Intestinal metastasis from breast cancer: Presentation, treatment and survival from a systematic literature review
2021-08-02ElenaBolzacchiniOlgaNigroDavideInversiniMonicaGiordanoGiovanniMaconi
Elena Bolzacchini, Olga Nigro, Davide Inversini, Monica Giordano, Giovanni Maconi
Elena Bolzacchini, Department of Oncology, Ospedale Sant' Anna, ASST Lariana, Como 22100,Italy, Department of Medicine and Surgery, University of Insubria, Varese 21100, Italy
Olga Nigro, Department of Oncology, Ospedale di Circolo ASST-Sette Laghi, Varese 21100,Italy
Davide Inversini, Department of General Surgery, Ospedale Sant' Antonio Abate, ASST Lariana,Cantu' 22100, Italy.
Monica Giordano, Department of Oncology, Ospedale Sant' Anna, ASST Lariana, Como 22100,Italy
Giovanni Maconi, Department of Biomedical and Clinical Sciences, Gastroenterology Unit,"Luigi Sacco" University Hospital, Milano 20157, Italy
Abstract BACKGROUND Intestinal metastases from breast cancer (BC) arerare; available data depend mainly on case reports and case series.AIM To conduct a review of the literature regarding presentation, diagnosis, treatment and survival of patients with intestinal metastasis from BC.METHODS We identified all articles that described patients with intestinal metastasis (from duodenum to anum) from BC using MEDLINE (1975 to 2020) and EMBASE (1975 to 2020) electronic databases.RESULTS We found 96 cases of intestinal metastasis of BC. Metastasization involved large bowel (cecum, colon, sigmoid, rectum) (51%), small bowel (duodenum, jejunum,ileum) (49%), and anum (< 1%). Median age of patients was 61-years. The most frequent histology was infiltrating lobular carcinoma followed by infiltrating ductal carcinoma. In more than half of patients, the diagnosis was made after the diagnosis of BC (median: 7.2 years) and in many cases of emergency, for bowel obstruction, bleeding or perforation. Diagnosis was achieved through endoscopy,radiological examination or both. In most of the cases, patients underwent surgery with or without systemic therapies. Survival of patients included in this review was available in less than 50% of patients and showed an overall median of 12 mo since diagnosis of the intestinal metastasis.CONCLUSION Although, intestinal metastases of BC are considered a rare condition, clinicians should consider the possibility of intestinal involvement in case of abdominal symptoms even in acute setting and many years after the diagnosis of BC,especially in patients with a histology of lobular carcinoma.
Key Words: Breast cancer; Intestinal metastasis; Diagnosis; Treatment; Small bowel; Large bowel
INTRODUCTION
Breast cancer (BC) is the most common malignancy among women and a leading cause of cancer-related deaths[1,2]. In case of early diagnosis and application of new therapies, approximately 30% of patients are still at risk of developing distant metastasis, while 5% of the cases are metastatic at diagnosis[3]. The most common metastatic sites of BC are bones, lungs, liver and brain[4]. Gastrointestinal (GI) tract metastases are uncommon, detected in less than 5% of all BC patients[5]. Distinguishing primary and secondary GI cancer tumors can be clinically challenging. In particular, intestinal metastases from BC are rare, and related symptoms are not specific and often attributed to oncologic treatment, the main problem is to recognize them promptly and discriminate peritoneal carcinomatosis from other GI diseases to avoid any diagnostic delay and establish an effective treatment as soon as possible to improve survival of patients[6].
Despite well-known potential of intestinal metastatization of the BC, available data rely mainly on case reports and case series. Therefore, we report a literature review on presentation, diagnosis, treatment and survival of patients with intestinal metastasis from BC.
MATERIALS AND METHODS
We identified all articles that described patients with intestinal metastasis (from duodenum to anum) from breast cancer using MEDLINE (1975 to 2020) and EMBASE(1975 to 2020) electronic databases.
The search strategy was developed with a language restriction (only English texts)and literature search performed by applying the words: “Breast cancer”,“gastrointestinal metastasis”, “gastrointestinal tract”, “intestine, bowel”, “duodenum”,“jejunum, cecum”, “ileum”, “small bowel”, “large bowel”, “colon”, “sigma”, “sigmoid tract”, “rectum”, “anus” using the following string [(breast) AND (cancer or tumor or neoplasm) AND [duodenal neoplasms (secondary) OR jejunal neoplasms (secondary)OR cecal neoplasms (secondary) OR ileal neoplasm (secondary), OR small bowel neoplasm (secondary), OR colorectal neoplasms (secondary) OR sigma OR sigmoid neoplasm (secondary) OR anal neoplasms (secondary) NOT review], and filtering them for English studies and for humans studies (Figure 1).

Figure 1 Study identification and selection process.
The research of the literature was performed independently by two investigators(Nigro O and Bolzacchini E).
Studies were included if they met the following criteria: (1) Patients ≥ 18 years; (2)Patients with intestinal metastasis from breast cancer; and (3) Diagnosis of intestinal metastasis was objectively confirmed (histology).
Two investigators (Nigro O and Bolzacchini E) independently extracted data on study (year of publication, study centre), patients’ characteristics (number of subjects studied, age, gender), tumour’s characteristics (histology, time and site of metastatization), clinical presentation (main symptoms reported) as well as treatment and survival from the diagnosis of intestinal metastasis. We tried to contact the authors of the articles with missing survival data.
RESULTS
We identified 96 cases (86 articles) of intestinal metastases from BC[5-91]. Metastases are described in all parts of the intestinal tract, from the duodenum to the anum. Site of metastasis, presentation symptoms, treatment and clinical data are reported in Table 1.
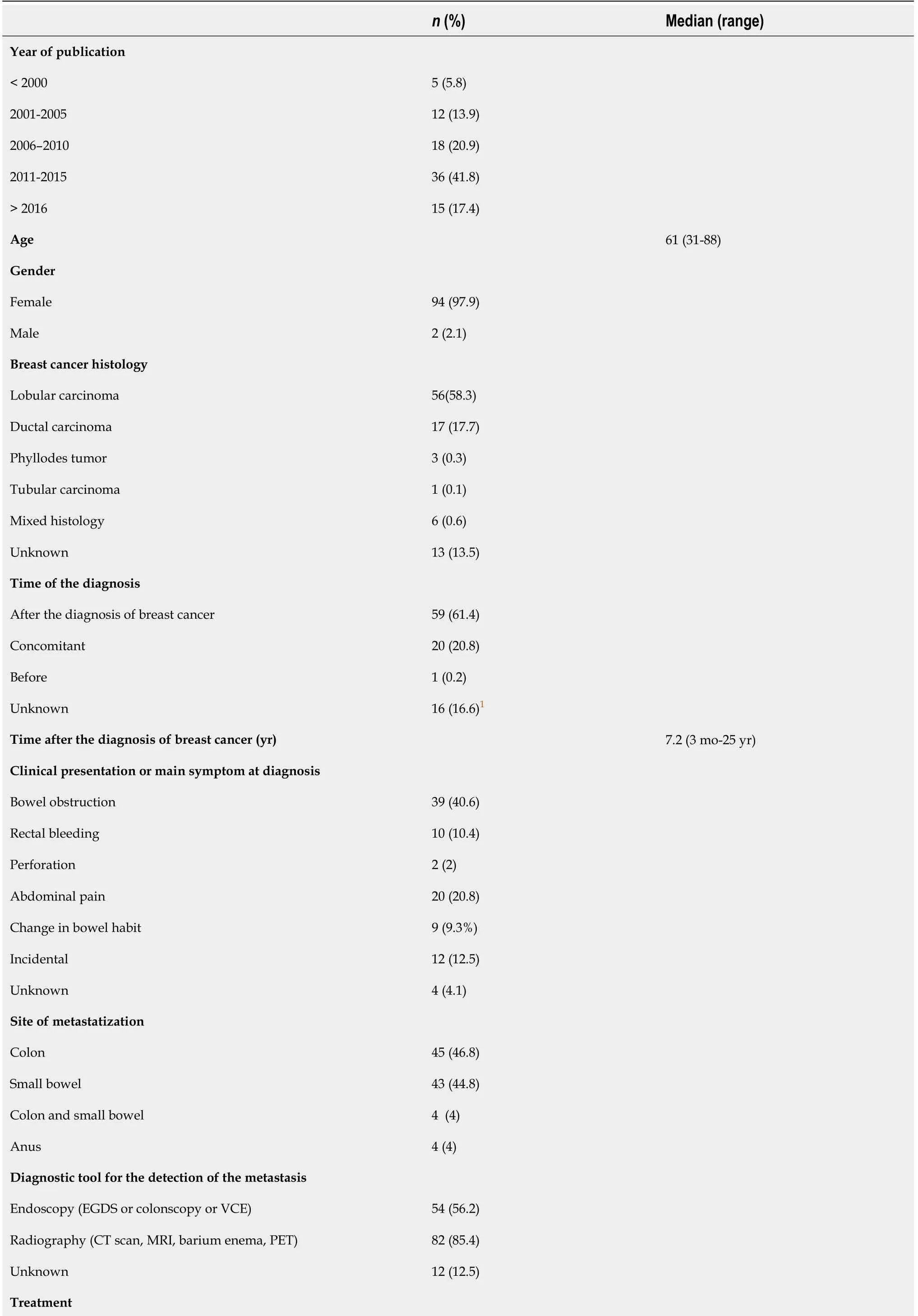
Table 1 Demographic and clinical data of patients with intestinal metastasis from breast cancer

1In one case the primary tumor remained occult.2Available for 46 patients. EGDS: Esophago-gastro-duodenoscopy; VCE: Video capsule endoscopy; CT: Computed tomography; MRI: Magnetic resonance imaging; PET: Positron emission tomography.
Metastatization arose in large bowel (cecum, colon, sigmoid, rectum) (50/96; 52%),small bowel (duodenum, jejunum, ileum) (47/96; 49%), and anum (4/96, < 1%). Four patients presented multiple sites of intestinal metastases (small and large bowel); in three patients, gastric metastasis was also found, while peritoneum was also involved in six patients. Median age of patients was 61-years (between 31 and 88-years-old);only two patients were males. Histology comprehended lobular carcinoma (56/96;58%), ductal carcinoma (17/96, 18%), phyllodes tumor (3), tubular carcinoma (1), or mixed histology (6).; 13/96 histologies were unknown. Intestinal involvement was diagnosed after the diagnosis of BC in 59/96 patients (median time; 7.2 years; range: 3 mo-25 years); the diagnosis was concomitant in 20/96 patients, in one case, the diagnosis of BC was made months after the metastatic involvement of the intestine and in another case, BC remained occult. In many cases, the diagnosis was made in emergency, for bowel obstruction (39 patients, 40.6%), bleeding (10 patients, 10.4%)and perforation (2 patients, 2%). Other patients complained of symptoms such as pain,changes in bowel habits, and in few patients, the diagnosis was incidental.
Diagnosis was achieved through endoscopy (esophagogastroduodenoscopy,colonoscopy or video capsule enteroscopy) in 54/96 cases (56.2%), radiological examination [computed tomography (CT), magnetic resonance imaging, barium enema or positron emission tomography (PET)] in 82/96 cases (85.4%) or both endoscopy and radiological imaging in 44/96 cases (45%).
In most of the cases, patients underwent surgery (69/96; 72%), with or without systemic therapies. The other patients started or continued medical therapy (18/96,18.7%) such as hormone therapy and chemotherapy.
Specifically, 40 patients received hormone therapy (one patient aromatase inhibitor plus palbociclib), 38 patients received chemotherapy and 9 patients received both.Chemotherapy prescribed included monotherapy agents such as taxane-based chemotherapy (paclitaxel, docetaxel), anthracycline-based and oral fluoropyrimidine.Moreover, chemotherapy regimen was not specified in many reports.
Median overall survival of patients included in this review was available for 46/96 pts (< 50%); median survival estimated from the available data was around 12 mo.
DISCUSSION
Intestinal metastases from BC are rare. Jainet al[92] in a large study examined 1238 patients with operable BC and identified metastatic sites. They found that infiltrating ductal carcinoma recurred more often in the lung, pleura and bone, while infiltrating lobular carcinoma metastasized more often to bone marrow and peritoneum. Bone involvement as the initial presentation of distant metastatic disease occurred in over 50% of the women with infiltrating lobular carcinoma, significantly more often than inthose with ductal infiltrating carcinoma (34%;P< 0.01). Survival was similar for the 2 groups.
Interestingly, metastatic disease to the extrahepatic GI tract from breast carcinoma usually originates from the lobular carcinoma subtype, which accounts for only 8% to 14% of all breast adenocarcinomas, rather than the more common invasive ductal carcinoma[93]. This could be related to a particular tropism of lobular cells. In a large autopsy series[94] of 337 patients who died of BC, GI metastasis presented an incidence of 16.4 % and only 20% of these patients complained of having symptoms.However, in this autopsy series, gastric and intestinal metastases were grouped,preventing an accurate estimation of the latter.
It has been well documented that recurrence in lobular BC can occur several years after the initial diagnosis of BC, even in early stage tumors. Recurrences of lobular BC have been reported up to 30 years from the initial time of diagnosis[95]. Accurate incidence of GI metastasis is hard to establish.
Symptoms depending on metastatic sites are generally not specific and may include abdominal pain, dyspepsia and nausea, acute symptoms such as bowel occlusion and GI bleeding may occur in most cases. Time interval between primary BC cases is wide,mostly years after the first diagnosis but rarely even before.
Endoscopy, radiological exams and histological evaluation are necessary to differentiate primary GI carcinoma from metastatic GI lesion of BC[32].
Endoscopic findings vary significantly and may range from ulcers, mucosal thickening or friability, linitisplastica-like inflammation, stenosis and polyps, to obstructing mass[24]. Barium studies reveal stricture or linitisplastica[41].
CT is indicated for characterizing the extension of the mass and for the re-staging[96]. Recently, Laoutlievet al[9] suggested that 18F-fluorodeoxyglucose PET should be considered.
Markers are generally not useful nor specific for the diagnosis of intestinal metastasis, but in an interesting case report by Santiniet al[8] an increase in CA19.9 was used to diagnose ileocaecal valve metastasis from BC.
Differentiation of breast metastasis from other GI primaries can be difficult and immunohistochemistry is crucial to establishing the accurate diagnosis. Commonly used markers include estrogen receptors and progesterone receptors, CK7, CK20. A CK7-/CK20+ profile favors a large bowel primary, while CK7+/CK20- favors a metastasis[74].
GCDFP-15 and mammaglobin positivity was found to be sensitive and specific markers were used to differentiate a malignant lesion as a metastatic breast carcinoma,with an excellent correlation between GCDFP-15 and mammaglobin positivity and the origin of a metastatic BC[97,98]. It is very important to clarify the diagnosis since the treatment strategy for GI metastasis of BC and for primary GI carcinoma is totally different[99].
However, data on treatment are fragmentary. Surgical treatment, often palliative,should be reserved in case of emergencies (perforation, obstruction and hemorrhage),patients with isolated lesions, and selected cases in which tumor debunking could improve clinical outcome. Medical treatment such as chemotherapy, hormone therapy and anti HER2 therapy may be indicated depending on the biologic features of the primary disease and on prior therapy[100] and it is recommended as first-line treatment in case of multiple metastatic involvement. These therapies can be extremely effective and may help to avoid unnecessary surgery[10]. Radiotherapy is an option in case of anal localization[26,57] and in case of brain metastases[33] or bone metastases.
Long term outcome remains uncertain due to data scarcity and for the rareness of the condition. Nevertheless, some cases of longer survival were also reported[6,30].Considering the available data, intestinal involvement seems prognostically unfavorable; in fact, progression free survival and overall survival of patients affected with metastatic BC have improved over the years thanks to the new treatment options.
We are aware that this review includes a selection bias as it does not rely on consecutive series of patients, but on many selected single case reports, published in English over a wide lag time (30 years). Therefore, many cases may not have been reported, several clinical data are missing and the outcome is especially not available for many cases even though we tried to contact the authors.
We pointed out that our review includes cases published from 1975 till date and clinical presentation, diagnosis and therapy might have changed over the years with awareness and technological advancement, nuclear medicine and new therapies. In this regard, a tentative analysis to assess the influence of time on several diagnostic and prognostic variables has been performed (data not shown), but no significant difference was found.
Nevertheless, the strength of our paper is its originality and the systematic methodological approach to the literature regarding intestinal localization of metastatic BC.Several reviews have already been published regarding gastric metastasis of BC; but to the best of our knowledge this is the first regarding intestinal involvement. Our paper comprehends all the cases reported so far in English language and summarizes epidemiology, symptoms, diagnostic work-up, therapy and survival of this condition.On this note, an estimate of the problem is given to the best of its knowledge and it forms the basis for the creation of a multicentre prospective study or a registry, which is the best option to investigate this uncommon but relevant issue of BC.
CONCLUSION
Clinicians should consider the possibility of intestinal involvement in case of abdominal symptoms, especially in patients with a histology of lobular carcinoma.Adequate imaging and endoscopic procedure should be performed promptly in order to obtain histological diagnosis. Treatment strategies include surgery, chemotherapy,hormone therapy and radiotherapy. Long term prognosis remains uncertain.
A multicenter study or registry study is required.
ARTICLE HIGHLIGHTS
Research background
Intestinal metastasis from breast cancer (BC) is considered rare.
Research motivation
We conducted a review of the literature regarding intestinal metastasis from BC.
Research objectives
We conducted a review of the literature regarding presentation, diagnosis, treatment and survival of patients with intestinal metastasis from BC.
Research methods
We identified all articles that described patients with intestinal metastasis from BC using MEDLINE and EMBASE electronic databases until 2020.
Research results
We found 96 cases of intestinal metastasis of BC. Metastasization involved large bowel in 51% of the cases, small bowel in 49% of the cases, and anum in less than 1%. Median age of patients was 61-year-old. The most frequent histology was infiltrating lobular carcinoma followed by infiltrating ductal carcinoma. In more than half of patients the diagnosis was made after the diagnosis of BC and in many cases in emergency setting,for bowel obstruction, bleeding or perforation. Diagnosis was achieved through endoscopy, radiological examination or both. In most of the cases patients underwent surgery with or without systemic therapies.
Research conclusions
Although intestinal metastases of BC are considered a rare condition, several cases are reported from the available literature.
Research perspectives
Our paper comprehends summarizes epidemiology, symptoms, diagnostic work-up,therapy and survival of this condition. On this account it gives an estimate of the problem and could lead to and represent the basis for the creation of a multicentre prospective study or a registry.
杂志排行
World Journal of Clinical Oncology的其它文章
- Reduction of muscle contraction and pain in electroporation-based treatments: An overview
- Prognostic role of sarcopenia in metastatic colorectal cancer patients during first-line chemotherapy: A retrospective study
- Thymoquinone anticancer activity is enhanced when combined with royal jelly in human breast cancer
- Hepatic Langerhans cell histiocytosis: A review
- Immune response evaluation criteria in solid tumors for assessment of atypical responses after immunotherapy
- COVID-19: Where is the treatment?