Diagnostic performance of isolated-check visual evoked potential versus perimetry with blue-yellow in patients with open angle glaucoma
2021-05-10LiNaHuangChenLinPengHuang5QiuXiaXie2CaiXiaWang
Li-Na Huang,2*, Chen Lin,3,4*, Peng Huang5, Qiu-Xia Xie2, Cai-Xia Wang
Abstract
INTRODUCTION
Glaucoma is an optic neuropathy characterized by progressive loss of retinal ganglion cells (RGCs) and their axons, changes in optic disc topography[1-2], and associated defect of visual function[2-3]. Early detection is important to initiate treatment in the early stages of glaucoma and to avoid its natural progression to blindness[2]. Detection of the functional disorder of blue-yellow color vision would be a way for early detection of glaucoma[4-7]. Besides of the blue-yellow perimetry, a kind of subjective visual field examination, isolated-checked visual evoked potential (IC-VEP) is a recently developed objective test to detect the damage of RGCs by evaluating the function of the blue-yellow color vision signal transduction pathway[8-13]. The purpose of this study was to evaluate the clinical performance of the isolated-checked visual evoked potential (IC-VEP) in the detection of glaucoma and compared it to the blue-yellow perimetry (B/YP) and optical coherent tomography (OCT).
SUBJECTSANDMETHODS
ParticipantsSixty-six primary open angle glaucoma (POAG) eyes from 66 patients (including early, moderate and advanced glaucoma) were recruited from Shenzhen Aier Eye Hospital from January 2018 to January 2019. POAG was defined by the presence of characteristic glaucomatous optic disc changes and corresponding visual field defects in 24-II blue-on-yellow perimetry, together with increased intraocular pressure (>21 mmHg) and an open anterior chamber angle in gonioscopy. Secondary glaucoma (e.g. uveitic glaucoma) was excluded. Early glaucoma, moderate glaucoma and advanced glaucoma were graded according to the criteria of Hodapp-Anderson-Parrish (HAP)[2]. Thirty-five eyes of 35 healthy individuals were recruited from the same hospital from January 2018 to January 2019. All individuals showed no optic disc or RNFL abnormalities on clinical examination, and no history of retinal disease, eye surgery, laser procedures, diabetes mellitus or neurologic disease. The best-corrected visual acuity (BCVA) of these individuals were not worse than 20/40 and their spherical refractive error was within the range of -6.00 DS to +3.00 DS. This study was carried out in accordance with the tenets of the Declaration of Helsinki, and after the approval the Ethics Committee.
Isolated-checkedVisualEvokedPotentialIC-VEP examination was performed using the isolated grid pattern of Neucodia electrophysiologic instrument (Medconova Corp., Huzhou, China). The pupil of the examined eye was parallel to the center of the stimulus pattern and had a distance of 70 cm. The whole stimulus process was 96s, divided into 8 cycles. If significant noise or artifacts from the eye movement occurred during a cycle, the system rejected the extreme signals, and the measurements were automatically repeated and rerecorded. Each subject was examined twice, with an interval of more than 10min. The reliable results were included in the final analysis. The signal-to-noise ratio (SNR), defined as a circle of confidence in the radius of the fundamental component of the average amplitude ratio, was used for the judgment of glaucoma. If the SNR was less than 1, which meant the electrophysiologic response from the RGCs was not higher than the background noise, the abnormality of IC-VEP results was recorded for this test. IC-VEP test will be repeated after 10min if the abnormality results were found. The eye with two consecutive results of SNR ≤1 was recorded as glaucomatous eye (Figure 1).

Figure 1 Flow chart of the order of tests The tests of Slit lamp, OCT, visual field and IC-VEP were performed in sequence. At least 15min rest was arranged before VF and IC-VEP test to avoid the fatigue effects and to ensure the accuracy and reliability of these tests.
Blue-on-yellowPerimetryBlue-on-yellow perimetry was performed by 24-II blue-yellow total threshold procedure and SITA-standard program of Humphry 750 perimetry (Carl Zeiss Meditec, Inc. USA). Criteria for blue-yellow visual field abnormalities: 1) three or more adjacent points decreased in light sensitivity by 7 dB or more; 2) two or more adjacent points decreased in light sensitivity by 7 dB or more in one point and 10 dB or more in the other; 3) the difference in light sensitivity between two or more adjacent points above or above the horizontal line on the nasal side was 10 dB or more; 4) three or more adjacent points proofread less than 5%. The classification of glaucoma visual field was based on HAP standard.
SpectralDomainOpticalCoherenceTomographyThe parapapillary retinal nerve fiber layer(RNFL) thickness and GC-IPL thickness in macular zone were measured by the Cirrus SD-OCT (software version 5.0, Carl Zeiss Meditec, Dublin, CA, USA) using the optic disc and macular scan mode (200×200 A-scans covering an area of 6×6 mm2centered on the optic disc and macular zone). The requirement for image quality was signal strength >6. The average RNFL and GC-IPL thickness was recorded for analyzing.
StatisticalAnalysisStatistical analyses were performed using SPSS 24.0 (IBM Corp., New York, USA) and STATA 14.0 (Stata Corp., Texas, USA). The significance of the differences in age, refraction, gender, BCVA, intraocular pressure, and C/D ratio was determined by the independent-samplet-test and Chi-squared test. The sensitivity of IC-VEP, perimetry and OCT for detection of glaucoma was calculated; the agreement between IC-VEP, perimetry and OCT was calculated with kappa statistics[14].P<0.05 was considered statistically significant.
RESULTS
Totally 66 glaucomatous eyes from 66 POAG patients and 35 normal eyes from 35 healthy subjects were enrolled in this study: 30 eyes were assigned to the early glaucoma group, 36 eyes were assigned to the moderate/advanced glaucoma group,and 35 eyes were assigned to the control group. The demographic characteristics of the study participants are summarized in Table 1. The spherical equivalent and gender distribution were not significantly different between the normal and POAG groups (P>0.05). Compared to the normal group, the C/D ratio was significantly higher in the POAG groups, the average-RNFL thickness was significantly lower in the POAG groups (P<0.05).
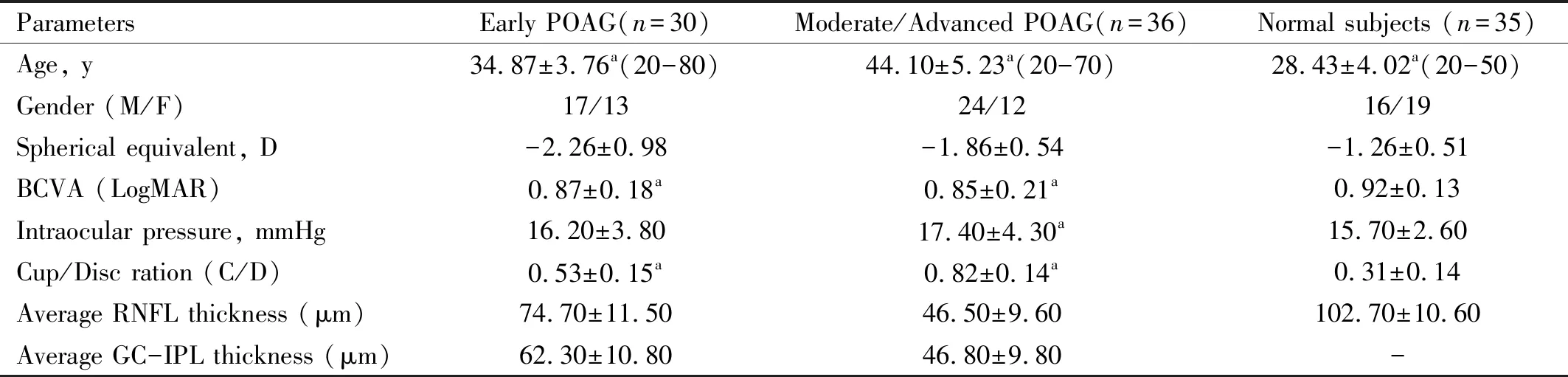
Table 1 Demographic information of the normal and POAG groups

Table 2 Performance of IC-VEP, blue-yellow perimetry and OCT in detection of POAG and normal subjects
PerformanceofIC-VEP,Blue-yellowPerimetryandOCTinDetectionofPOAGIn the early POAG group, 21 eyes (70.00%) on IC-VEP, 21 eyes (70.00%) on blue-yellow perimetry and 19 eyes (63.33%) on OCT were detected as abnormal. In the moderate/advanced POAG group, 31 eyes (86.11%) on IC-VEP, 33 eyes (91.67%) on blue-yellow perimetry and 32 eyes (88.89%) on OCT were detected as abnormal. In the normal subjects, 32 eyes (91.43%) on IC-VEP were detected as normal (Table 2). For both early and advanced glaucoma groups, the sensitivity of IC-VEP was 74.24%, and the specificity was 91.43%; the sensitivity of GC-IPL detection of OCT and blue-yellow perimetry were 77.27% and 81.82%, respectively.
AgreementBetweenIC-VEP,Blue-yellowPerimetryandOCTWithin the 30 eyes in early POAG group, 19 eyes were detected as abnormal by both OCT and IC-VEP (Kappa=0.851, 95%CI=0.530-0.958,P<0.001), 21 eyes were detected as abnormal by both blue-yellow perimetry and IC-VEP (Kappa=1.000, 95%CI=0.736-1.000,P<0.001), 19 eyes were detected as abnormal by both blue-yellow perimetry and OCT (Kappa=0.851, 95%CI=0.530-0.958,P<0.001), 19 eyes were detected as abnormal by IC-VEP , blue-yellow perimetry and OCT (Kappa=0.898, 95%CI=0.672-0.972,P<0.001) (Figure 2A). Within the 36 eyes in moderate/advanced POAG group, 31 eyes were detected as abnormal by both OCT and IC-VEP (Kappa=0.873, 95%CI=0.450-0.977,P<0.001), 31 eyes were detected as abnormal by both blue-yellow perimetry and IC-VEP (Kappa=0.721, 95%CI=0.271-0.921,P<0.001), 32 eyes were detected as abnormal by both blue-yellow perimetry and OCT (Kappa=0.842, 95%CI=0.366-0.972,P<0.001), 31 eyes were detected as abnormal by IC-VEP , blue-yellow perimetry and OCT (Kappa=0.813, 95%CI=0.410-0.949,P<0.001) (Figure 2B). Thus, in both groups, the results of IC-VEP was highly consistent with OCT and blue-yellow visual field test.

Figure 3 Two individuals with the abnormal results of IC-VEP A: a 51 years old male with early glaucoma (SNR: 0.44; average GC-IPL thickness: 72 μm; mean deviation of visual field test: -3.95 dB); B: a 48 years old female with advanced glaucoma (SNR: 0.61; average GC-IPL thickness:51 μm; mean deviation of visual field test: -21.21 dB).

Figure 2 Venn diagrams showed the agreement of IC-VEP, perimetry and OCT in the early POAG group (A) and the moderate/advanced POAG group (B) Red circle: GC-IPL detection of OCT; Green: IC-VEP, Blue: blue-yellow perimetry.
DISCUSSION
At present, there are more than 22 million glaucoma patients aged 40 years and above in China; by 2050, the glaucoma cases in China will increase to 25 million[15-16]. Patients in the early stage of glaucoma are often asymptomatic; when obvious symptoms are detected, a significant deficiency of visual function are already irreversible[2,17]. Thus, early diagnosis of glaucoma is an important step to preserve the visual function. OCT, as well as blue-yellow perimetry and IC-VEP have been developed for early detection of glaucoma by evaluating structure loss or functional disorder of RGCs, which is the characteristic pathological change of glaucomatous eyes[8,18].
Visual signals are transmitted by a special type of cell in the retina called the retinal ganglion cell (RGC). The RGCs can be categorized into M cells with larger cell bodies and P cells with smaller cell bodies[19]. The early manifestation of glaucoma is the function loss of the M-type RGCs[20]. The IC-VEP, which selectively stimulate M cell by separating grating pattern stimulation and evaluate the function of signal transduction pathway of M cells, would be a useful tool for the early detection of glaucoma[8-10]. In our study, we found that the sensitivity and specificity of IC-VEP for detecting early glaucoma were 70% and 91% respectively.
Studies showed that glaucoma patients have color vision disorders before the visual field changes, especially blue-yellow color vision disorders[7]. In our study, we also found that IC-VEP could objectively detect early glaucoma with the same sensitivity (70.00%) of blue-yellow perimetry. Compared to GC-IPL detection of OCT, IC-VEP would be more sensitive for the detection of early glaucoma (70.00%vs63.33%). For the moderate and advanced glaucoma, the performance of these 3 methods was similar. For early to advanced stages of glaucoma, the agreement between IC-VEP, blue-yellow perimetry and OCT is high.
There are limitations to our study. 1) It was a single-center clinical study with limited the sample size (around 30 cases in each group); 2) Since the examinations of blue-yellow perimetry and OCT were not performed in normal subjects, the specificity between IC-VEP, perimetry, and OCT cannot be compared. Multi-center study and longitudinal observation are still needed to further verify the clinical diagnostic efficacy of IC-VEP; 3) The age and BCVA of 3 groups (early glaucoma, moderate and advanced glaucoma and control group) did not match with each other, these factors may have slight influence on the results of IC-VEP, perimetry and OCT. Thus, the performance of the specificity of IC-VEP may be slightly different in the age-matched normal subjects.
To sum up, IC-VEP is an objective examination of visual function. By indirectly detecting the function loss of M-cell of RGCs, it can be used for early diagnosis of glaucoma. Regular monitoring of RGCs with IC-VEP may be likely to be pivotal to inform diagnosis decisions for suspected glaucoma patients.