Acute mesenteric ischemia and small bowel imaging findings in COVID-19:A comprehensive review of the literature
2021-07-28LorenaPirolaAndreaPalermoGiacomoMulinacciLauraRattiMariaFicheraPietroInvernizziChiaraViganSaraMassironi
Lorena Pirola,Andrea Palermo,Giacomo Mulinacci,Laura Ratti,Maria Fichera,Pietro Invernizzi,Chiara Viganò,Sara Massironi
Lorena Pirola,Andrea Palermo,Giacomo Mulinacci,Laura Ratti,Maria Fichera,Pietro Invernizzi,Chiara Viganò,Sara Massironi,Division of Gastroenterology and Center for Autoimmune Liver Diseases,Department of Medicine and Surgery,University of Milano-Bicocca,Monza 20900,Italy
Lorena Pirola,Andrea Palermo,Giacomo Mulinacci,Laura Ratti,Maria Fichera,Pietro Invernizzi,Chiara Viganò,Sara Massironi,European Reference Network on Hepatological Diseases,San Gerardo Hospital,Monza 20900,Italy
Abstract BACKGROUND Coronavirus disease 2019(COVID-19),an infectious condition caused by severe acute respiratory syndrome coronavirus 2(SARS-CoV-2),has rapidly spread worldwide since its first description in Wuhan in December 2019.Even though respiratory manifestations are the most prevalent and responsible for disease morbidity and mortality,extrapulmonary involvement has progressively gained relevance.In particular,gastrointestinal(GI)signs and symptoms,reported in up to two-thirds of patients with COVID-19,might represent the first and,in some cases,the only disease presentation.Their presence has been associated in some studies with an increased risk of a severe disease course.Proposed pathogenic mechanisms explaining GI tract involvement are either direct viral access to intestinal cells via angiotensin-converting enzyme 2 or indirect damage of the intestinal wall through mesenteric ischemia induced by the hypercoagulable state associated with COVID-19 infection.Although not typical of SARS-CoV-2 infection,several small bowel manifestations have been described in infected patients who underwent any form of abdominal imaging.The radiological findings were mainly reported in patients with abdominal symptoms,among which abdominal pain was the most common.AIM To discuss small bowel radiological manifestations of SARS-CoV-2 infection in abdominal imaging studies.METHODS Bibliographical searches were performed in PubMed,using the following keywords:“covid-19” AND “imaging” AND “gastrointestinal” OR “abdominal”OR “small bowel”.RESULTS Of 62 patients with described radiologic small bowel alterations,mesenteric ischemia was diagnosed in 31 cases(50%),small bowel wall thickening in 10 cases(16%),pneumatosis in nine cases(15%),intussusception in eight cases(13%),pneumoperitoneum in two cases(3%)and paralytic ileus in two cases(3%).We also reported mesenteric adipose tissue hypertrophy and lymph nodes enlargement in a young woman.CONCLUSION So far it is difficult to establish whether these manifestations are the direct consequence of SARS-CoV-2 infection or collateral findings in infected patients,but their recognition would be pivotal to set a closer follow-up and to reduce missed diagnoses.
Key Words:COVID-19;SARS-CoV-2;Radiology;Small intestine;Abdomen
INTRODUCTION
Coronavirus disease 2019(COVID-19)is an infectious condition caused by severe acute respiratory syndrome coronavirus 2(SARS-CoV-2),firstly isolated in December 2019 in Wuhan,China[1].As of February 8,2021,there have been more than one hundred million confirmed cases of COVID-19,with more than two million deaths[2].The most common COVID-19 symptoms include fever(85.6%),cough(65.7%),fatigue(42.4%)and dyspnea(21.4%)[3].Although respiratory tract manifestations are the most prevalent and responsible for disease morbidity and mortality,extrapulmonary involvement has progressively gained relevance.In particular,gastrointestinal(GI)symptoms are described in a significant proportion of infected patients,being reported in up to two-thirds of patients with COVID-19[4].Several studies suggest that GI symptoms might not only be the initial presentation of SARS-CoV-2 infection but are also the only manifestation reported during disease course in about 10% of cases[5].Patients presenting with GI manifestations alone have a delayed diagnosis[6].Furthermore,in some studies the presence of GI symptoms has been associated with an increased risk of severe clinical course,but the real impact of GI involvement on disease outcome is still a matter of debate[6,7].The most commonly reported GI symptoms were loss of appetite(21%),diarrhea(9%),nausea or vomiting(6%),and abdominal pain(3%)[6].It has been widely described and accepted in the literature that SARS-CoV-2 exploits angiotensin-converting enzyme 2(ACE2)to gain access to single cells[8].Hence,it is possible to assume that cells with higher expression of ACE2,such as enterocytes in the GI tract[9],are more susceptible to infection[10].Several reports have evaluated the pulmonary radiological findings in COVID-19,which facilitate disease recognition and add to the understanding of its pathogenic mechanisms in the lung[11].However,despite the broad spectrum and the high prevalence of GI symptoms,only a few studies have assessed the abdominal radiological findings in COVID-19 patients,and only a few of those have focused on small bowel alterations.Furthermore,the pathogenic mechanisms behind the described findings remain unclear,highlighting the importance of collecting further evidence on the topic.In this review,we analyzed the radiological small bowel findings in patients with COVID-19 and evaluated their impact on the whole clinical picture of the disease.
MATERIALS AND METHODS
Bibliographical searches were performed in PubMed,using the keywords “covid-19”AND “imaging” AND “gastrointestinal” OR “abdominal” OR “small bowel”.PubMed was used to search for all relevant articles published since the first description of SARS-CoV-2 infection,which occurred in December 2019,until the end of January 2021.Reference lists from studies selected from the electronic search were manually searched to identify further relevant reports.Reference lists from all available review articles,primary studies,and proceedings of major meetings were also considered.Articles published as abstracts were included.Only English-language papers were included.
RESULTS
Thirty-nine articles describing small bowel imaging findings in patients with COVID-19 were identified.The review included 28 case reports,six case series,and five retrospective studies discussing radiological manifestations of SARS-CoV-2 infection in abdominal imaging studies.Several small bowel radiological manifestations have been described in infected patients,with a prevalence ranging from 3% to 21%[12,13].They were mainly reported in patients with abdominal symptoms,among which abdominal pain was the most common.Of the 62 patients with small bowel radiological findings,acute mesenteric ischemia(AMI)was the most prevalent condition,diagnosed in 31 cases(50%).The characteristics of COVID-19 patients with AMI are shown in Table 1.Other radiological findings(Figure 1)were small bowel wall thickening in 10 cases(16%),pneumatosis in nine(15%),intussusception in eight(13%),pneumoperitoneum in two(3%),and paralytic ileus in two(3%).A summary of those findings is shown in Table 2.In addition,we reported mesenteric adipose tissue hypertrophy and lymph node enlargement in a young woman.
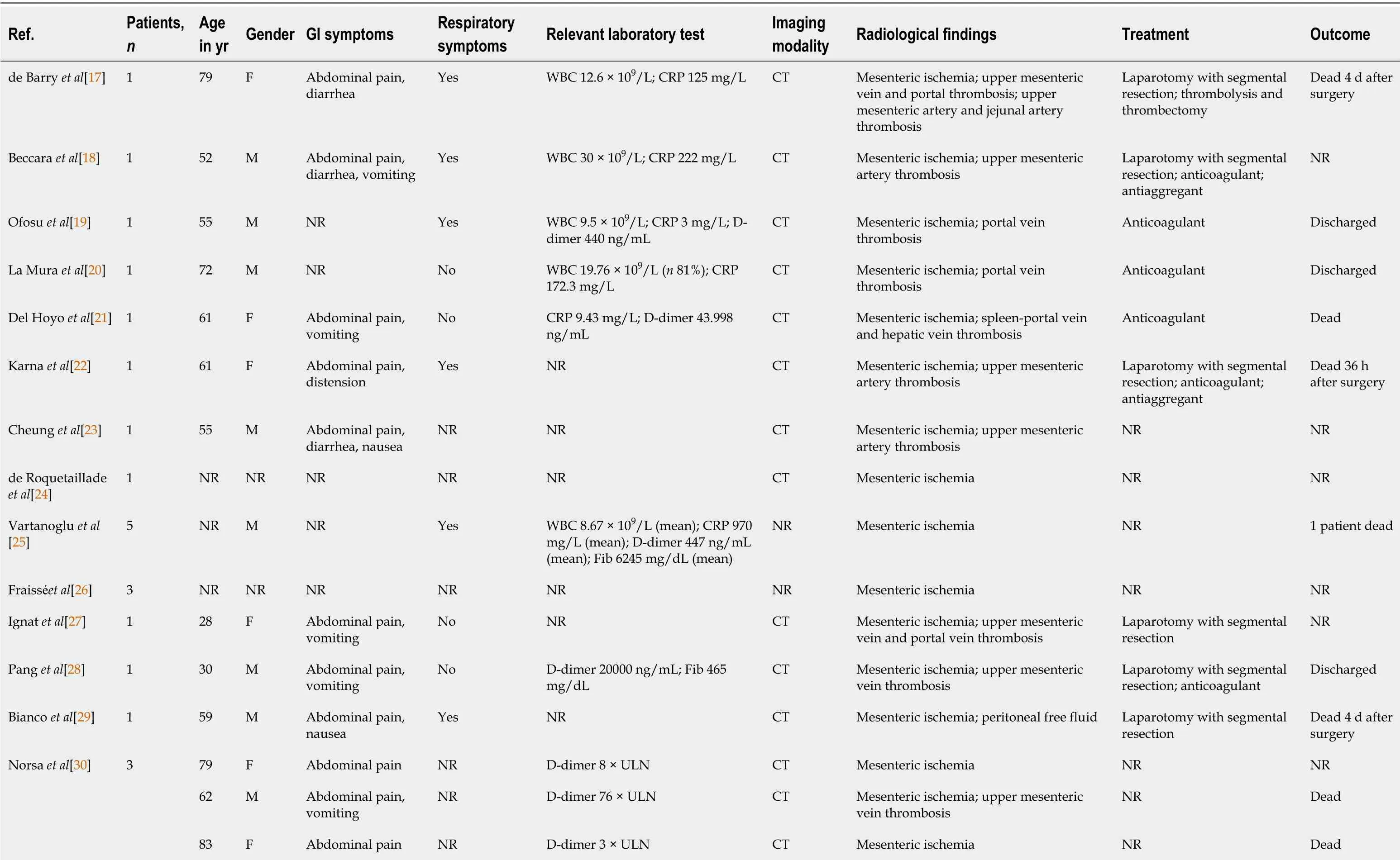
Table 1 Clinical characteristics and radiological findings of acute mesenteric ischemia in coronavirus disease-2019 patients

CRP:C-reactive protein;CT:Computed tomography;Fib:Fibrinogen;N:Neutrophil;NR:Not reported;RX:Radiography;US:Ultrasound;WBC:White blood cell.
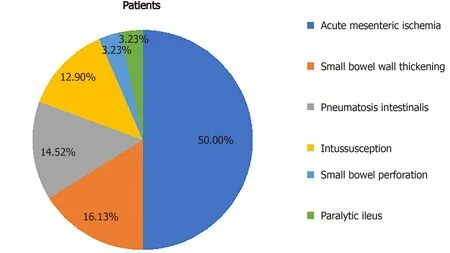
Figure 1 Proportions of radiologic small bowel manifestations reported since the beginning of the severe acute respiratory syndrome coronavirus 2 pandemic.

Table 2 Other small bowel radiological findings in coronavirus disease-2019 patients and relevant clinical characteristics
AMI
AMI is a pathological condition characterized by a sudden decline in blood flow through the mesenteric vessels,resulting in a discrepancy between the metabolic need of the visceral organs and actual oxygen delivery[14].If untreated,it may lead to small bowel wall necrosis,with a mortality rate of up to 80%[15].Among the causes of AMI,the most prevalent are acute mesenteric artery embolism,nonocclusive mesenteric ischemia[16],and acute mesenteric vein thrombosis.So far,22 papers have been published describing mesenteric ischemia in 31 COVID-19 patients,including 17 case reports,two case series,and three retrospective studies[17-38].The characteristics and radiological findings of COVID 19 patients with AMI are reported in Table 1.All but one patient underwent abdominal contrast-enhanced computed tomography(CT)scan after the onset of GI symptoms such as nausea,vomiting,and/or abdominal pain.Among the vascular findings,the most frequent were nine cases with thrombosis of the upper mesenteric artery or jejunal artery and nine cases of thrombosis of splanchnic veins,of which seven involved the portal vein,five involved the superior mesenteric vein(Figure 2),and one involved splenic and hepatic veins.Other findings described in association with AMI were the presence of liquid in the peritoneal cavity(two cases),bowel distension(one case),mesenteric intravenous air(one case),and splenic infarction(one case).From a pathological perspective,it is of interest that none of the patients had evidence of a systemic atherosclerotic disorder or other pathologic conditions that could possibly explain the findings.Treatment of AMI was reported in 17 cases.Thirteen(76%)were treated by segmental resection of small bowel,and anticoagulant therapy alone was administered in four cases.Of the nineteen patients with a reported outcome,nine(47%)died.
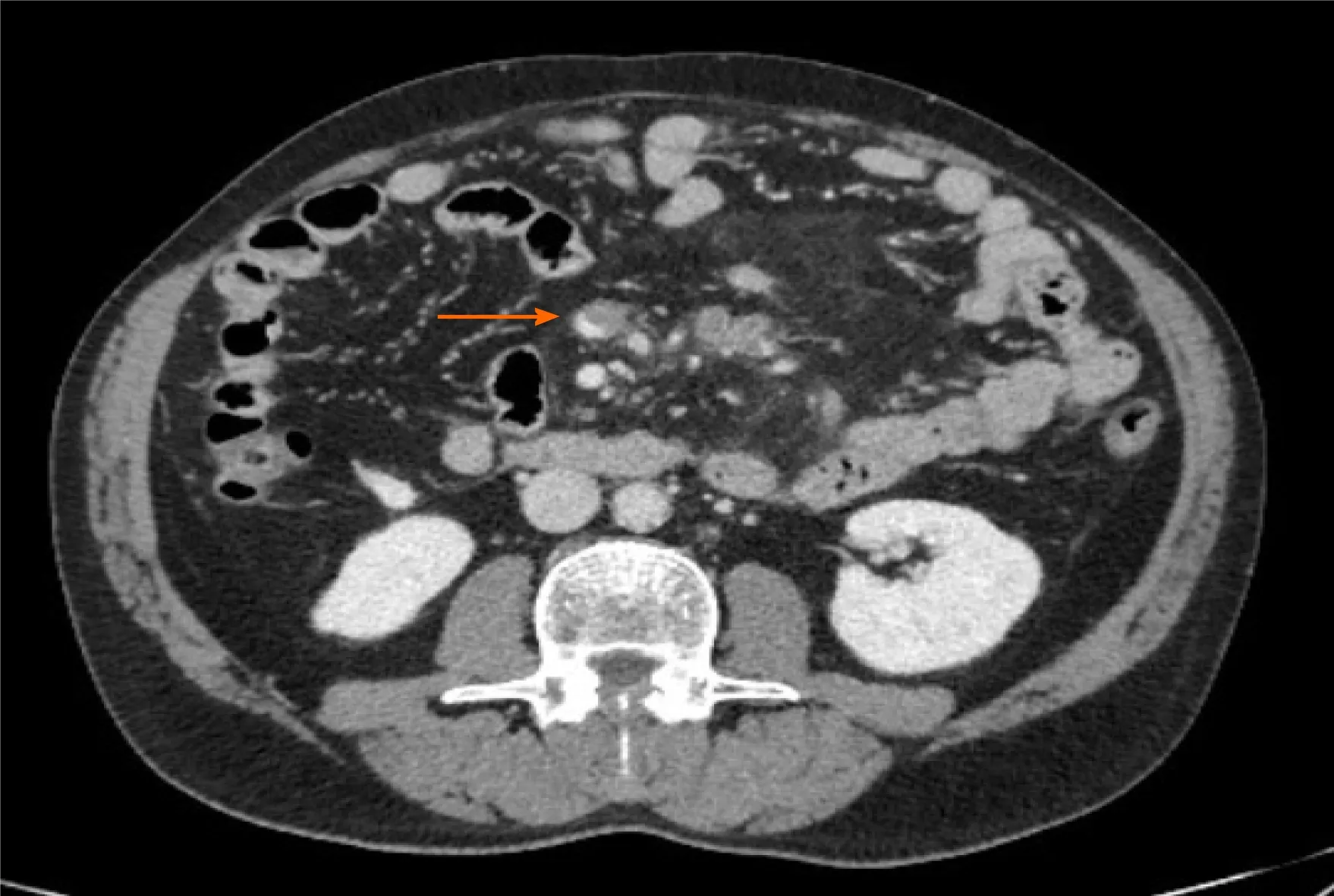
Figure 2 Computed tomography image showing partial superior mesenteric vein thrombosis in a man with severe acute respiratory syndrome coronavirus 2 infection.
Small bowel wall thickening
Thickening of the small bowel wall may occur secondary to neoplastic,inflammatory,infectious,or ischemic conditions[39].It was first described by Hellingeret al[40]in a patient presenting at the emergency room with abdominal symptoms,and this condition has been subsequently reported in other COVID-19 patients(Figure 3).At the time of writing,we identified five papers,three case reports and two retrospective studies,describing ten patients with radiological evidence of small bowel wall thickening.In a study of 412 patients admitted to the hospital for SARS-CoV-2 infection,42 underwent abdominal CT scans.In five of those patients(11.9%)small bowel thickening,reported as a single-wall thickness greater than 3 mm in distended loops or greater than 5 mm in collapsed loops[12].In a report including 141 COVID-19 patients who underwent abdominopelvic CT within 14 d of diagnosis,GoldbergSteinet al[13]reported a small bowel thickening prevalence of 2.5%.In addition,diffuse mural wall thickening of the ileum was reported in a single case study of a 11-year-old boy with SARS-CoV-2 infection,who presented to the emergency room with fever,diarrhea,and abdominal pain,without respiratory symptoms[41].Lastly,Guoet al[42]described segmental wall thickening involving a segment of jejunum in a 29-year-old man presenting with diarrhea and fever.The cause of small bowel thickening in SARSCoV-2 infected patients is still unclear.It may be a manifestation of local inflammation and edema secondary to direct or indirect viral damage of the bowel wall.Another hypothesis is that may be linked to hypercoagulability secondary to viral infection,which may promote formation of fibrin clots in the microcirculation,leading to ischemia and edema.

Figure 3 Magnetic resonance image showing distal ileum wall thickening in a young woman with severe acute respiratory syndrome coronavirus 2 infection.
Pneumatosis intestinalis
Pneumatosis intestinalis is a radiological sign reflecting the presence of gas within the intestinal wall,most commonly in the mucosa or submucosa.Pneumatosis can occur in any part of the digestive tract,and may even be accompanied by the presence of gas in the portal or mesenteric vein[43].The clinical relevance of pneumatosis intestinalis varies widely and ranges from a benign to life-threatening condition depending on the underlying cause[44].This pathologic finding has been previously described in association with viral infections,such as cytomegalovirus,adenovirus,rotavirus,and norovirus,and the proposed pathogenic mechanism was direct mucosal damage caused by viral activity[44-47].
So far,four papers,one case report,one case series,and two retrospective studies,have described pneumatosis intestinalis in nine patients with SARS-CoV-2 infection.Bhayanaet al[12]described pneumatosis intestinalis of the small bowel in four of 42 COVID-19 patients(9.5%)with abdominal CT scans.The percentage reached 20% in patients admitted to the intensive care unit.All patients underwent laparotomic exploration.Two cases showed frank signs of bowel necrosis,with bowel resection performed in one.Fibrin clots were detected in arterioles adjacent to the necrotic mucosa in histological samples.In a retrospective study,Tirumaniet al[48]described small bowel pneumatosis with portal venous gas in one of 73 SARS-CoV-2 infection patients with abdominal CT scans.Pneumatosis intestinalis of the small bowel was also reported in a small study of three cases and in a single-patient case report.Complete resolution was reported following conservative of a patient with widespread pneumatosis affecting the jejunum,proximal ileum,and caecum,for which surgery was deemed to be associated with unacceptably high morbidity[49].In the remaining three patients,an open abdomen with negative pressure therapy was successfully performed without the need of intestinal resection[50].The rationale behind this approach lies in the capability of either increasing gastrointestinal arterial and venous blood flow through intra-abdominal pressure reduction and dampening intestinal cytokine release in the peritoneal cavity,which might also prevent the deterioration of lung function[12,51,52].
Intussusception
Intussusception is the invagination of a segment of the bowel within a more distal one[53].It is the most common cause of bowel obstruction in infants,usually occurring between 4 and 10 mo of age[53].On the contrary,intussusception in adults is a rare disease,accounting for less than 5% of bowel obstruction episodes[53].In both children and adults,intussusception usually involves the ileum,with ileocecal valve invagination into the cecum being the most common localization.Furthermore,90% of cases of intussusception in adults are secondary to a well-defined pathological condition,such as inflammatory bowel disease,postoperative tractions,Meckel’s diverticulum,benign and malignant lesions,metastatic neoplasms,or even an iatrogenic cause(e.g.,intestinal tubes,jejunostomy feeding tubes,or gastric surgery)[53].Conversely,in the pediatric age group,approximately 90% of cases are idiopathic.In the literature,viral infection was cited as a possible cause of intussusception in children[54].Indeed,local immune activation and mesenteric adenitis may trigger enhanced peristaltic activity,consequently leading to the invagination of the proximal bowel segment into the distal one[54].
So far,eight cases of intussusception were reported in children between 4 and 10 mo of age with laboratory-confirmed SARS-CoV-2 infection in one case series,five case reports,and one retrospective study[54-60].The diagnosis was made mainly by ultrasound(US)through the presence of typical findings of intussusception,such as the doughnut sign(i.e.concentric alternating hyperechoic and hypoechoic rings);as expected,in all cases except one in which the site of intussusception was not specified,the ileocolic tract was involved.Three patients died of complications.To date,it has not been possible to establish an association between SARS-CoV-2 infection and intussusception.Testing for viral pathogens,including SARS-CoV-2,may be considered in infants with symptoms consistent with intussusception or with typical radiological findings.
Small bowel perforation
Pneumoperitoneum,an indirect sign of small bowel perforation,refers to the presence of free air in the abdominal cavity,often suspected through abdominal radiography and confirmed on CT scans[61].It has been less frequently reported than the previously mentioned radiologic features.One case report and one retrospective study described small bowel perforations in two patients with SARS-CoV-2 infection without any other possible explanation other than viral infection.Both cases were then confirmed by laparoscopic exploration[12,62].The clinical outcome was not specified in one study.In the other,despite prompt orotracheal-intubation and surgery,the patient developed refractory septic shock and died[12,62].As for the previously described findings,the disease pathogenesis is unknown.However,it is likely that small bowel perforation occurred as a consequence of either viral action on the intestinal mucosa or as a consequence of ischemic small bowel necrosis.
Paralytic ileus
Paralytic ileus is defined as a temporary functional cessation of propulsive contractions of the gastrointestinal tract,with subsequent upstream gut dilation and accumulation of secretions and gas within the lumen[63].Diagnosis of paralytic ileus is established by the coexistence of a clinical suspect and the support of radiological imaging.Many conditions may cause paralytic ileus,the most common being abdominal or retroperitoneal surgery.Other causes include the use of opioids,intraabdominal infections,bleeding,hypokalemia,and the absence of enteral nutrition[64].In patients with SARS-CoV-2 infection,one case of paralytic ileus of the small bowel was reported in a retrospective study,and another,involving both the small and the large bowel was described in a case report[13,65].
Mesenteric adipose tissue hypertrophy and enlarged lymph nodes
Even though there are very few data available in literature at the time of writing,small bowel involvement in SARS-CoV-2 infection may also lead to mesenteric activation and lymph nodes enlargement[66].We report those alterations in a 34-year-old woman with SARS-CoV-2 infection presenting abdominal pain,vomiting,and diarrhea.Abdominal US showed enlarged abdominal lymph nodes with a maximum short-axis diameter of 17 mm,and mesenteric adipose tissue hypertrophy(Figure 4).Abdominal CT confirmed the presence of multiple mesenteric enlarged lymph nodes associated with adipose tissue hypertrophy(Figure 5).

Figure 4 Abdominal ultrasound image in a 34-year-old woman with severe acute respiratory syndrome coronavirus 2 infection.Enlarged hypoechoic mesenteric lymph nodes,with a maximum longitudinal axis diameter of 17 mm(arrow,A)and hyperechoic mesenteric adipose tissue hypertrophy(arrow,B)are shown.

Figure 5 Abdominal computed tomography image showing multiple enlarged lymph nodes and mesenteric adipose tissue hypertrophy in a 34-year-old woman with severe acute respiratory syndrome coronavirus 2 infection.
DISCUSSION
In this review,we focused on the small bowel radiological findings in COVID-19 patients,as described so far mainly in patients presenting with GI symptoms.Although no specific aspect was identified,some radiological features have been reported in a significant proportion of patients with GI symptoms,reaching up to 21%of prevalence.Among them,AMI was the most frequent.AMI is an uncommon cause of abdominal pain,accounting for 0.09%-0.2% of all acute surgical admissions to emergency departments[15].Acute mesenteric arterial embolism caused by atrial fibrillation,thrombosis of the superior mesenteric artery(SMA)in a background of pre-existing chronic atherosclerotic disease,and nonocclusive mesenteric ischemia secondary to SMA vasoconstriction,are the major causes of AMI.Hypercoagulability,including that induced by inherited disorders such as Factor V Leiden and prothrombin mutations,protein S and C deficiency,and others,promote mesenteric venous thrombosis and have been described as causative agents of AMI[15].
Interestingly,enteric involvement has been described in other beta coronavirus infections such as SARS and Middle East respiratory syndrome,but a strong relationship with AMI has never been reported.Of note,all cases of AMI reported during COVID-19 infection were subsequent to direct vascular obstruction,thus ruling out the possibility of nonocclusive mesenteric ischemia[67,68].It has been widely reported that SARS-CoV-2 infection is associated with an increased risk of various thromboembolic complications[69].Indeed,SARS-CoV-2 infection induces a hypercoagulable state through systemic inflammation,endothelial activation,and hypoxia.The tropism of SARS-CoV-2 for the vascular endothelium may be explained by the expression of the ACE2,the target receptor for viral entry into cells,and endothelial damage induces massive release of Von Willebrand factor,further increasing the risk of thrombosis[70].Overall,both hemodynamic alterations consequent to vascular thrombosis and direct enterocyte damage might contribute to the development of small bowel ischemia and necrosis[70],although their exact contribution to the development of wall ischemia is still to be determined.Studies of histological samples are required to further explain the pathophysiology behind this manifestation.The mortality rate of AMI in COVID-19 is still unknown,yet it is likely to contribute significantly to an increased burden of disease.It is thus of the utmost importance to raise awareness among clinicians to recognize the typical signs of mesenteric ischemia,as early diagnosis and timely intervention are essential to decrease the mortality curve.Junget al[71]recently described the role of contrast-enhanced ultrasonography(CEUS)to detect abdominal microcirculatory disorders in severe cases of COVID-19.CEUS has good sensibility in detecting areas of reduced micro-vascularization,even in the early stages[71].Small bowel wall thickening was reported in 16% of cases.The cause is still unclear,but it may be a manifestation of local inflammation and edema secondary to direct viral damage of the bowel wall.Pneumatosis intestinalis is a radiological finding described in 15% of cases.The etiology in patients with COVID-19 remains unclear.Direct viral mucosal damage,intestinal ischemia,or atrophy of the lymphoid follicles with secondary increased mucosal permeability[72]were considered as possible pathogenic mechanisms.
Other reported imaging findings include intussusception(13%),pneumoperitoneum(3%),and paralytic ileus(3%).We also reported mesenteric enlarged lymph nodes and mesenteric adipose tissue hypertrophy in a young woman with COVID-19.It is possible that,in addition to direct viral damage of enterocytes,SARS-CoV-2 infection could promote a local immune activation with cytokines release,leading to the described alterations[66].
This review has some limitations.First,it is mainly based on case series and few retrospective studies,thus the real prevalence of the reported radiological findings may actually be significantly higher,as only a proportion of patients with GI symptoms undergo imaging studies.Further investigation of abdominal imaging abnormalities in COVID-19 patients is a topic for future research,and could help to decrease missed diagnosis,encourage closer follow-up,and decrease morbidity and mortality.
CONCLUSION
So far,the small number of reported cases does not allow to conclusively ascribe these manifestations to the direct action of SARS-CoV-2;nevertheless,it is important to exclude this infection in the current diagnostic workup of patients presenting with gastrointestinal symptoms.
ARTICLE HIGHLIGHTS
Research background
Coronavirus disease 2019(COVID-19)is an infectious disease with predominant respiratory symptoms.Yet extrapulmonary manifestations have been increasingly recognized in COVID-19 patients.In particular,gastrointestinal(GI)symptoms are reported in up to two-thirds of patients and might be the only manifestations in some cases.
Research motivation
Given the high prevalence of gastrointestinal involvement of COVID-19 and the unclear association with disease clinical outcome,we believe that it could be of interest to deeply investigate small bowel involvement in severe acute respiratory syndrome coronavirus 2 infection.
Research objectives
To analyze and to summarize small bowel radiological features described in COVID-19 patients,and possibly clarify their impact on the clinical management of COVID-19 patients presenting with GI symptoms.
Research methods
A literature search of the PubMed electronic database was conducted using the MeSH terms “covid-19”,“imaging” and “gastrointestinal” or “abdominal” or “small bowel”.The search was limited to English-language papers.All available case reports,case series and retrospective studies between December 2019 and January 2021 were included.
Research results
AMI is the major radiological finding in COVID-19 patients with small bowel involvement(50%).Less common findings are thickening of the small bowel wall,pneumatosis intestinalis,intussusception,and paralytic ileus.Furthermore,we described a case of mesenteric adipose tissue hypertrophy and enlarged lymph nodes associated to COVID-19.
Research conclusions
Gastrointestinal involvement in COVID-19 patients is highly prevalent.The most frequent small bowel alteration is AMI,a condition associated with high mortality.Raised awareness and prompt identification of small bowel involvement in COVID 19-patients could be essential to improve clinical management and clinical outcome,mainly in case of AMI.
Research perspectives
Further investigation of abdominal imaging abnormalities in COVID-19 patients may be a topic for future research and could help in reducing missed diagnoses and benefit overall morbidity and mortality.
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Current status of treatments of pancreatic and peripancreatic collections of acute pancreatitis
- Efficacy and safety of early oral feeding in postoperative patients with upper gastrointestinal tumor:A systematic review and metaanalysis
- Novel parameter based on lipid indicators ratio improves prognostic value of plasma lipid levels in resectable colorectal cancer patients
- Gastrectomy impact on the gut microbiome in patients with gastric cancer:A comprehensive review
- Robotic donor hepatectomy:Are we there yet?
- Management of early rectal cancer;current surgical options and future direction