Variations of the hilar biliary confluence from postoperative cholangiography in Chinese population
2021-07-24YuLiWeiZhngHoSunXueMinLiuYiLv
Yu Li ,,c,Wei Zhng ,c,Ho Sun ,Xue-Min Liu ,,c,Yi Lv ,,c,∗
a Department of Hepatobiliary Surgery, the First Affiliated Hospital of Xi’an Jiaotong University, Xi’an 710061, China
b National Local Joint Engineering Research Center for Precision Surgery & Regenerative Medicine, Xi’an 710061, China
c Shaanxi Province Center for Regenerative Medicine and Surgery Engineering Research, Xi’an 710061, China
TotheEditor:
Treatment of the bile ducts at the porta hepatis is a critical step for avoiding post-surgical bile leakage and atrophy of the residual liver and/or the graft during hepatobiliary surgeries,such as hemihepatectomy,surgeries for cholangiocarcinoma or procurement of graft.Precise knowledge of the bile duct anatomy in individual cases has great importance in avoiding these kinds of complications.According to the Couinaud nomenclature,the intrahepatic biliary system can be divided into eight segments: the right anterior hepatic lobe (S5,S8),the right posterior lobe (S6,S7),the left liver (S2-4),and the caudate lobe (S1).The incidence of this normal anatomy was reported in 40%–80% cases [1].Numerous intrahepatic biliary variations have been reported [2–4].However,the data for the Chinese population are paucity.
We analyzed the images of postoperative cholangiography,and proposed a more detailed classification of hilar biliary confluence( Fig.1 A-G): Type 1 is typical,common hepatic duct (CHD) formed by the fusion of the right hepatic duct (RHD) and left hepatic duct(LHD).The RHD arises through the fusion of the right anterior hepatic duct (RAHD) and the right posterior hepatic duct (RPHD); Type 2 involves triple confluence,including RAHD,RPHD,and LHD,and has two subtypes −2a,RPHD courses superiorly before fusion with RAHD and LHD,which has a Hjortsjo curve in cholangiogram; 2b,RPHD runs inferiorly before confluence with the other two ducts;Type 3 is divided into 3a and 3b,according to the drainage pattern of the RPHD; Type 4 has an accessory duct; Type 5 has no LHD,which means the bile duct of S2-S4 drains individually into the RHD or CHD; and the remaining ones were left unclassified or were classified as a complex variation.All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964Declarationof Helsinkiand its later amendments.Informed consent was obtained from all participants prior to enrollment in the study.
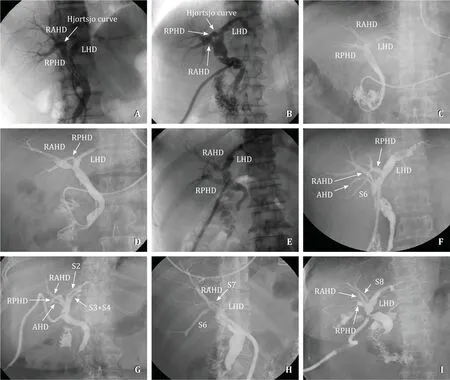
Fig.1.Intrahepatic variations in cholangiograms.A : type 1 (61.5%),a Hjortsjo curve was present; B : type 2a (15.1%),a Hjortsjo curve was viewed; C : type 2b (6.9%); D :type 3a (6.4%); E : type 3b (7.4%); F : type 4 (0.4%),a type 3a with an accessory duct; G : type 5 (1.4%),LHD was absent,S2 and S3 + 4 joined with RHD individually,and an accessory duct was present; H and I : complex type,S7,or S8 poured into the joint of LHD and RHD.RHD: right hepatic duct: RAHD: right anterior hepatic duct: LHD: left hepatic duct: RPHD: right posterior hepatic duct.
A total of 260 patients underwent cholangiography between January 2017 and June 2017 at the Department of Hepatobiliary Surgery of the First Affiliated Hospital of Xi’an Jiaotong University.Only cases with adequate cholangiography were enrolled in the analysis.After excluding 42 cases (30 cases without an intact biliary system,who underwent hemihepatectomy or lobectomy and 12 cases with unsatisfactory imaging),218 patients were included in the present study.Iconos R200 (Siemens,Munich,Germany) was used for cholangiography in the following positions: first,in the supine position with the patient’s head 20 degrees lower; second,the right anterior oblique position allowing for better display of the left and right hepatic duct boundaries; third,in the left lateral position to judge each segment duct of left liver; and fourth,in the right lateral position to show S5-S8 duct in the right liver clearly.All the cholangiograms were retrospectively evaluated by one radiologist and a surgeon in hepatobiliary surgery,and they reached a consensus for each pattern.
Of the 218 enrolled patients,124 were male and 94 were female.The primary diseases of the enrolled patients were as follows: gallstones with choledocholithiasis (n= 180),peri-ampulla carcinoma (n= 26),and pancreatic head carcinoma (n= 12).The general characteristics of the patients are shown in Table 1.After analyzing all the cholangiograms,the ratios for each type were as follows: Type 1,61.5% (n= 134),and the mean lengths of the RHD and LHD were 8.5 ± 4.81 mm and 15.6 ± 4.5 mm,respectively;Type 2,22.0% (n= 48),of which,type 2a,15.1% (n= 33),type 2b,6.9% (n= 15); Type 3,13.8% (n= 30),of which,type 3a,6.4%(n= 14),type 3b,7.3% (n= 16); Type 4,0.5% (n= 1); Type 5,1.4%(n= 3); and other complex biliary variations accounted for two cases (0.9%).In total,the prevalences of typical (type 1) and atypical (other types except type 1) anatomy were 61.5% and 38.5%,respectively.There was no significant difference in age between normal and anomalous types (P= 0.805) or among type 1,type 2,and type 3 (P= 0.418).In fact,normal biliary anatomy was present in 59.7% (74/124) of male cases and 63.8% (60/94) of female cases;the observed difference was not significant (P= 0.533).Regarding the specific atypical pattern,trifurcation (type 2) and abnormal draining of RPHD (type 3) were similar in men and women(P= 0.153 andP= 0.673,respectively).We also analyzed difference of hilar confluence type between benign or malignant diseases,however,the ratio of atypical anatomy between the two groups was similar (71/180 vs.13/38,P= 0.547).
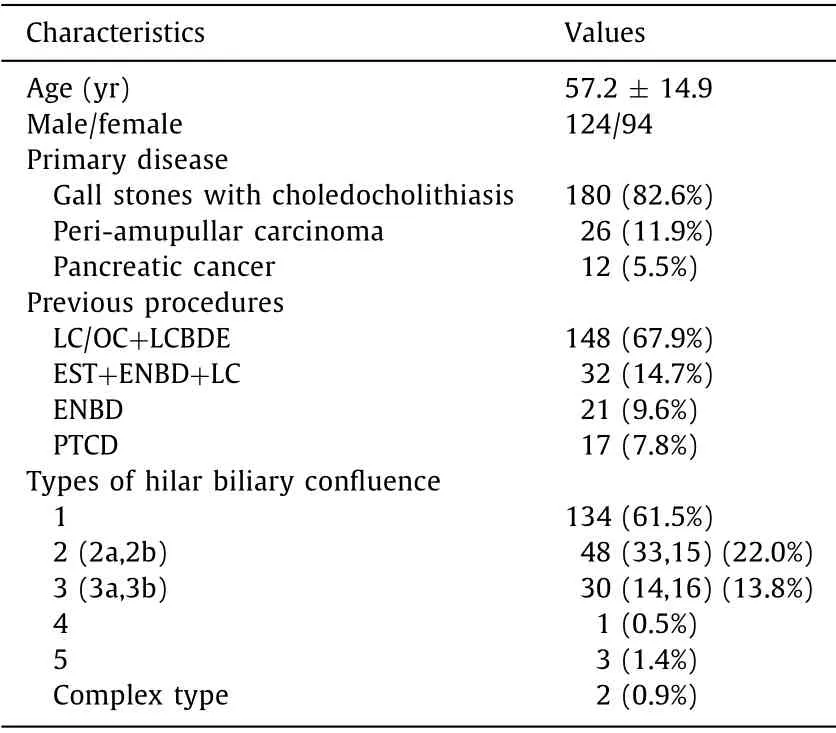
Table 1 Demographic and clinical characteristics.
Present study showed an incidence of the typical intrahepatic biliary system of 61.5% in the Chinese population.To the best of our knowledge,this study has the biggest sample size conducted in China’s mainland.Two early reports from China [ 2,3 ]that were based on cholangiograms from endoscopic retrograde cholangiopancreatography implied that the prevalence of normal type was 63%–66% in graft donors.Later on,Ji et al.[4]reported that normal biliary confluence pattern was seen in 53 (54.6%)out of the 97 patients with hilar cholangiocarcinmoma,based on CT biliary three-dimensional images.A recent meta-analysis reviewed all reported studies,enrolling 7514 patients [1],and reported that the prevalence of typical biliary anatomy in Europe,America,and Asia were 59.7%,58.1%,and 64.8%,respectively,implying similar epidemiology across three continents.However,Cucchetti et al.[1]pointed out that male donors presented normal anatomy more frequently than females (74% vs.55%).In the present study,we analyzed this difference between males and females but found that they had similar frequency in normal anatomy (74/124 vs.60/94).The discrepancy was probably due to the population selection bias.While the clinical relevance of extrahepatic biliary abnormalities is well described in the literature,especially as pancreaticobiliary duct maljunction inducing malignant biliary tumor [5],few data are available regarding the relevance of intrahepatic biliary abnormalities and malignant tumors.Herein,we assessed the prevalence of anomalous confluence types between benign and malignant diseasees (71/180 vs.13/38),but found no significant difference.
The common variations were type 2 and type 3 in the present study,accounting for 22% and 13.8% of patients.Along with previous report [1],type 2 was most common in the Chinese population,while type 3 was a dominant variation in Japanese and Caucasians.Although numerous variations were reported,trifurcation(type 2) has not yet been clarified in detail [ 1–4,6 ].As it is well known,the relationship between RPHD and right portal vein is important for cholangiocarcinoma.In order to distinguish their clinical relevance for surgeons,type 2 was sub-typed depending on the course of RPHD in present study,which was not reported before.In type 2a,accounting for 15.1% of patients,the RPHD runs a regular course,the right portal vein could disturb further dissecting RPHD while the surgical margin is positive for a Bismuth-Corlette Type IV hilar cholangiocarcinoma.However,in type 2b,accounting for 6.9% of patients,the RPHD runs ventrally and caudally to the right portal vein,which allows a straightforward approach for resection of RPHD at a more distal level [ 4,7 ].
The prevalences of type 3a and type 3b were 6.4% and 7.4% in the present study,respectively.For type 3a,the RPHD ran over the hilum,increasing the chance of right sectoral bile duct injury during left hepatic resections or harvest of the graft.To alleviate jaundice before the operation for patients with Bismuth-Corlette Type IIIb,both the RAHD and the RPHD should be drained.Drainage of RPHD to LHD with acute angulation increases the risk of bile stasis and repeated cholangitis.Due to the deep position,the stones in RPHD were difficult to remove and easy to miss.A total of 4197 patients with intrahepatic bile duct stones were investigated over the last century across China,and the residual stone rate of RPHD was 24.23% after surgery [8].In type 3b,the RPHD drainage into CHD was found in 1%–11% of people [1].This was a useful variation for hilar cholangiocarcinoma as described for type 2b.However,type 3b increases the difficulty in harvesting graft.
In conclusion,the present study enrolled the largest volume of patients in China,using specified cholangiography in different positions,thus proposing a more detailed hilar biliary confluence types.The typical anatomy was found in only 61.5% of patients.The most common variation was trifurcation,with a rate of 22%,followed by anomalous draining RPHD,with a rate of 13.8%.
Acknowledgments
We thank all the staff from the Radiology Department of the First Affiliated Hospital of Xi’an Jiaotong University for their help providing all the facilities to carry out this study.
CRediTauthorshipcontributionstatement
YuLi:Data curation,Formal analysis,Methodology,Writing -original draft.WeiZhang:Methodology,Writing - original draft,Writing - review & editing.HaoSun:Conceptualization,Supervision.Xue-MinLiu:Conceptualization,Supervision.YiLv:Conceptualization,Funding acquisition,Supervision,Writing - review &editing.
Funding
This study was supported by a grant from the National Natural Science Foundation of China (81470896).
Ethicalapproval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964DeclarationofHelsinkiand its later amendments.Informed consent was obtained from all participants prior to enrollment in the study.
Competinginterest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- MEETINGS AND COURSES
- Reply to: Contrast-enhanced ultrasonography for intrahepatic cholangiocarcinoma: A cost-effective alternative for low-resource settings
- Contrast-enhanced ultrasonography for intrahepatic cholangiocarcinoma: A cost-effective alternative for low-resource settings
- Transarterial chemoembolization as adjuvant treatment after surgery:The cure of huge hepatocellular carcinoma?
- RELEVANT CONTENT
- Prediction of Clostridium difficile infection based on gut microbial traits in patients with Clostridium difficile colonization
