Immune response evaluation criteria in solid tumors for assessment of atypical responses after immunotherapy
2021-08-02DavideIppolitoCesareMainoMariaRagusiMarcoPortaDavideGandolaCammilloTaleiFranzesiTeresaPaolaGiandolaSandroSironi
Davide Ippolito, Cesare Maino, Maria Ragusi, Marco Porta, Davide Gandola, Cammillo Talei Franzesi, Teresa Paola Giandola, Sandro Sironi
Davide Ippolito, Cesare Maino, Maria Ragusi, Marco Porta, Davide Gandola, Cammillo Talei Franzesi, Teresa Paola Giandola, Department of Diagnostic Radiology, H. S. Gerardo Monza,School of Medicine, University of Milano-Bicocca, Monza 20900, Italy
Sandro Sironi, Diagnostic Radiology, University of Milano-Bicocca, Bergamo 24127, Italy
Abstract In 2017, immune response evaluation criteria in solid tumors (iRECIST) were introduced to validate radiologic and clinical interpretations and to better analyze tumor’s response to immunotherapy, considering the different time of following and response, between this new therapy compared to the standard one. However,even if the iRECIST are worldwide accepted, to date, different aspects should be better underlined and well reported, especially in clinical practice. Clinical experience has demonstrated that in a non-negligible percentage of patients, it is challenging to determine the correct category of response (stable disease,progression disease, partial or complete response), and consequently, to define which is the best management for those patients. Approaching radiological response in patients who underwent immunotherapy, a new uncommon kind of target lesions behavior was found. This phenomenon is mainly due to the different mechanisms of action of immunotherapeutic drug. Therefore, new groups of response have been described in clinical practice, defined as “atypical responses,” and categorized into three new groups: pseudoprogression, hyperprogression, and dissociated response. This review summarizes and reports these patterns, helping clinicians and radiologists get used to atypical responses, in order to identify patients that respond best to treatment.
Key Words: Response evaluation criteria in solid tumors; Tumor response; Pseudoprogression; Hyperprogression; Dissociated response
INTRODUCTION
In the last few years, new therapies such as immunotherapy have been experimented with and introduced into clinical practice for the treatment of oncologic patients.Immunotherapy is a type of treatment that involves the immune system to fight cancer, targeting malignant cells and providing a precise immune response through tumor antigen recognition[1].
There are different types of immunotherapy, so different types of cancer responses can be achieved. All of them are bound by a fundamental principle: Immunotherapy is different from standard therapies (i.e.chemotherapy, radiotherapy, or oncologic surgery) because it helps the self-response to cancer[2].
For these reasons, the standard criteria for monitoring the success of therapy in oncologic patients are not sufficient. All scores, including the World Health Organization classification and the response evaluation criteria in solid tumors(RECIST 1.1.), do not consider that fighting cancer for immunotherapy requires a synergy between tumor cells and host cells[3,4]. To obviate this essential issue, since 2004, different criteria were developed to analyze these responses such as immunerelated response criteria, immune-related RECIST, and finally in 2017 immuno-RECIST (iRECIST)[5-8]. These new criteria aim to consider the variety and the time of response to immunotherapy compared with standard therapy, and to standardize and validate the radiologic and clinical interpretation[9].
However, immunotherapy raises different questions such as: why is the target lesion increased at first control after immunotherapy and reduced at its end? Why is the target legion bigger at the end of treatment, but the patient’s conditions improve?Why do some metastases disappear, and others become bigger? These different phenomena are called pseudoprogression, hyperprogression, and dissociate response,respectively, and belong to the new lexicon of cancer response to immunotherapeutic agents[10,11].
Radiologists and clinicians should be confident with these patterns (Figure 1) and the interpretation of these data to better understand and manage oncologic patients who have undergone immunotherapy.
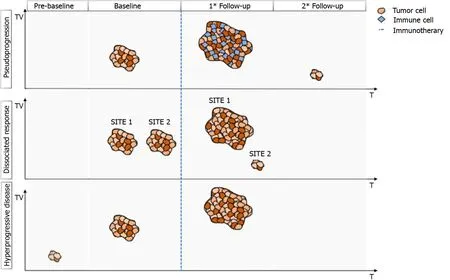
Figure 1 Graphical summary of different responses to immunotherapy. Pseudoprogression: increase of longest diameter > 20% at first follow-up,followed by a decrease of > 30% at subsequent follow-up. Dissociated response: increase of some target lesions of > 20% and reduction of at least another target lesion > 30% at follow-up. Hyperprogression: significant increase of target lesion at first follow-up; a baseline study is needed to correctly assess the hyperprogression. T: Time; TV: Tumor volume.
In this setting, the present review aims to critically analyze and summarize the most common type of responses to immunotherapy and to drive the knowledge of correct radiologic and clinical interpretation of iRECIST, strengthening the communication skills between specialists.
PSEUDOPROGRESSION
Pseudoprogression is defined as the phenomenon characterized by an initial increase in primary tumor size or new lesions appearance, after starting immunotherapy,followed by a decrease in tumor burden[12-15]. Pseudoprogression should not be considered a true tumor progression but an infiltration and recruitment of various immune cells, such as T or B lymphocytes in the tumor core[16]. Two biological hypotheses have been proposed to explain the phenomenon of pseudoprogression observed in patients treated with immuno-oncology agents. The first hypothesis concerns tumors’ continuous growth until the activation of an effective antitumoral immune response; the second one suggests that an immune-cell influx could occur in the tumoral microenvironment caused by the reactivation of the immune system,leading to inflammation and a transient increase of tumor burden[15].
A study by Cohenet al[17] described the case of a patient with melanoma brain metastasis, who was treated with pembrolizumab, presenting a pseudoprogression of brain lesions revealed through magnetic resonance imaging (MRI) and biopsy. The MRI showed an enlargement of central nervous system lesions with diffuse perilesional edema, while the histologic evaluation revealed tumor cells surrounded by reactive astrocytosis, scattered inflammatory cells, and microglial cells, which was consistent with the abovementioned response to treatment rather than tumor growth.
Rochaet al[18] described the case of a patient with end-stage squamous cell lung cancer, who was treated with nivolumab and exhibited pseudoprogression of the liver lesions, proved by the biopsy. The tissue sample revealed extensive areas of necrosis,no viable tumor cells, and lymphocyte infiltration. In the liver biopsy, the number of CD4-, CD8-and CD103-cells were increased, the ratio of CD4+/CD8+T cells was decreased, and CD68+staining indicated a higher proportion of macrophages,suggesting an inflammatory response rather than disease progression. Moreover, other cases have shown necrosis, hemorrhage, edema, and immune cell infiltration in lesions with pseudoprogression[14,15,19,20]. Therefore, the infiltration of immune cells, such as CD4+, CD8+cells and macrophages, represents the major mechanism of pseudoprogression, consequently including edema, hemorrhage, and necrosis[12].
An unconventional pattern of response to immunotherapy was first described with the development of cytotoxic T-lymphocyte antigen 4 inhibitors in melanoma, with a patient experiencing enlargement of a cutaneous lesion during the first weeks of treatment, followed by prolonged stabilization[15]. Since then, pseudoprogression has been used to describe an objective response obtained after initial progression disease and has been observed in other cancer types[16] (Figure 2).

Figure 2 Axial computed tomography images in the portal-venous phase of a 69 y/o male, ex-smoker with non-small lung cell carcinoma,during second-line therapy with Atezolizumab. A: Pre-treatment imaging show the right peri-hilar lesion; B: During follow-up after 4 wk the lesion increase in size; C and D: During the following computed tomography scans (8 and 12 wk) a significant decrease in longest diameter was achieved, confirming a final response to treatment with the presence of intercurrent (B) pseudoprogression.
The occurrence of pseudoprogression was confirmed in large trials, which allows treatment beyond progression; its incidence, reported in different tumor types, has never exceeded 10% of patients[21]. However, a recent study determined that the incidence of atypical response is about 20%, including the development of new lesions,and the increase greater than 10% in the total sum of the longest dimension[22].
Pseudoprogression has been described in different types of tumors, mainly in melanoma patients but also in non-small lung cell carcinoma (NSCLC) (Figure 3), renal cancer (RCC), urothelial cancer, uveal melanoma, Merkel cell carcinoma, mesothelioma, Hodgkin lymphoma, and head and neck squamous cell carcinoma (HNSCC)[23] and it can also occur in metastatic lesions and some oncologic patients with pleural effusion and ascites[14,24-29].

Figure 3 Axial computed tomography images in the portal-venous phase of a 65 y/o female, with non-small lung cell carcinoma and a programmed death-ligand 1 expression > 90%, during first-line treatment with Pembrolizumab. A: In the baseline examination, computed tomography (CT) shows a metastatic lesion in the right adrenal gland; B: After 4 wk of treatment, the lesion becomes bigger, with a total increment of 21%, referred to as unconfirmed progression; C-E: during following CT scans, the target lesion shows a progressive dimensional reduction with a total decrease of 46%. These variations in the size of the lesion, during immunotherapy, was in line with pseudoprogression.
The reported incidence of pseudoprogression in clinical trials was 2.78%-9.69% for melanoma, 1.81%-5.77% for NSCLC, 2.86%-8.82% for RCC, 1.49%-7.14% for urothelial carcinoma, 11.11% for uveal melanoma, 1.79% for HNSCC, 1.14% for Merkel cell carcinoma, and 6.90% for mesothelioma[12].
Clinical and biological characteristics of different tumors, the demographic characteristics of patients, and the different types of immunotherapy agents used might explain the different incidence of pseudoprogression in various types of solid tumors.In addition, according to some case reports, there might be some sites of pseudoprogression specific to the tumor type after immunotherapy, such as brain metastasis pseudoprogression of lung cancer and RCC[30,31].
Interestingly, for patients treated beyond progression, no increase in immunerelated toxicity was reported. Furthermore, patients experiencing pseudoprogression had longer overall survival (OS) compared with standard progressive disease (PD),suggesting that patients who present with pseudoprogression can effectively obtain benefit from treatment beyond progression[23].
The iRECIST guidelines proposed two specific response patterns: unconfirmed PD(iUPD) and confirmed PD (iCPD). The iUPD is defined as PD for the RECIST v1.1 criteria that is not confirmed at the follow-up imaging assessment within 4-8 wk. The iCPD is defined as the appearance of a new lesion or further growth of the sum of measures of target lesions of 5 mm or greater at the diagnostic follow-up after the iUPD within 4-8 wk, or as an increase in a non-target lesion, that was initially categorized as iUPD. If no change in tumor size nor extent from iUPD occurs, then the time point response would again be iUPD. Complete response (iCR), partial response(iPR), and stable disease (iSD) were assigned based on the RECIST 1.1. Moreover, if after iSD, iPR, or iCR, PD takes place again, we consider it as iUPD and reset the bar again through the application of the so-called “dynamic time point”[7]. To resume,iUPD can be assigned multiple times as long as iCPD is not confirmed at the next assessment and iRECIST requires the confirmation of progression to rule out or confirm pseudoprogression.
The iRECIST guidelines proposed a status of iUPD, which would allow the continuation of treatment and follow-up more closely to better benefit patients. This approach allows the identification, understanding, and better characterization of atypical responses, such as delayed responses that occur after pseudoprogression[7].
To differentiate pseudoprogression from true progression, the iRECIST guidelines recommend that clinical trials should only include patients who are clinically stable to continue treatments until the next assessment (≥ 4 wk later). In these cases, the next imaging assessment should be performed no longer than 8 wk later, to ensure that patients remain fit for rescue therapies[7].
Among the potential useful methods to identify pseudoprogression in tumors treated with immunotherapy and to differentiate it from the true progression of the disease, the combination of biopsy and histopathologic examination is considered the gold standard, although it presents some disadvantages due to the invasive nature of the procedure. Compared to biopsy, the radiographic follow-up presents incomparable advantages in the monitoring of pseudoprogression. It could be used in any type of tumor with measurable lesions and it is convenient, non-invasive, and can avoid prematurely discontinued immunotherapy for pseudoprogression. In addition to radiological computed tomography (CT) follow-up, other proposed methods to determine pseudoprogression included MRI and positron emission tomography(PET)/CT, which can distinguish inflammatory cell infiltration from the enlarged tumor tissue, at least theoretically. In recent literature, the circulating tumor’s DNA and interleukin-8 serum levels were purposed in the follow-up of oncologic patients to quickly identify a possible pseudoprogression[12].
A summary of the most important studies focusing on pseudoprogression is reported in Table 1.
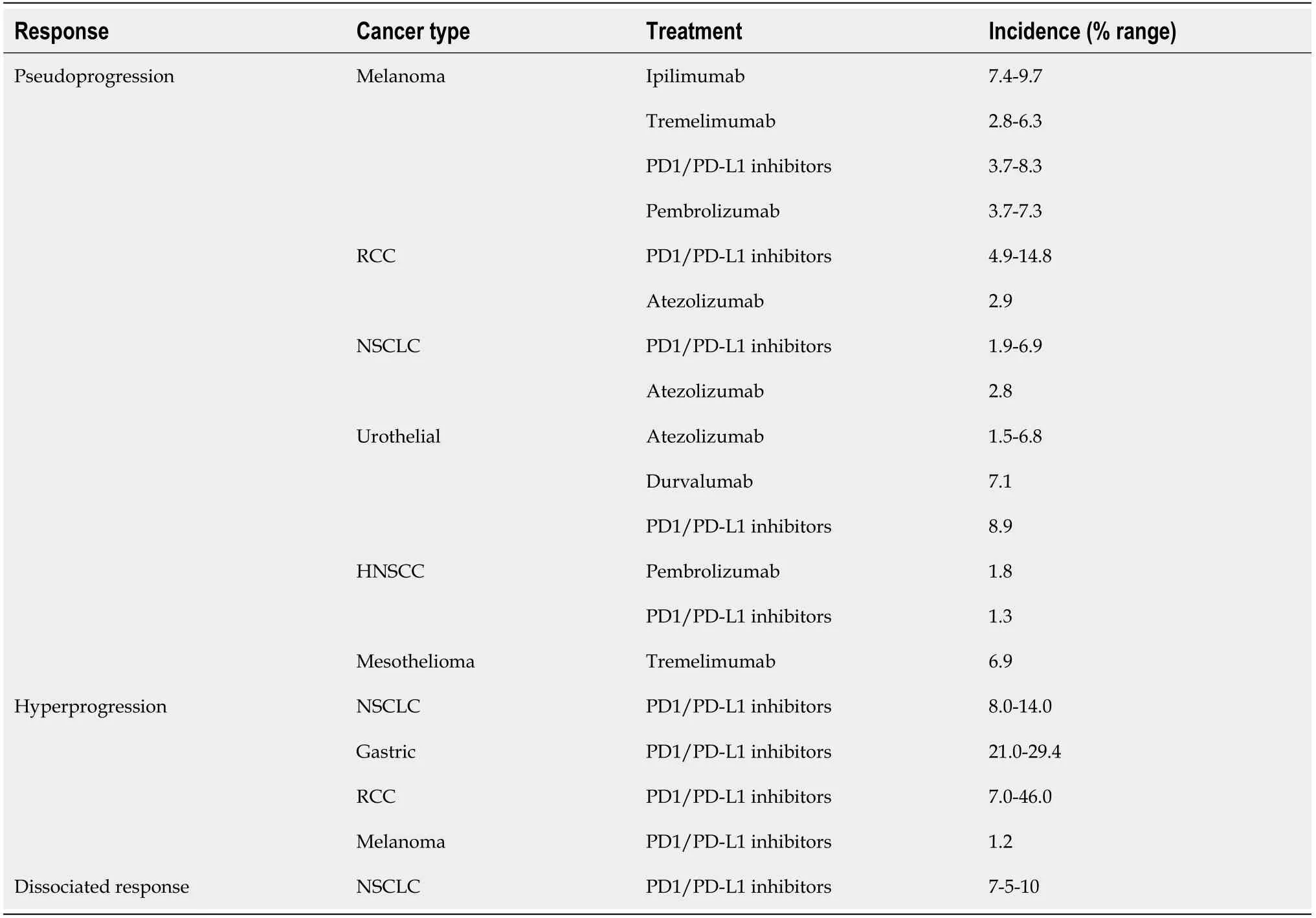
Table 1 Incidence of atypical response in different cancer types and treatments, according to the most recent literature
HYPERPROGRESSION
Hyperprogressive disease (HPD) is considered fast tumor growth, after starting immunotherapy, regarding the absolute mass. However, compared with the other atypical patterns, HPD relies on its intrinsic definition in the “expected” response, and consequently, a specific description is currently missing. For example, empiric doubling of tumor volume or by using linear growth in tumor diameter have been proposed to identify the HPD and, as a matter of fact, recently published papers reported different ways to define HPD and different thresholds to stratify pa-tients[32-34]. Moreover, considering that HPD can be shown in different cancer types, a standardized definition is needed.
Different cellular and genetic triggering events were studied to better define and understand HPD. The first described is linked to cytotoxic agents used before immunotherapy, probably causing a decreased effect of the last one[35] due to clones’selection able to escape therapy. On the other hand, new immunotherapeutic agents can bind other than targeted receptors and allow rapid tumor growth. Finally,different genetic mutations, such as the most common one Janus kinase 1/2 mutation,can be directly linked to HPD, generating resistance to immunotherapy and resulting in a fast tumor volume increase. The tumor microenvironment can be strictly involved in HPD, especially by immune cell infiltration, as reported in previous papers[36-38].
From a radiological point of view, to identify HPD, at least one imaging exam should be obtained before and one after starting immunotherapy, to correctly establish an increase in tumor volume higher than the expected one[39,40].
Even if the iRECIST algorithm is the most widely applied in clinical practice, it does not suggest evaluating the pretreatment imaging data to identify the tumor growth rate (TGR), and suspected hyperprogressive patients should be followed-up for at least 12 wk for definitive confirmation[39]. The identification of HPD poses a challenge for the iRECIST, which fail to capture pre- and post-treatment tumor growth kinetics(TGK) at early times of disease, and consequently, different parameters such as“RECIST progression at the first evaluation”[39], TGR[40], TGK ratio (ratio of the slope of tumor growth before treatment and the slope of tumor growth on treatment), time to treatment failure (TTF)[41], and the combination of clinical and radiological criteria[42] have been proposed.
A recent study by Gomes da Moraiset al[43], combining four different definitions for HPD previously proposed, found no overall significant differences between baseline and post-baseline tumor growth rate (P= 0.93). Finally, the authors confirmed that the progression-free survival (PFS) was shorter in patients with HPD compared with non-HPD ones.
A metanalysis published by Kimet al[44] evaluated a total of 217 HPD cases of 1519 cancer patients. Considering the lack in HPD definition, its incidence ranged from 1%to 30%, in line with Frelautet al[23], reporting a range from 7% and 29%. Authors identified age (> 65 years), gender (female), aggressive primary tumor (high recurrence rate, > 2 metastatic sites), histological and immunological profiling (i.e.low programmed death-ligand 1 expression, epidermal growth factor receptor, mouse double minute 2 homology and DNA (cytosine-5)-methyltransferase 3A alterations) as predictive factors for HPD.
Analyzing the most important recent studies, Parket al[45] identified HPD in 18 patients (14.4%) with head and neck cancer, underlying that younger age, a primary tumor of the oral cavity, and previous locoregional irradiation are significant predictors of HPD. Moreover, patients with HPD showed a shorter median PFS and OS.
To date, different published papers have investigated the importance of HPD in lung cancer patients. Kimet al[46] observed HPD in 55 (20.9%), 54 (20.5%), and 98(37.3%) patients according to the TGK, TGR, and TTF, underlying that HPD was associated with worse PFS and OS. The same results in terms of incidence were reported in previous retrospective studies by Ferraraet al[40] (14%), Lo Russoet al[42](26%), Kimet al[46] (21%), as summarized in the review by Kimet al[44]. More recently, Kaset al[47], with a retrospective study including 406 patients, suggested a new definition for HPD in patients with NSCLC, based on ΔTGR.
Aokiet al[48] and Sasakiet al[49] studied the importance of HPD in gastric cancer patients reporting an incidence of 29.4% and 21% after nivolumab treatment,respectively. Both studies reported a slight decrease in PFS and OS in patients with HPD.
Kimet al[50] reported that HPD exists in a fraction of hepatocellular carcinoma(HCC) patients who received programmed cell death protein 1 (PD-1) blockade:Analyses of the baseline immune profile and on-treatment tumor growth dynamics could promote optimal patient selection and earlier identification of rapid tumor growth induced by PD-1 inhibitors in HCC patients[50].
Zhenget al[51] reviewed patients with RCC under immunotherapy, finding that the incidence of HPD ranged between 7% and 74% without any strong suggestive factors associated.
Regarding melanoma, immunotherapy treatment is not extensively reported in the literature. A recent retrospective study by Haoet al[52] and Schuivelinget al[53],enrolling 168 patients, reported a 1.2% incidence of HPD.
According to the RECIST working group, a CT scan 8 wk after the first treatment is needed to evaluate early response[7]. In line with the guidelines, if progression is not confirmed, the follow-up should be continued as previously planned, while in case of suspected progression at first-imaging follow-up, a confirmatory CT 4 wk later should be required. Moreover, considering the importance of pre-baseline imaging, a CT scan at least 1 mo before starting immunotherapy should be evaluated to define the tumor volume and consider it in further evaluations. During the anamnestic questionnaire,special attention should be addressed to pre-immunotherapy treatments, specifically regarding conventional cytotoxic agents, as aforementioned[39,40]. Radiological assessment, both CT- and MRI-based, is fundamental to determine the growth rate;however, the true positive rate can be weakened by pseudoprogression in case of prebaseline missing, because it is not possible to distinguish between the two patterns.
On these bases, a complete assessment based on clinical and radiological findings,along with a careful evaluation of pre-baseline imaging, is needed to correctly stratify patients suspected of HPD, to define the best clinical approach possible to increase PFS and OS. The difficulties to standardize the HPD definition by using radiological criteria firstly rely on the various types of cancer to deal with and, consequently, on the different imaging techniques considered as the reference standard for staging and re-staging patients.
A summary of the most important studies focusing on hyperprogression is reported in Table 1.
DISSOCIATED RESPONSE
Besides the mixed pattern of response arising from traditional platinum-based chemotherapy, the development of immunotherapy has led to the introduction of the concept of dissociated response (DR).
DR has been recently described as a concomitant increase in the size of some target lesions or the appearance of new lesions, accompanied by regression of other ones[54].A combination of factors may explain the biological mechanisms of a dissociated tumor response. Tumor heterogeneity within an individual patient and differences in tissue penetration of anti-cancer drugs have been proposed as potential reasons for DR[55]. Tumoral cells can undergo clonal evolution from a single progenitor cell into more aggressive and therapy-resistant cells, due to genomic instability of solid cancer cells.
This genotypic and phenotypic heterogeneity is an unfavorable prognostic factor for cells’ survival, and it can explain the DR, particularly when using targeted therapies due to their selective pressure on tumor evolution. Moreover, the heterogeneity of the immune environment of the lesions can actively influence therapeutic response and therefore explain different responses[56] (Figure 4).

Figure 4 Axial computed tomography images in the portal-venous phase of a 57 y/o female ex-smoker with non-small lung cell carcinoma during second-line treatment with Pembrolizumab. Images show a dissociated response of two target lesions. A: The left peri-hilar lesion progressively decreased in size during follow-up, if compared to the pre-treatment computed tomography scan (after 3 wk and after 9 wk of immunotherapy from left to right, respectively); B: The second target lesion in left lung firstly regressed after 3 wk of immunotherapy showing, then a progression during the follow-up period(from left to right, respectively).
In literature few studies reported on the incidence of DR, ranging from 7.5% to 10%[54,55,57]. Using fluorodeoxyglucose PET/CT, Humbertet al[58] recently pub-lished a prospective study including 50 patients with NSCLC treated with pembrolizumab in first-line therapy or with nivolumab in second-line therapy, showing that 10% of the population had a DR.
DR has been associated with different prognoses compared to progressive or non-PD. Tazdaitet al[54] observed similar survival between patients with the non-PD and those with the atypical response, even if pseudoprogression and DR were not evaluated separately. On the contrary, the higher survival of patients with DR,compared to those with PD, was confirmed both by Tazdaitet al[54] and Tozukaet al[55], suggesting that the prognosis of patients with DR is probably intermediate between those with PD and those with the non-PD.
In the literature, several different definitions of DR were encountered; in particular,it is still not clear if a concomitant progression and reduction of different lesions are sufficient to consider as DR, or if it is necessary to reach at least 20% of PD and 30% of PR[54,55,57]. On PET/CT, DR definition should be inspired by PET Response Criteria In solid tumor (PERCIST) and defined as a concomitant relative decrease > 30% in some tumor lesions metabolism and relative metabolic increase > 30% in others.
An important issue is the optimal duration of treatment due to the potential of late treatment effect and the rare phenomenon of pseudoprogression. Many clinicians choose to continue treatment beyond progression with immunotherapy according to the RECIST[59]. As the progressing lesions might represent pseudoprogression, the monitoring and management of patients with the DR should be similar to that of patients with pseudoprogression, if the patient is clinically stable. A recent study shows that continuing immunotherapy post-DR had significantly better survival than discontinuing therapy[57].
Besides, continuing immune checkpoint inhibitor treatment plus local ablative therapy targeted to progressing lesions could be a valid alternative to immunotherapy alone in case of single progressive lesions[56]. However, if the patient is clinically deteriorating the interruption of immune checkpoint inhibitor treatment and switching to another therapy, or clinical trial participation, should be considered[60].
The high number of atypical responses such as pseudoprogression and DR suggest that in most cases the RECIST 1.1 underestimates the benefit of treatment with immunotherapy and the new iRECIST are certainly superior in the evaluation of responses. The iRECIST consider consistently pseudoprogression, while DR is not considered[7,11], suggesting that they may not correctly describe the clinical benefit from immunotherapy[61].
Considering the different interpretations of DR given by the different authors, a more uniform definition of this phenomenon is crucial to assess the correct prognosis of patients with DR compared to progressive and non-PD after immunotherapy. As suggested by Humbert and Chardin[56], DR on CT exam should be inspired by RECIST 1.1, defined as a concomitant decrease in size > 30% in some lesions and increase in size > 20% in others (and/or presence of new lesions), while on PET/CT,DR should be motivated by PERCIST criteria, defined as a concomitant decrease > 30%in some tumor lesions metabolism and metabolic increase > 30% in others (and/or new hypermetabolic lesions).
A summary of the most important studies focusing on DR is reported in Table 1.
To conclude, DR should be considered in the iRECIST in addition to or separately from a PD, partial response, and stable disease, through radiological evaluation, for a more precise evaluation of tumor response to the immunotherapy.
CONCLUSION
iRECIST can help to correctly categorize the classes of response to immunotherapy treatment by dividing patients into four main groups (iSD, iPR, iCR, iPD), according to the radiological target lesion modifications, achieved along the time, and the standard solid response criteria (RECIST 1.1). Recently, other different kinds of response have been described in literature after immunotherapy treatment, defined as atypical responses, categorized in three patterns: pseudoprogression, hyperprogression, and dissociated response. The correct knowledge of these new atypical patterns should be correctly assessed by both radiologists and clinicians, through the deep investigation of clinical anamnesis and imaging findings to guarantee the best management.
杂志排行
World Journal of Clinical Oncology的其它文章
- Intestinal metastasis from breast cancer: Presentation, treatment and survival from a systematic literature review
- Reduction of muscle contraction and pain in electroporation-based treatments: An overview
- Prognostic role of sarcopenia in metastatic colorectal cancer patients during first-line chemotherapy: A retrospective study
- Thymoquinone anticancer activity is enhanced when combined with royal jelly in human breast cancer
- Hepatic Langerhans cell histiocytosis: A review
- COVID-19: Where is the treatment?