Nie-pinching the spine, puncturing Sifeng (EX-UE 10)plus Chinese herbs for pediatric anorexia due to dysfunction of spleen in transportation:a randomized controlled trial
2021-04-23ZhouBowen周博文ChenMingming陈明明
Zhou Bo-wen (周博文), Chen Ming-ming (陈明明)
Fuzhou Traditional Chinese Medicine Hospital, Fujian University of Traditional Chinese Medicine, Fuzhou 350001, China
Abstract
Objective: To observe the clinical efficacy of Nie-pinching the spine, puncturing Sifeng (EX-UE 10) plus Chinese herbs in treating pediatric anorexia due to dysfunction of spleen in transportation.
Methods: A total of 64 kids were randomized into an observation group and a control group by the random number table method, with 32 cases in each group. Patients in both groups received Jian Pi Kai Wei (strengthening spleen and stomach)powder according to pattern differentiation of traditional Chinese medicine (TCM). In addition, patients in the observation group received Nie-pinching the spine and puncturing Sifeng (EX-UE 10). Nie-pinching the spine was applied twice a week, and puncturing Sifeng (EX-UE 10) was performed once a week, with 2 weeks counted as 1 course of treatment. After 2 courses of treatment, the body mass index (BMI), peripheral blood leptin level and the microelements Zn, Fe and Se were compared at different time points (before treatment, after the first and second courses of treatment),as well as the therapeutic efficacy and onset time.
Results: After 2 courses of treatment, 31 cases in each group were evaluated. After the 1st course and the 2nd course,the BMI and serum Zn, Fe and Se levels in the observation group increased significantly (all P<0.05), the leptin level decreased substantially (both P<0.05); the BMI in the control group showed a substantial rise (P<0.05), while the Zn, Fe and Se levels slightly increased showing no statistical significance (all P>0.05), and the leptin level decreased but the difference showed no statistical significance (P>0.05). After the 1st and the 2nd courses of treatment, the BMI, serum Zn,Fe and Se levels increased more significantly (all P<0.05), and the serum leptin level decreased more significantly (both P<0.05) in the observation group than in the control group. After the 2nd course, the total effective rate and recovery rate in the observation group were both higher than those in the control group (both P<0.05), together with a quicker onset time (P<0.05).
Conclusion: Nie-pinching the spine, puncturing Sifeng (EX-UE 10) plus Chinese herbs is effective for pediatric anorexia due to dysfunction of spleen in transportation. It can decrease leptin, increase Zn, Fe and Se levels, alleviate apositic symptoms and increase BMI in the kids.
Keywords: Acupuncture Therapy; Massage; Pediatric Massage (Tuina); Chiropractics (Traditional Chinese Medicine); Point,Sifeng (EX-UE 10); Anorexia; Dysfunction of Spleen in Transportation; Randomized Controlled Trials
Anorexia is a common disease in pediatric department,mainly manifesting as a long-term poor appetite,reduced food intake and even food refusal. Latest research showed the incidence rate of anorexia in children between 0 and 3 years was 12% to 34%[1].Without a proper treatment, it may lead to malnutrition,low immunity, growth retardation, or even cause rickets and iron-deficiency anemia, which affect children’s physical and mental health[2-3]. Current Western medicine treatments are focused on supplementing microelement Zn, or gastric motility drugs (such as domperidone), while showing limited effect for patients with disorders of digestion and absorption[4]. Therefore,seeking an effective and safe treatment for pediatric anorexia is of great importance and an urgent need in present time. Based on the holistic view of traditional Chinese medicine (TCM) and stressing the regulation of spleen function, we used Nie-pinching the spine,puncturing Sifeng (EX-UE 10) plus Chinese herbs to treat pediatric anorexia due to dysfunction of spleen in transportation, and the report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria for pediatric anorexia
The Western medicine criteria for pediatric anorexia referred theDiagnosis and Treatment of Feeding Disorders in Infants, Toddlers, and Young Childrenby Chatoor I[5]. TCM pattern differentiation criteria referred the dysfunction of spleen in transportation in thePediatrics in Chinese Medicine[6]. Main symptoms: loss of appetite, aversion to or refusal of food; combining symptoms: lusterless complexion, moderate spirit,tastelessness, occasional salivation, belching and hiccup,nausea, loose stool, a thin red tongue with thin white or greasy coating, soft pulse, thin red superficial veins on index finger. Diagnosis can be made with 4 or more main and combining symptoms, together with the manifestations of tongue, pulse and superficial veins on index finger.
1.2 Inclusion criteria
Aged between 1 and 6 years old; disease lasted for 3 months or more; without using medicine affecting appetite or for anorexia; informed consented by children’s parents.
1.3 Exclusion criteria
Anorexia nervosa; with organic disorders, or other serious heart, liver or kidney diseases; with mental diseases or retardation.
1.4 Drop-out criteria
Cases failed to complete the whole process and quit halfway due to various reasons, including the usage of other medicine for pediatric anorexia or drugs affecting appetite, or proposed by children’s parents, or regarded as not suitable to continue the research.
1.5 Statistical methods
Data were processed by SPSS version 20.0 software by specific staff. Measurement data were expressed as mean ± standard deviation (±s), with independent samplet-test ort’-test used for between-group comparison and pared-samplet-test for intra-group comparison. Enumeration data were expressed as frequency or rate, and Chi-square test was used for percentage comparison.P<0.05 indicated statistical significance.
1.6 General data
This research had won approval of the Ethics Committee of Fuzhou Traditional Chinese Medicine Hospital, Fujian University of Traditional Chinese Medicine (No. 2018-017-02). Anorexia children aged between 1 and 6 years old were recruited between June 2018 and June 2019 in Fuzhou Traditional Chinese Medicine Hospital, Fujian University of Traditional Chinese Medicine. Cases were numbered from 1 to 64.Then chose any line or row from a random number table to generate 64 random numbers from 00 to 99. Cases with odd numbers were divided into the observation group, and those with even numbers were divided into the control group. There were 32 cases in each group (for uneven case numbers between the two groups, rechecked the random number table, and adjusted the case number in each group according to a certain randomization method). During the research process, 1 case lost to visit in the observation group during the 1st course of treatment lost visit (home moving); 1 case in the control group suspended research during the 2nd course of treatment (took other medicine affecting appetite). Therefore, there were 31 cases in each group evaluated at the end of the 2nd treatment course.Between-group comparison of the general data showed no statistical significance (allP>0.05), indicating the comparability (Table 1).
2 Treatment Methods
2.1 Control group
Patients in the control group were treated with Jian Pi Kai Wei (strengthening spleen and stomach) powder prepared by our hospital.
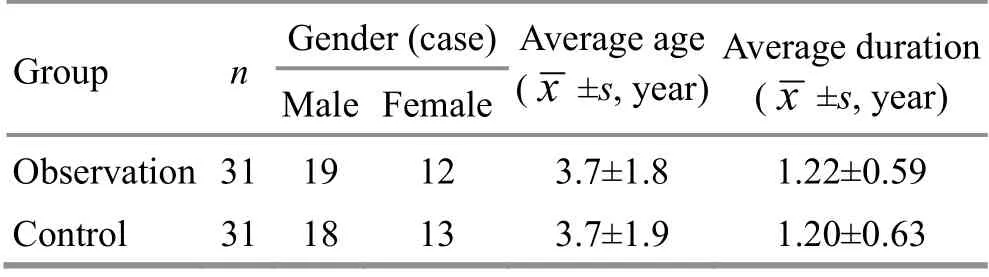
Table 1. Comparison of the general data between the two groups
Ingredients:Dang Shen(Radix Codonopsis) 15 g,Zhi Huang Qi(Radix Astragali Preparata) 15 g,Bai Zhu(Rhizoma Atractylodis Macrocephalae) 10 g,Fu Ling(Poria) 10 g,Chen Pi(Pericarpium Citri Reticulatae) 10 g,ginger-processedBan Xia(Rhizoma Pinelliae Preparata)10 g,Mu Xiang(Radix Aucklandiae) 6 g,Sha Ren(Fructus Amomi) 6 g,Shen Qu(Massa Medicata Fermentata) 10 g,Shan Zha(Fructus Crataegi) 10 g,Mai Ya(Fructus Hordei Germinatus) 15 g, andZhi Gan Cao(Radix Glycyrrhizae Preparata) 3 g. Put all herbs in 400 mL cold water for 30 min. After bringing to the boil, the herbs were brewed with mild fire for 30 min to concentrate water into 150 mL decoction. Then repeated the same process and mixed the decoction. The decoction was taken separately 1 h after breakfast and dinner, 50 mL each time for children between 1 and 2 years old, 100 mL for children between 3 and 4 years old, 150 mL for children between 5 and 6 years old. A total of 2 courses of treatment (4 weeks) were taken.
2.2 Observation group
Nie-pinching the spine and puncturing Sifeng(EX-UE 10) were added in the observation group on the basis of Chinese herbal treatment in the control group.2.2.1 Puncturing Sifeng (EX-UE 10)
The child turned the palm up, Sifeng (EX-UE 10) are located at the midpoint of the proximal finger crease from the second to the fifth finger of both hands (8 in total). After routine sterilization, punctured Sifeng(EX-UE 10) on both hands with a three-edge needle by 0.5 mm, then squeezed a little yellow or transparent mucus or blood. Then sterilized the spots with dry cotton balls, and pressed the points for a while (Figure 1 and Figure 2). Such treatment was given once a week, 2 weeks as 1 course, and the whole treatment lasted for 2 courses.
2.2.2 Nie-pinching the spine
Children laid on their back. Held the back skin with the finger pulps of the thumbs (backward), index and middle fingers (forward), then twisted backward with the index and middle fingers, pushed forward with the thumb from Changqiang (GV 1) to Dazhui (GV 14), and repeated for 10 times. Perpendicularly lifted the skin with a strong force when pushing to Pishu (BL 20) and Weishu (BL 21),(Figure 3). Such treatment was given twice a week, a succession of 2 weeks as 1 course, and the whole treatment lasted for 2 courses.

Picture 1. Puncturing Sifeng (EX-UE 10) with a three-edge needle

Picture 2. Squeezed little mucus or blood after puncturing

Picture 3. Nie-pinching the spine with finger pulps of the thumb, index and middle finger
3 Therapeutic Efficacy Evaluation
3.1 Observation items
The body mass index (BMI), the leptin level and concentrations of Zn, Fe and Se in peripheral blood were measured before treatment and after the 1st and the 2nd courses of treatment. After treatment, the clinical efficacy (clinical recovery rate and total effective rate) as well as the onset time were compared.
3.2 Therapeutic efficacy criteria[6]
Therapeutic efficacy evaluation referred theGuiding Principles for Clinical Study of New Chinese Medicines[7],and mainly compared the food intake and appetite with healthy children of the same age group.
Clinical recovery: The food intake and appetite were recovered to a normal level.
Markedly effective: Obvious improvement of the appetite, and the food intake was recovered to 3/4 of the normal level.
Effective: Improvement of the appetite and food intake, while not reached to the 3/4 of the normal level.
Invalid: No improvement of the appetite and food intake.
3.3 Supplementation
In this research, the observation group was treated with additional Nie-pinching the spine and puncturing Sifeng (EX-UE 10) on the basis of the treatment in the control group. Doctors only knew the intervention and grouping information, but didn’t participate in data recording and statistical process. Moreover,communication among doctors, result recorders and statistician were forbidden to ensure an independent working environment to guarantee a objective and scientific result.
3.4 Results
3.4.1 Comparison of the clinical efficacy
The clinical recovery rate was 38.7% in the observation group, and 25.8% in the control group. The clinical recovery rate in the observation group was substantially higher than that in the control group, and the betweengroup comparison showed statistical significance(P<0.05). The total effective rate was 96.8% in the observation group, and 83.9% in the control group, and the between-group comparison showed statistical significance (P<0.05), (Table 2).
3.4.2 Comparison of the onset time after treatment
Onset meant an improvement in appetite and food intake (at least reached the level of ‘effective’ in the therapeutic efficacy criteria). Illustration: only counted the effective cases at each time point, and cases showed effective at the last time point wouldn’t be included repeatedly. The total effective rate at the 1st and the 2nd weeks in the observation group was 19.4% and 35.5%,respectively. Between-group comparison of the onset time showed statistical significance (bothP<0.05) at the same time point (Table 3).
3.4.3 Comparison of BMI, serum leptin and Zn, Fe, Se levels at each time point
Intra-group comparison showed that after the 1st and the 2nd courses of treatment, the BMI and serum Zn, Fe and Se levels increased significantly (allP<0.05), the leptin level dropped significantly (P<0.05) in the observation group. Intra-group comparison showed after the 1st and the 2nd courses of treatment, the BMI increased significantly in the control group (bothP<0.05).Serum Zn, Fe and Se levels increased, and the leptin levels decreased but without statistical significance (allP>0.05). After the 1st and the 2nd courses of treatment,the BMI and serum Zn, Fe, Se levels in the observation group were substantially higher than those in the control group (allP<0.05), and the leptin level was lower than that in the control group (bothP<0.05), (Table 4).
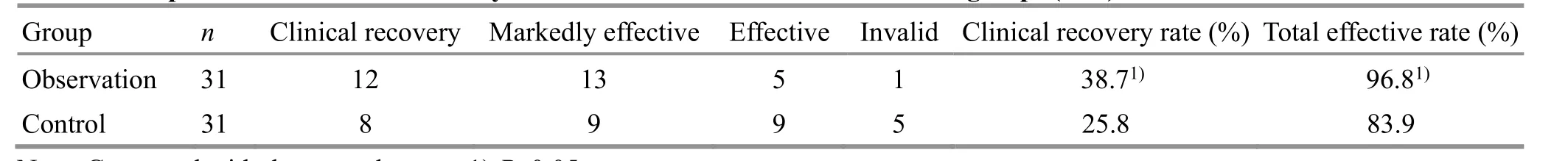
Table 2. Comparison of the clinical efficacy at the end of treatment between the two groups (case)
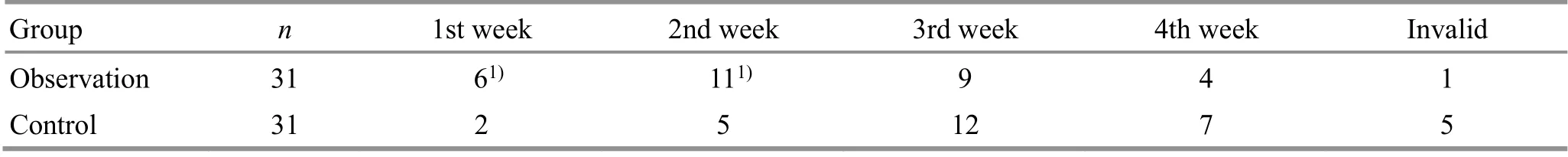
Table 3. Comparison of the onset time between the two groups (case)
Table 4. Comparison of BMI, and serum leptin and Zn, Fe, Se levels at each time point in the two groups ( ±s)
Note: Intra-group comparison, 1) P<0.05; between-group comparison, 2) P<0.05
Group n Time point BMI (kg/m2) Leptin (ng/L) Zn (µmol/L) Fe (µmol/L) Se (µmol/L)Before treatment 13.65±1.17 3.53±0.73 47.87±4.31 5.21±1.11 0.081±0.005 Observation 31After 1-course treatment 14.53±0.921)2) 3.09±0.611)2) 67.65±9.471)2) 6.90±1.371)2) 0.178±0.0091)2)After 2-course treatment 15.28±0.831)2) 2.17±0.431)2) 99.27±12.821)2) 9.28±1.631)2) 0.216±0.0141)2)Before treatment 13.69±1.26 3.54±0.72 48.12±4.27 5.19±1.12 0.081±0.006 Control 31After 1-course treatment 14.07±0.841) 3.35±0.67 53.93±7.37 6.21±1.23 0.124±0.008 After 2-course treatment 14.74±0.511) 3.19±0.62 75.45±9.27 7.89±1.34 0.176±0.012
4 Discussion
Pediatric anorexia pertains to Na Dai (poor appetite),Shang Shi (food damage disease), Wu Shi (anorexia) in TCM. Due to TCM theory, spleen deficiency is a common pattern in children, and the lactation and feeding require a regular time and restriction. However, improper diet is usually caused by parents’ over-caring, and children may overeat greasy or cold food. Those improper feeding habit may harm the spleen and stomach, consequently,dysfunction of the spleen and stomach will give rise to the anorexia symptoms such as loss of appetite and reduction of food intake[8-9]. A long-term anorexia will weaken the immune system, causing malnutrition and weakness, or even hindering children’s intelligence development and growth[10]. Current Western medicine treatment for pediatric anorexia remains unsatisfactory.It’s usually a difficult disease to treat with a long course.Therefore, a safe and effective treatment for pediatric anorexia is an urgent need in clinical practice.
Modern research showed puncturing Sifeng (EX-UE 10)can accelerate gastric emptying, and increase pepsinia secretion to improve appetite[11]. Besides, it can also inhibit leptin. Leptin is a peptide hormone with protein structure secreted by fat tissue. It can bind leptin receptor in hypothalamus to inhibit the secretion of neuropeptide Y, which may reduce food intake and increase energy consumption[12-13]. Nie-pinching the spine is a characteristic external therapy for pediatric anorexia in TCM. Research showed Nie-pinching the spine can regain the coordination between sympathetic and parasympathetic nerves, enhance gastric peristalsis,improve gastrointestinal blood circulation and lymphatic return, and thus promote digestive juice secretion, lift serum Zn, Fe and Se concentrations, and improve intestinal absorption to enhance appetite[14-18]. Besides,due to TCM pattern differentiation, we used herbal decoction to invigorate spleen and stomach in children of spleen deficiency. In the decoction,Dang ShenandHuang Qiare the main herbs to tonify qi and fortify the spleen helping transportation and transformation.Bai Zhu,Fu Ling,Chen Pi,Ban Xia,Mu XiangandSha Rencan fortify the spleen to dispel dampness, regulate qi to harmonize the stomach; complemented byShen Qu,Shan ZhaandMai Yawhich can promote digestion. The whole decoction aimed to strengthen the spleen and improve appetite, and harmonize the middle Jiao(energizer).
Our research showed that the clinical recovery rate and total effective rate in the observation group were higher than those in the control group, and betweengroup comparison showed statistical significance (bothP<0.05). It indicated that Nie-pinching the spine,puncturing Sifeng (EX-UE 10) plus Chinese herbs or Chinese herbs alone can improve the symptoms in children with anorexia due to dysfunction of spleen in transportation, while the integrated treatment showed more significant clinical efficacy than Chinese herbs alone. Moreover, the onset time in the observation group was earlier than that in the control group, and between-group comparison showed statistical significance (bothP<0.05), indicating that the children in the observation group got a quicker recovery in symptoms.
As for BMI, and the serum leptin and Zn, Fe, Se concentrations, intra-group comparison showed statistical significance in the observation group (allP<0.05). In the control group, except for BMI, the intragroup comparison showed no statistical significance (allP>0.05). After the 1st and the 2nd courses of treatment,between-group comparison of the BMI, and the serum Zn, Fe, Se and leptin concentrations showed statistical significance (allP<0.05), showing a better result in the observation group. It indicated that herbal decoction alone was inferior to the combination of Nie-pinching the spine, puncturing Sifeng (EX-UE 10) and herbal decoction in increasing the serum Zn, Fe, Se concentrations and inhibiting serum leptin. It may be accounted for the regulation of yin-yang, qi-blood and functions of Zang-fu organs by Nie-pinching the spine and puncturing Sifeng (EX-UE 10)[19-21], thus, the food essence can be transformed and qi movement can be balanced.
Above all, Nie-pinching the spine, puncturing Sifeng(EX-UE 10) plus Chinese herbs is effective for pediatric anorexia due to dysfunction of spleen in transportation.However, such treatment has some limitations. For example, children may fear puncture and Chinese herbs,which may restrict its acceptance. Chinese massage manipulation like Nie-pinching the spine is hard to standardize the intensity and location. Besides, current researches usually focused on clinical study and lacked experimental test and evidence. Its mechanism still requires further investigation.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
This work was supported by Fuzhou Young and Middleaged Scientific Research Project (福州市中青年科学研究项目, No. 2019-S-wq11).
Statement of Informed Consent
Informed consent was obtained from the guardians of the recruited children in this study.
Received: 30 November 2019/Accepted: 11 May 2020
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Review of systematic reviews of acupuncture for diabetic peripheral neuropathy
- Clinical observation on spleen-invigorating and qibenefiting pediatric massage for treating recurrent respiratory tract infection in children with cerebral palsy due to qi deficiency of spleen and lung
- Acupoint catgut-embedding therapy as promising treatment for non-alcoholic fatty liver disease
- Clinical observation of electroacupuncture with different frequencies for migraine without aura
- Warm needling moxibustion plus PKP for vertebral compression fracture due to kidney deficiency and blood stasis: a randomized controlled trial
- Evaluation of the prevention and treatment effects of acupuncture-moxibustion for Alzheimer disease based on various mouse models
