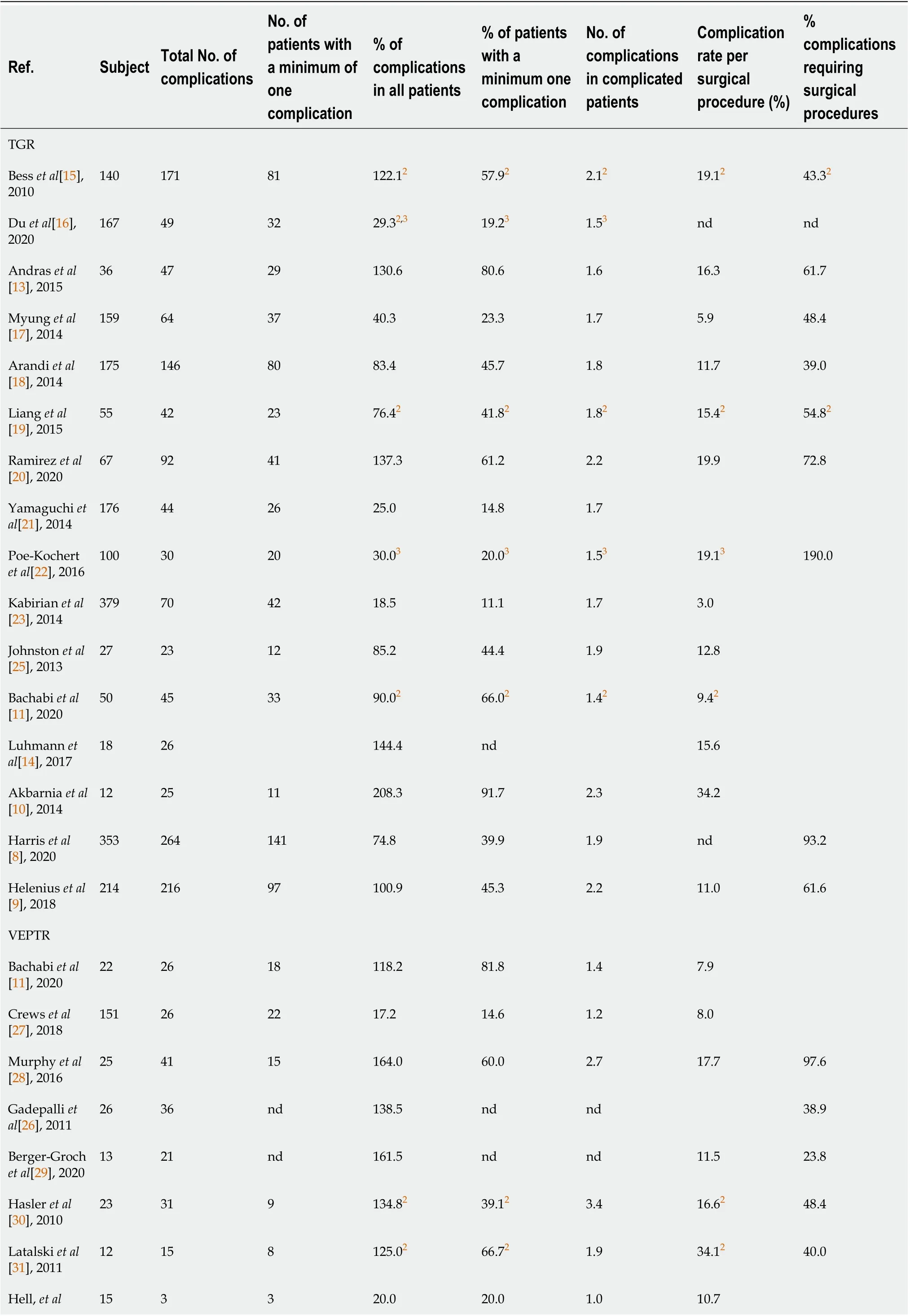
Table 6 Number of complications analyzed in extracted papers
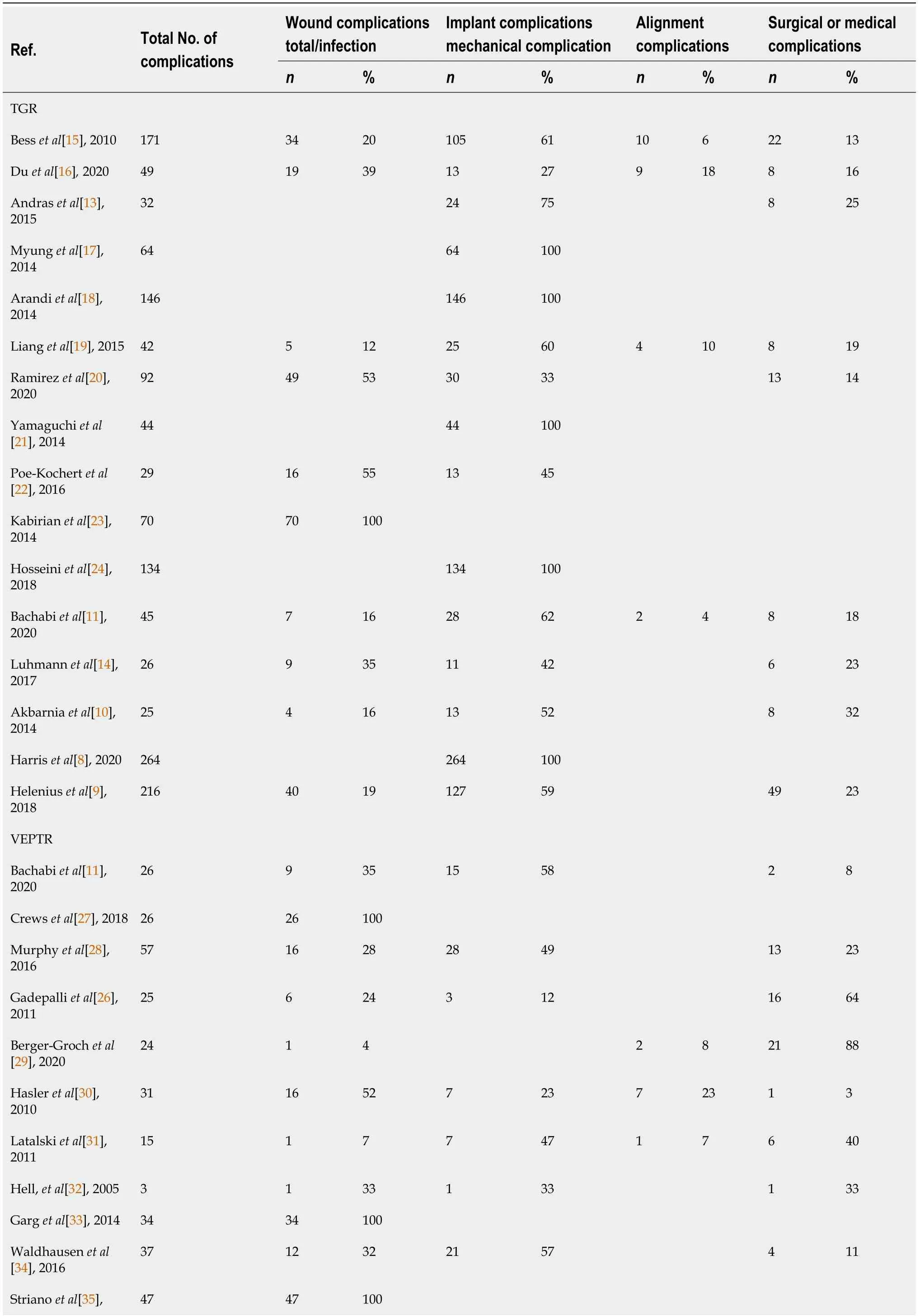
Table 7 Total number of complications divided into wound-related,implant-related,alignment and surgical/medical related
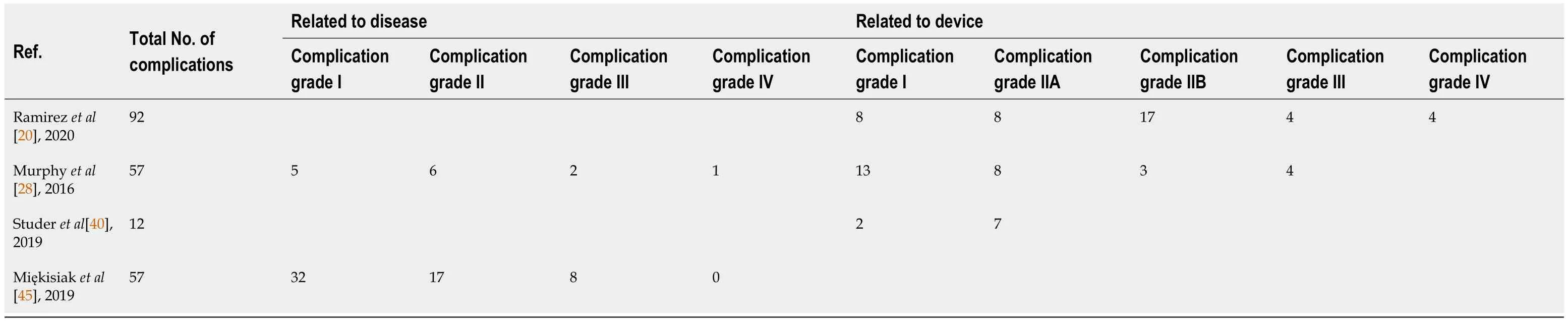
Table 8 Complication grades according to Smith
DISCUSSION
Currently there is great interest in the concept of the continued growth of the spine and chest while treating spinal deformity in EOS patients.The risk of complications is inherent in correction surgeries,regardless of etiology.Many studies agree that in the case of neuromuscular scoliosis the probability of a complication is 35%,while for EOS the probability increases to 48%[49].Watanabeet al[50] identified risk factors for complications in the treatment of early-onset scoliosis using the dual growing rod technique.Postoperative complications occurred after 119 out of 538 procedures(22%)and affected 50 patients(57%).Complications mostly included implant-related failures(72%),and infections(16%).The authors suggested that independent risk factors for postoperative complications included an increase of every 20° in the proximal thoracic Cobb angle,an increase of every 20° in the thoracic kyphosis angle,and 6 or more rod-lengthening procedures.According to Besset al[15],the patients’ early age when carrying out the index surgery influenced the incidence of complications,but Watanabe did not confirm this.He believed that a patient’s being young at the time of the index surgery significantly reduced the risk of the child’s developing a significant deformity,the degree of which at the start of the treatment significantly affects the risk of its course.However,one should be aware of the inverse relationship between the age of the index surgery and the number of lengthenings in distraction-based methods[4].
Bess,and the Growing Spine Study Group,stated in publications that there was a 24% complication rate each time a growing-rod construct was surgically lengthened,and a 13% decrease in complications for each additional year of age at the time of the initial growing rod implantation[15].Rod implantation below age 7 years,increasing kyphosis,and more severe major curve magnitude,have been shown to correlate with a higher rate of complications overall[51].
Surgical difficulties,as well as the potentially harmful effect of repeated anesthesia,have led to the adoption of magnetically controlled growing rods,and guided growth systems like Shilla.However,problems with the loss of fixation and failure of the implants in some cases persist[10,47].Some authors have pointed out an additional problem connected with metal debris which appears in the serum and surrounding tissues[52].Although it does not directly affect the outcome of the treatment,it is worth considering this occurrence as undesirable/a complication.
The most important issue is that authors define complications in different ways.In Andraset al[13],major complications are defined as any neurological injury and anyissue requiring surgery for implant revision or infection.In Ramirezet al[20],complications are defined as any change from the normal postoperative course which occurred from the time of the surgery until the most recent follow-up visit.In McCarthyet al[47],2015,complications are defined as any problem requiring a return to the operating room,so all returns to the operating room were considered unanticipated.Some authors report major complications and some report the whole range of general complications.
For this study,complications were categorized as wound,implant,alignment,or general [surgical or medical].Wound problems were classified as either superficial or deep infections,and other wound-related problems,such as painful scars.Implant complications included rod breakage,failure of foundation fixation such as hook or screw pullout,and implant prominence.Alignment complications included junctional kyphosis(proximal or distal),curve progression above or below the instrumented levels,and curve progression after definitive fusion.General complications included,but were not limited to,dural tears,hematomas,and postoperative cardiopulmonary and gastrointestinal complications.Unfortunately,not all authors evaluated all these kinds of complications together – 4 out of 17 in TGR,3 out of 13 in VEPTR,4 out of 8 in MCGR,and 1 out of 7 in Shilla.Only 16 out of 44 papers(36%)referred to alignment complication in the evaluation – mostly in MCGR(88%),and conversely to VEPTR(23%).Five papers(11%)(TGR)described only implant-related complications,and 5 only wound-related(4 VEPTR and 1 TGR).The most frequently evaluated set of complications were wound,implant,and medical-related – 13 papers(30% of the papers).The original idea of the paper was to evaluate the number of procedures used to treat complications categorized as either planned or unplanned.Planned procedures were defined as procedures which were scheduled as part of the routine growing-rodtreatment protocol.Unplanned procedures were defined as unscheduled surgical procedures performed to manage a complication.Unfortunately,there was no division into such treatments,so the data were simplified and surgical procedures were classified as planned(implantations,lengthenings,final fusions)and unplanned(revisions).In that case,the number of complications requiring surgical treatment could have been greater,as some of them could have been repaired during the planned lengthening procedure.Only 10 papers(23%)(2 TGR,3 VEPTR,4 MAGEC,1 Shilla)included data with unplanned surgeries,and all described complications concurrently.FF significantly influenced the number of surgeries.Despite the number of patients with FFs being known,there were no data about the time of the FFs – so estimated data based on the mean follow-up times and durations between lengthening procedures were understated.Deleting these references from the statements in question leaves 6 papers with no TGR patients.Adding Smith's classification for evaluation as a criterion further reduces the number of papers to only one.That is why the analysis had to be simplified.
TGRs constitute the most commonly applied technique,and are considered the gold standard for EOS with long curves[53].In the reviewed papers,the complication rate per patient of the growing rod technique was very high and ranged from 19% to 208%(median 84%).Interestingly,Akbarniaet al[10],presented a complication rate of 208%(wound,implant-related and medical)in only 12 patients,whereas the rate for deep infections was 19% in 379 cases[23].Comparing only implant-related complications,this parameter varied from 25%[21] to 40%[17],to 83%[18] – the authors analyzed a similar group of approximately 160 patients.The complication rate per surgical procedure varied from 3% to 34%(median 15%).There were two complications in complication-affected patients.In the analyzed papers,an average of 946 surgical procedures were performed.The incidence of unplanned surgeries in all patients varied from 19% to 144%(median 53%).The percentage of unplanned surgeries for all surgeries was 8%(3%-36%).The ratio of planned to unplanned surgeries was 11.6%(1.8%-33.9%).The most frequent complications were implant-related(61%)andwound-related(27%),while medical complications and alignments accounted for 19%and 8%,respectively.The most concerning problem related to TGRs is the high complication rate.The risks for implant failure,infections,and wound healing problems are significantly increased as a consequence of the repeated lengthening procedures and an unfused spine.If rod breakage or screw displacement occurs,revision surgeries are indicated to change the rod or extend the instrumented segments.Additionally,repeated general anesthesia can pose a threat to mental health.Adequate informed consent and close follow-ups are necessary.
2The values of the % of unplanned surgeries in which all four complications were analyzed in the paper.3Corresponds to the papers in which all patients were after final fusion.TGR:Traditional growing rods;VEPTR:Vertical expandable prosthetic titanium ribs;MCGR:Magnetically controlled growing rods.
TGR:Traditional growing rods;VEPTR:Vertical expandable prosthetic titanium ribs;MCGR:Magnetically controlled growing rods.
VEPTR was developed for patients with thoracic insufficiency syndrome(TIS),but it is sometimes indicated for individuals with EOS who are at risk of secondary TIS[54,55].The complication rate per patient was as high as 125%(17%-226%)with a 9% rate per surgical procedure(7%-18%).Such a discrepancy is very confusing.Garget al[37]identified only wound complications following VEPTR implant or revision surgeries.If so,adding implant,alignment,and medical-related complications,the final percentage of complications should be expected at a much higher level.On the other hand,Crewset al[27] analyzed wound,implant,and general complications at the level of 17%.The most frequent complications were implant-related 48%,and woundrelated 33%,while medical complications and alignments accounted for 23% and 11%.respectively.which limits their applications.In the analyzed papers,an average of 251 surgical procedures were performed.The percentage of unplanned surgeries in all patients varied from 39% to 160%(median 60%).The percentage of unplannedsurgeries to all surgeries was 14%(3%-17%).The proportion of planned to unplanned surgeries was 6%(4.7%-35.6%).
MCGRs were introduced by Takasoet al[56] in 1998 as remote-controlled growingrod spinal instrumentation.The system did not require open lengthening as TGRs did,and the effect could instead be achieved by external remote control without repeated anesthesia.The complication rate of the magnetically controlled growing rod technique per patient varied from 36% to 100%(median 55%).In this group of patients,the distribution of complications is fairly homogeneous.Only Akbarniaet al[10] described such a high level of complications while omitting wound-related and alignment problems.The complication rate per surgical procedure varied from 20% to 75%(median 31%).In the analyzed papers,an average of 44 surgical procedures were performed.The percentage of unplanned surgeries in all patients varied from 23% to 79%(median 43%).The percentage of unplanned surgeries in all surgeries was 30%(11%-34%).The ratio of planned to unplanned surgeries was 2.3(1.3-3.8).The most frequently occurring complication was implant-related – 55%,then general(25%),wound(14%),and alignment(10%).La Rosaet al[57] stated that MCGRs can prevent surgical scarring,surgical site infections,and psychological distress,which occur in patients with TGRs and VEPTR due to the multiple surgeries.The decreased rate of infections and wound healing problems in patients who received MCGRs is of great benefit to patients.However,Aslanet al[58] used psychosocial tools to compare the mental state of patients receiving MCGRs and TGRs.He affirmed that if the patient noticed benefit from the growing rods,and did not experience major complications,the non-invasiveness of the lengthening procedures did not show an advantage on the patients’ psychosocial state.Besides,although MCGRs were associated with a lower rate of infections [both deep and superficial],they were associated with a significantly increased risk of metalwork problems and unplanned revisions[59].
The Shilla technique guides spinal growth towards a normal alignment[60].The technique first corrects the apical deformity towards a neutral alignment.Then the upper and lower growth guidance portions extend into the distal and proximal areas of the curve,using special screws and caps,allowing the rod to slide with growth in a longitudinal direction.Multiple open lengthening surgeries are avoided,as in MCGRs.The complication rate was as high as 111% of the patients(39%-192%),and the complication rate per surgical procedure was 54%.Haapalaet al[12] showed the fewest complications – 39%.The remaining authors assessed the number of complications at a similar level.The most frequently appearing complications were implant-related(65%).Wound-related and alignment problems were 16% and 18%,respectively.General complications were only 5%.The percentage of unplanned surgeries in all patients varied from 15% to 181%(median 105%).The percentage of unplanned surgeries to all surgeries was 33%(11%-64%).The ratio of planned to unplanned surgeries was 1.8(0.6-8.5).Luhmannet al[14] found that the Shilla growth guidance system compared favorably with TGRs in terms of the degree of correction of the major curve,spinal length,and growth,and the maintenance of the sagittal alignment.Looking at these data the benefits are not so obvious.Similar to MCGR and TGR,the SGGS is associated with a very high rate of implant-related complications,which usually results in revision surgery.Additionally,for patients with great growth potential,the distal and proximal screws can slide off the rod,requiring the rods to be changed.
EOS surgery has a varying but high rate of complications.Based on this review of 40 papers,3249 cases,and 15037 surgical procedures,the most-frequent implant complications(total 54%),the general,wound,and alignment were 17%,15%,and 12%,respectively.These data are simplified and certainly underestimated,because of the reasons described earlier.The rate of complications might have been higher than reported,as some authors did not report every type of complication.Due to complications,54% of the patients required unplanned surgeries,which equated to 15% of all surgeries.
The long-term risks of EOS surgery have not yet been reported on in research.There is a lack of papers with homogenous cases,long-term follow-up,all revision surgeries,and complication data.
One would expect that successful treatment which encourages the growth of the spine and chest would lead to favorable outcomes in patients with early-onset idiopathic scoliosis.But it is not unambiguous with patients with,e.g.,progressive neuromuscular conditions such as congenital muscular dystrophies and spinal muscular atrophy.Surgery can effect spinal growth with expandable instrumentation,but worsening muscle weakness can negate the positive effects of growth-friendly procedures[2].Tsirikoset al[61] showed that the life expectancy of patients with cerebral palsy and other neurogenic deformities subjected to deformation correction does not change,but only an additional source of data such as the number of days in the intensive care unit after surgery,and the presence of severe preoperative thoracic hyperkyphosis,were the only factors affecting survival rates.
As highlighted by Hawes[62],the complexity of spinal surgery is reflected in the diversity of complications which might occur months or even years later.Given the time delay and difficulty in diagnosis,it is likely that some of the events are not recognized as surgical complications.Therefore,clear uniformity of definitions and the carefulness of the surgeon are important in assessing patient follow-up and treatment outcomes.
CONCLUSION
The literature concerning the definitions,collection,and interpretation of data regarding EOS surgery complications is often difficult to interpret.This causes problems in the comparison,analysis,and improvement of spine surgery practice.Additionally,this observation indicates that data on the incidence of complications can be underestimated and should be interpreted with caution.Awareness of the high rate of complications of EOS surgery is crucial,and an optimal strategy for prevention should become a priority.
ARTICLE HIGHLIGHTS
Research background
The treatment for early-onset scoliosis(EOS)remains a great challenge for pediatric orthopedics.The treatment goals for EOS,regardless of the diagnosis,are the same:minimizing spinal deformity while maximizing thoracic volume and pulmonary function.When conservative treatment is ineffective,the option is surgery.
Research motivation
Different surgical techniques have different advantages and drawbacks.Those most often used are traditional growing rods(TGR),vertical expandable prosthetic titanium ribs(VEPTR),magnetically controlled growing rods(MCGR),and the Shilla growth guidance system(SGGS).Repeated surgeries and complications are two major concerns in EOS management.
Research objectives
The aim of the study was to review the current literature to assess the safety of EOS surgical treatment in terms of the rate of complications and unplanned surgeries.
Research methods
The systematic review was conducted according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses.In January 2021,a search of three electronic medical databases(PubMed,the Cochrane Library,and Embase)was performed by three independent authors.We combined the terms:“early-onset scoliosis” OR “eos” OR “juvenile scoliosis” OR “infantile scoliosis” OR “tgr” OR“veptr” OR “MCGR” OR “Shilla” OR “growth-friendly” AND “complication”.
Research results
EOS surgery has a varying but high rate of complications.The most frequent complications were categorized as implant,general,wound and alignment.The rate of complications might have been even higher than reported,as some authors do not report all types of complications.
Research conclusions
The literature concerning the definitions,collection,and interpretation of data regarding EOS surgery complications is often difficult to interpret.This creates problems in the comparison,analysis,and improvement of spine surgery practice.Awareness of the high rate of complications of EOS surgery is crucial,and an optimal strategy for prevention should become a priority.
Research perspectives
This observation indicates that data on the incidence of complications can be underestimated,and should be interpreted with caution.Further studies are needed to confirm the study results,especially concerning longitudinal data.
杂志排行
World Journal of Orthopedics的其它文章
- International recognition of the Ilizarov bone reconstruction techniques:Current practice and research(dedicated to 100th birthday of G.A.Ilizarov)
- Calcar-guided short-stem total hip arthroplasty:Will it be the future standard? Review and perspectives
- Fibula pro-tibia vs standard locking plate fixation in an ankle fracture saw bone model
- Thromboelastography in elective total hip arthroplasty
- Performance of alpha-defensin lateral flow test after synovial fluid centrifugation for diagnosis of periprosthetic knee infection
- Limb lengthening with PRECICE magnetic nail in pediatric patients:A systematic review