Clinical observation of electroacupuncture with different frequencies for migraine without aura
2021-04-23GongJie龚杰XuMimi徐密密PanYaying潘亚英
Gong Jie (龚杰), Xu Mi-mi (徐密密), Pan Ya-ying (潘亚英)
Xiaoshan Hospital of Traditional Chinese Medicine in Hangzhou, Zhejiang Province, Hangzhou 311200, China
Abstract
Objective: To observe the clinical efficacy of electroacupuncture (EA) with different frequencies in treating migraine.
Methods: Ninety patients with migraine were divided into a low frequency electroacupuncture (LF-EA) group, a high frequency electroacupuncture (HF-EA) group and a variable frequency electroacupuncture (VF-EA) group by the random number table method. Shuaigu (GB 8), Hegu (LI 4), Waiguan (TE 5), Taichong (LR 3), Taiyang (EX-HN 5), Fengchi (GB 20)and Ashi points were selected for all three groups. After achieving needling sensation (Deqi), the LF-EA group received 2 Hz continuous wave EA stimulation; the HF-EA group received 100 Hz continuous wave EA stimulation, and the VF-EA group received 2 Hz/100 Hz sparse-dense wave EA stimulation. The EA stimulation lasted for 30 min in all the three groups,once a day, 10 times as a course, and the clinical efficacy was evaluated after 2 consecutive courses of treatment.
Results: After treatment, the total effective rates in the LF-EA group, HF-EA group and VF-EA group were 77.7%, 83.3%and 93.3%, respectively. The difference in total effective rate between the LF-EA and HF-EA groups was not statistically significant (P>0.05), but the total effective rate was significantly higher in the VF-EA group than in the LF-EA and HF-EA groups (both P<0.01). After treatment, the headache scores significantly decreased in all three groups (all P<0.01). The difference in headache score between the LF-EA and HF-EA groups was not statistically significant (P>0.05), while the score was significantly lower in the VF-EA group than in the LF-EA and HF-EA groups (both P<0.01).
Conclusion: VF-EA (2 Hz/100 Hz), compared with LF-EA (2 Hz) and HF-EA (100 Hz), shows superior clinical efficacy in treating migraine.
Keywords: Acupuncture Therapy; Electroacupuncture; Frequency; Pain Measurement; Migraine
Migraine is a neurological disease mainly caused by vasomotor dysfunction, often manifested as unilateral or bilateral pulsatile headache[1]. The disease is characterized by periodic recurrent attacks and is often accompanied by nausea, dizziness, sweating, vomiting,palpitations and other uncomfortable symptoms during severe attacks. The cause of the disease is complicated,mostly considered to be related to cerebral vasculopathy,mental tension, endocrine, genetic factors,menstruation and other factors in modern clinical medicine[2]. The prevalence of migraine in China is 9.3%according to the epidemiological survey and long-term drug treatment can lead to a variety of adverse events[3-4], seriously affecting patients’ normal life.
Acupuncture has been widely used to treat migraine clinically and shown definite efficacy in a series of studies[5-7]. Electroacupuncture (EA) has a good analgesic effect, which is affected by many parameters, mainly including frequency, intensity, waveform and wave width[8-10]. Previous studies have reported the efficacy of EA with different frequencies in the treatment of migraine, but there is a lack of comparative observation.Thus, a prospective randomized controlled trial including 90 patients was performed in this study to compare the clinical efficacy of different frequencies EA stimulation in treating migraine.
1 Clinical Materials
1.1 Diagnostic criteria
The diagnostic criteria of migraine without aura referred the International Headache Society (2004)[11]:recurrent attacks more than 5 times in half a year; each single attack lasts for 4-72 h; headache has at least two of the following characteristics: ① pain occurs on the side of the head (unilateral or bilateral); ② the pain is pulsatile; ③ when the headache is serious, can only stay in bed and cannot carry out any normal activities;④ headache gets worse during strenuous activities;headache is accompanied by at least one of the following:① nausea and/or vomiting; ② phonophobia and photophobia.
1.2 Inclusion criteria
Those who met the above diagnostic criteria for migraine; in ictal phase; aged 18-70 years old; signed informed consent.
1.3 Exclusion criteria
Those who were pregnant or during lactation; with serious complications; with mental illness; headache caused by other diseases.
1.4 Criteria for elimination and dropout
Those who were found not meet the inclusion criteria after inclusion; did not receive treatment as prescribed;dropped out without completing all the treatment; used concomitant medication or other treatments, resulting in inability to determine the therapeutic effect.
1.5 Statistical analysis
The data were analyzed by SPSS version 24.0 software.All measurement data were expressed as mean ±standard deviation (±s). One-way analysis of variance was used for comparison among groups. For betweengroup comparisons, least significant difference or Dunnett's T3 test was performed when homogeneous or non-homogeneous variance, respectively, was found in the data. The counting data were expressed as percentage and tested by Chi-square test.P<0.05 was taken as statistically significant.
1.6 General data
A total of 90 patients were included. All of them were recruited from outpatients attending the Acupuncturemoxibustion Department of Xiaoshan Hospital of Traditional Chinese Medicine in Hangzhou, Zhejiang Province between December 2017 and October 2019.Patients were randomly assigned into three groups by the random number table method. No dropout cases were observed during treatment. There were no statistically significant differences across the three groups in baseline characteristics, confirming that the three groups were appropriately comparable (Table 1).
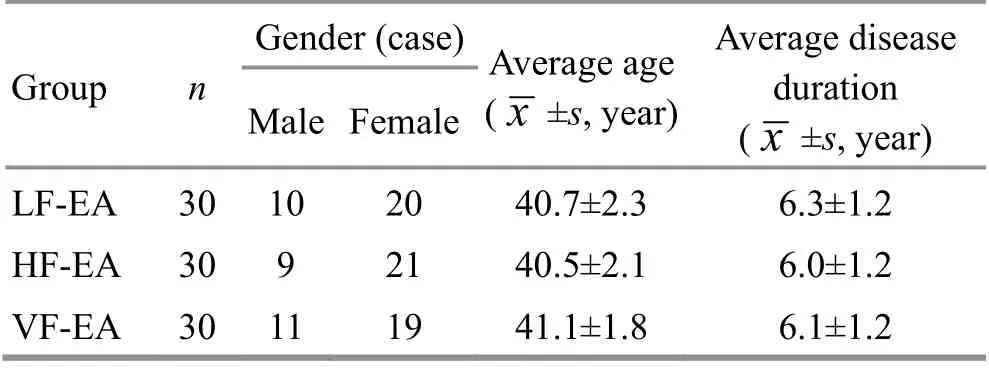
Table 1. Baseline characteristics among the three groups
2 Treatment Methods
The selected acupoints of the three groups were the same, but the EA stimulation parameters were different:2 Hz continuous wave was used in the LF-EA group,100 Hz continuous wave was used in the HF-EA group,and 2 Hz/100 Hz sparse-dense wave was selected in the VF-EA group.
Acupoints: Shuaigu (GB 8), Hegu (LI 4), Waiguan (TE 5),Taichong (LR 3), Taiyang (EX-HN 5), Fengchi (GB 20) and Ashi point.
Methods:Hwato brand disposable acupuncture needles (0.25 mm in diameter, 40 mm in length) and HANS-200A EA apparatus were used. Following needle insertion and achieving needling sensation (Deqi), one pair of electrodes from the EA apparatus were attached to the needle handles at local Ashi points on the affected side, and the other pair of electrodes were attached to the needle handles at Hegu (LI 4) and Waiguan (TE 5) on the affected side. EA stimulation lasted for 30 min with a mild current intensity without causing pain. Patients received the treatment once per day, 10 times as a course, and the clinical efficacy was evaluated after 2 consecutive courses.
3 Observation of Therapeutic Efficacy
3.1 Observation items
The headache score was evaluated by the headache attack times, headache severity, headache duration and concomitant symptoms of migraine[12].
The headache attack times: 6 points for more than 5 attacks per month, 4 points for 3-4 attacks per month,and 2 points for 2 or less attacks per month.
The headache severity during migraine attack: 6 points for those who needed to stay in bed; 4 points for those who could not work normally; 2 points for those whose work wasn’t affected.
The headache duration of each attack: 6 points for headache lasting more than 2 d; 4 points for headache lasting 12 h to 2 d; 2 points for headache duration less than 12 h.
Concomitant symptoms: 3 points for 3 or more items of nausea, vomiting, photophobia and phonophobia;2 points for only 2 concomitant symptoms; 1 point for only 1 concomitant symptom.
Headache score: The headache score was calculated by adding the above points according to theGuiding Principles for Clinical Study of New Chinese Medicines[13].The headache score, ≥17, ≥12 but <17, ≥7 but <12, and<7, was defined as severe headache, moderate headache, mild headache and no headache, respectively.
3.2 Criteria for therapeutic efficacy
The efficacy index was calculated by Nimodipine method[14], and the clinical efficacy was evaluated according to the efficacy index. The efficacy index =(Before-treatment headache score - After-treatment headache score) ÷ Before-treatment headache score ×100%.
Markedly effective: The efficacy index was ≥50%.
Effective: The efficacy index was ≥20%, but <50%.
Invalid: The efficacy index was less than 20%.
3.3 Results
3.3.1 Comparison of the therapeutic efficacy
The data after treatment showed that EA was effective in the treatment of migraine. The difference in total effective rate between the LF-EA and HF-EA groups in the pairwise comparison was not statistically significant(P>0.01), but the rate was significantly higher in the VFEA group than in the LF-EA and HF-EA groups (bothP<0.01), (Table 2).
3.3.2 Comparison of the headache score
The headache scores of the three groups decreased significantly after treatment (allP<0.01). The difference in headache score between the LF-EA and HF-EA groups in the pairwise comparison was not statistically significant (P>0.05), but the score was significantly lower in the VF-EA group than in the LF-EA and HF-EA groups(bothP<0.01), (Table 3).
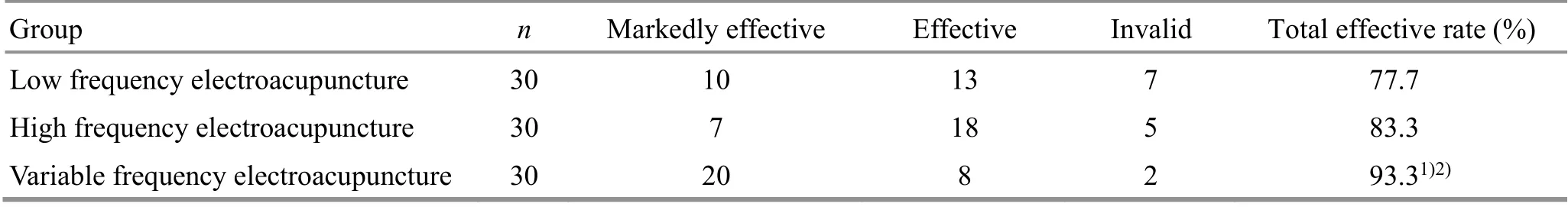
Table 2. Comparison of the total effective rate among the three groups (case)
Table 3. Comparison of the headache score among the three groups before and after treatment ( ±s, point)
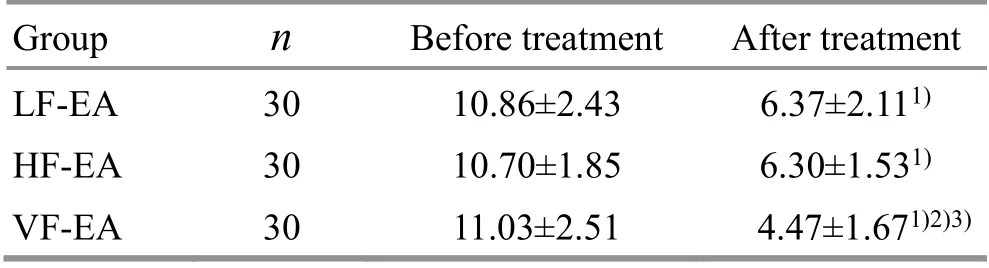
Table 3. Comparison of the headache score among the three groups before and after treatment ( ±s, point)
Note: LF-EA=Low frequency electroacupuncture group; HFEA=High frequency electroacupuncture group; VF-EA=Variable frequency electroacupuncture group; compared with the same group before treatment, 1) P<0.01; compared with the LF-EA group after treatment, 2) P<0.01; compared with the HF-EA group after treatment, 3) P<0.01
Group n Before treatment After treatment LF-EA 30 10.86±2.43 6.37±2.111)HF-EA 30 10.70±1.85 6.30±1.531)VF-EA 30 11.03±2.51 4.47±1.671)2)3)
4 Discussion
Migraine belongs to the category of ‘brain wind’ or‘head wind’ in traditional Chinese medicine (TCM). Blood stasis in the head meridians will lead to the loss of nourishment of the brain and orifices, which can result in pain. The etiology of migraine mainly involves exogenous and endogenous pathogens. Wind is the predominant exogenous pathogen, while endogenous pathogens are mainly related to liver, spleen and kidney.Ascendant hyperactivity of liver yang can obstruct the clear orifices. Failure of splenic transportation and transformation will lead to turbid phlegm, which will in turn cloud the orifices; the deficiency of kidney essence will inhibit the sea of marrow which can result in the loss of nourishment of the brain. Thus, headache occurs. At present, the pathogenesis of migraine is not completely clear in Western medicine, and it is believed that the direct cause is mainly the dysfunction of cerebral vasodilatation and vasoconstriction.
Acupuncture can unblock the meridians and regulate the function of the human body. Modern studies have shown that acupuncture has a good analgesic effect[15].Migraine belongs to Shaoyang headache according to TCM syndrome differentiation, and the treatment should focus on pacifying liver, subduing yang and dispelling wind for relieving pain. Therefore, the acupoints on Gallbladder Meridian of Foot Shaoyang and Liver Meridian of Foot Jueyin are mainly selected for migraine treatment. Shuaigu (GB 8), Waiguan (TE 5), Taichong(LR 3) and Fengchi (GB 20) can pacify liver to subdue yang and unblock the meridians to relieve pain. Taiyang(EX-HN 5) and Ashi points, located in the affected areas,can exert a good analgesic effect. The compatibility of these acupoints can achieve the goal of treating migraine.
Frequency is an important parameter of EA, and it can affect the therapeutic efficacy. Previous studies have shown that EA is effective for migraine. The analgesic
effect exerted by EA can be explained by the regulation of cerebral vasodilation and vasoconstriction[16-17], which can in turn improve cerebral circulation and release analgesic substances[18-19]. Different frequencies of EA stimulation promote the releases of different analgesic substances[20], resulting in different analgesic effects. The results of this study showed that 2 Hz, 100 Hz and 2 Hz/100 Hz were all effective in EA treatment of migraine, and could significantly reduce the headache score. 2 Hz/100 Hz sparse-dense wave showed better effect in reducing headache score and should therefore be regarded as the optimal parameter compared with the 2 Hz and 100 Hz continuous wave EA stimulation[21].At present, there is no standard for the use of EA in clinic. The results of this study may provide theoretical basis for EA treatment of migraine. However, this study only observed the therapeutic effect of EA on migraine from the view of stimulation frequency, and what kind of EA parameter combination can achieve the best effect in the treatment of migraine needs further study.
Conflict of Interest
There is no potential conflict of interest in this article.
Acknowledgments
This work was supported by Policy Guidance Project of Major Social Science and Technology Planning, Xiaoshan District of Hangzhou (杭州市萧山区社会重大科技计划政策引导项目).
Statement of Informed Consent
Informed consent was obtained from all individual participants.
Received: 23 February 2020/Accepted: 9 June 2020
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Review of systematic reviews of acupuncture for diabetic peripheral neuropathy
- Clinical observation on spleen-invigorating and qibenefiting pediatric massage for treating recurrent respiratory tract infection in children with cerebral palsy due to qi deficiency of spleen and lung
- Acupoint catgut-embedding therapy as promising treatment for non-alcoholic fatty liver disease
- Warm needling moxibustion plus PKP for vertebral compression fracture due to kidney deficiency and blood stasis: a randomized controlled trial
- Evaluation of the prevention and treatment effects of acupuncture-moxibustion for Alzheimer disease based on various mouse models
- Effects of moxibustion on the P2X7R/STAT3/VEGF pathway in rats with colitis-associated colon cancer
