R2 * value derived from multi-echo Dixon technique can aid discrimination between benign and malignant focal liver lesions
2021-04-17GuangZiShiHongChenWeiKeZengMingGaoMengZhuWangHuiTingZhangJunShen
Guang-Zi Shi, Hong Chen, Wei-Ke Zeng, Ming Gao, Meng-Zhu Wang, Hui-Ting Zhang, Jun Shen
Abstract
BACKGROUND R2 * estimation reflects the paramagnetism of the tumor tissue, which may be used to differentiate between benign and malignant liver lesions when contrast agents are contraindicated.
AIM To investigate whether R2 * derived from multi-echo Dixon imaging can aid differentiating benign from malignant focal liver lesions (FLLs) and the impact of 2 D region of interest (2 D-ROI) and volume of interest (VOI) on the outcomes.
METHODS We retrospectively enrolled 73 patients with 108 benign or malignant FLLs. All patients underwent conventional abdominal magnetic resonance imaging and multi-echo Dixon imaging. Two radiologists independently measured the mean R2 * values of lesions using 2 D-ROI and VOI approaches. The Bland–Altman plot was used to determine the interobserver agreement between R2 * measurements.Intraclass correlation coefficient (ICC) was used to determine the reliability between the two readers. Mean R2 * values were compared between benign and malignant FFLs using the nonparametric Mann–Whitney test. Receiver operating characteristic curve analysis was used to determine the diagnostic performance of R2 * in differentiation between benign and malignant FFLs. We compared the diagnostic performance of R2 * measured by 2 D-ROI and VOI approaches.
RESULTS This study included 30 benign and 78 malignant FLLs. The interobserver reproducibility of R2 * measurements was excellent for the 2 D-ROI (ICC = 0 .994 )and VOI (ICC = 0 .998 ) methods. Bland–Altman analysis also demonstrated excellent agreement. Mean R2 * was significantly higher for malignant than benign FFLs as measured by 2 D-ROI (P < 0 .001 ) and VOI (P < 0 .001 ). The area under the curve (AUC) of R2 * measured by 2 D-ROI was 0 .884 at a cut-off of 25 .2 /s, with a sensitivity of 84 .6 % and specificity of 80 .0 % for differentiating benign from malignant FFLs. R2 * measured by VOI yielded an AUC of 0 .875 at a cut-off of 26 .7 /s in distinguishing benign from malignant FFLs, with a sensitivity of 85 .9 %and specificity of 76 .7 %. The AUCs of R2 * were not significantly different between the 2 D-ROI and VOI methods.
CONCLUSION R2 * derived from multi-echo Dixon imaging whether by 2 D-ROI or VOI can aid in differentiation between benign and malignant FLLs.
Conflict-of-interest statement: The authors declare no conflict of interest.
Data sharing statement: No additional data are available.
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4 .0 )license, which permits others to distribute, remix, adapt, build upon this work non-commercially,and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: htt p://creativecommons.org/License s/by-nc/4 .0 /
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification Grade A (Excellent): 0 Grade B (Very good): B, B Grade C (Good): 0 Grade D (Fair): 0 Grade E (Poor): 0
Received: November 20 , 2020
Peer-review started: November 20 ,2020
First decision: January 23 , 2021
Revised: February 2 , 2021
Key Words: R2 *; Multi-echo Dixon imaging; Hypoxia; Malignant lesion; Benign lesion;Focal liver lesion
INTRODUCTION
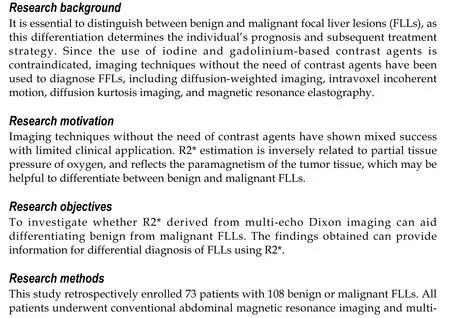
Liver cancer is the sixth most common cancer and the fourth leading cause of cancer deaths worldwide[1]. The liver is also the most frequent site for distant metastases[2].Clinically, once a focal liver lesion (FLL) is identified, it is essential to distinguish between benign and malignant lesions, as this differentiation determines the individual’s prognosis and subsequent treatment strategy[3]. Contrast-enhanced computed tomography (CT) and magnetic resonance imaging (MRI) are widely used to detect and characterize FLLs[4-7]. However, the use of iodine and gadolinium-based contrast agents is sometimes contraindicated; for example, in patients with severe kidney impairment due to the potential development of contrast-induced nephropathy[8] or nephrogenic systemic fibrosis[9]. Several imaging techniques without the need of contrast agents have been used to diagnose FFLs, including diffusionweighted image (DWI), intravoxel incoherent motion, diffusion kurtosis imaging, and magnetic resonance elastography, although these techniques have shown mixed success with limited clinical application[10 -13].
A hypoxic microenvironment is a hallmark in biology for solid tumors[14 ,15]. It is known that R2 * estimation (R2 * = 1 /T2 *) is inversely related to partial tissue pressure of oxygen, and reflects the paramagnetism of the tumor tissue, such as the presence of deoxygenated hemoglobin[15 -17 ]. Previous studies have demonstrated that R2 * can be used to assess oxygenation status in several malignancies[18 ,19]and offer additive value in identifying metastatic lymph nodes in breast cancer[20 ]. However, whether R2 * can be used to differentiate between benign and malignant FLLs remains to be determined. Besides, 2 D region of interest (2 D-ROI) and volume of interest (VOI)analyses, which are better for R2 * measurement in FFLs, remain elusive.
In this study, the diagnostic performances of R2 * derived from multi-echo Dixon imaging in differentiating between benign and malignant FLLs based on 2 D-ROI and VOI analyses were investigated. The purpose of this study was to determine whether R2 * derived from multi-echo Dixon imaging can aid in differentiating benign from malignant FLLs, and the impact of 2 D-ROI and VOI on the outcomes.
MATERIALS AND METHODS
Patients
This retrospective study was approved by the Institutional Ethics Review Board of our hospital (approval No. SYSEC-KY-KS-2020 -147 ), and the requirement for informed consent from the patients was waived. From January 2019 to December 2019 ,consecutive patients with FLLs were identified from the hospital database. Patients were included if they had: (1 ) A solid malignant or benign FLL confirmed by histology, and follow-up contrast-enhanced CT/MRI examination for at least 6 mo, or positron emission tomography (PET)-CT; and (2 ) Multi-echo Dixon imaging. The exclusion criteria were as follows: (1 ) Diffuse liver inflammation (n = 5 ); (2 ) Maximal lesion diameter < 10 mm (n = 5 ); (3 ) Lower signal-to-noise ratio on R2 * images; and (4 )Obvious breathing artifacts on R2 * images (n = 5 ).
MRI acquisition
MRI was performed on a 3 .0 T unit (MAGNETOM Skyra; Siemens Healthcare,Erlangen, Germany). The sequences consisted of conventional sequences and multiecho Dixon imaging. Conventional MRI included axial BLADE T2 -weighted imaging(T2 WI) [repetition-time/echo-time (TR/TE) = 9672 .9 -12331 .7 /84 ms; flip angle = 130 °;averages = 1 ; matrix = 320 × 320 ; field of view = 100 mm; slice thickness = 5 mm], axial and coronal T1 -weighted imaging (T1 WI) volume interpolated breath-hold examination (VIBE) (TR/TE = 3 .97 /1 .29 ms; flip angle = 9 °; averages = 1 ; matrix = 320 × 180 ; field of view = 75 mm; slice thickness = 3 mm), and axial DWI (TR/TE =4900 /66 ms; flip angle = 90 °; averages = 12 ; matrix = 192 × 113 ; field of view = 78 .125 mm; slice thickness = 5 mm; b values = 0 and 800 s/m2 ). The multi-echo Dixon imaging was performed with T2 * correction. The acquisition parameters were: TR = 9 ms; six-echo with TE = 1 .05 /2 .46 /3 .69 /4 .92 /6 .15 /7 .38 ms; averages = 1 ; matrix = 160 ×136 ; field of view = 450 mm; slice thickness = 3 .5 mm; number of slices = 64 ; a flip angle = 4 ° was used to minimize the effects of T1 weighting[21]. This sequence was acquired in a breath-hold of 16 s. After these sequences, multiphase contrast-enhanced imaging was performed after administration of gadolinium contrast medium(Magnevist; Bayer Schering Pharma, Berlin, Germany) using a fat-suppressed dynamic contrast enhancement sequence with the following acquisition parameters: TR/TE =3 .8 /1 .23 ms; averages = 1 ; slice thickness = 2 .5 ; field of view = 80 .56 ; matrix = 288 ×186 ; flip angle = 10 °. Then, all patients underwent axial and coronal contrast-enhanced T1 WI–VIBE (TR/TE = 3 .97 /1 .26 ms; flip angle = 9 °; averages = 1 ; slice thickness = 2 .3 mm; matrix = 320 × 180 ; field of view = 75 mm).
Image analysis
All the images were assessed by using the ImageJ software (http://rsb.info.nih.gov/ij/). A low flip angle multi-echo Dixon sequence was used to derive R2 * to minimize T1 -related bias and improve the separation of water and fat. The improvedtting of the signals within fatty tissues allows more accurate R2 * mapping and T2 *correction of the water-fat separation[22]. Two experienced radiologists (Shi GZ and Gao M, with 6 and 12 years of experience in liver diagnostic imaging, respectively)who were blinded to the diagnosis of patients manually delineated the lesions on R2 *maps. For 2 D-ROI, a single freehand ROI was drawn to cover the whole tumor area on the section showing the maximal tumor dimension. For VOI, the freehand ROI was placed slice by slice to cover the entire tumor volume. The mean R2 * values measured by 2 D-ROI and VOI were used for analysis (Figure 1 ).
Laboratory and anthropometric evaluations
Hepatitis B virus infection, α-fetoprotein (AFP), carbohydrate antigen 19 -9 (CA 19 -9 ),and carcinoma embryonic antigen (CEA) were measured using standard reagents.Liver cirrhosis was determined by Masson trichrome staining. The normal ranges are:AFP ≤ 25 ng/mL, CA 19 -9 ≤ 34 U/mL, and CEA ≤ 5 ng/mL. Laboratory examination was performed before clinical treatment. The time between laboratory examination and multi-echo MRI examination was within 1 wk.
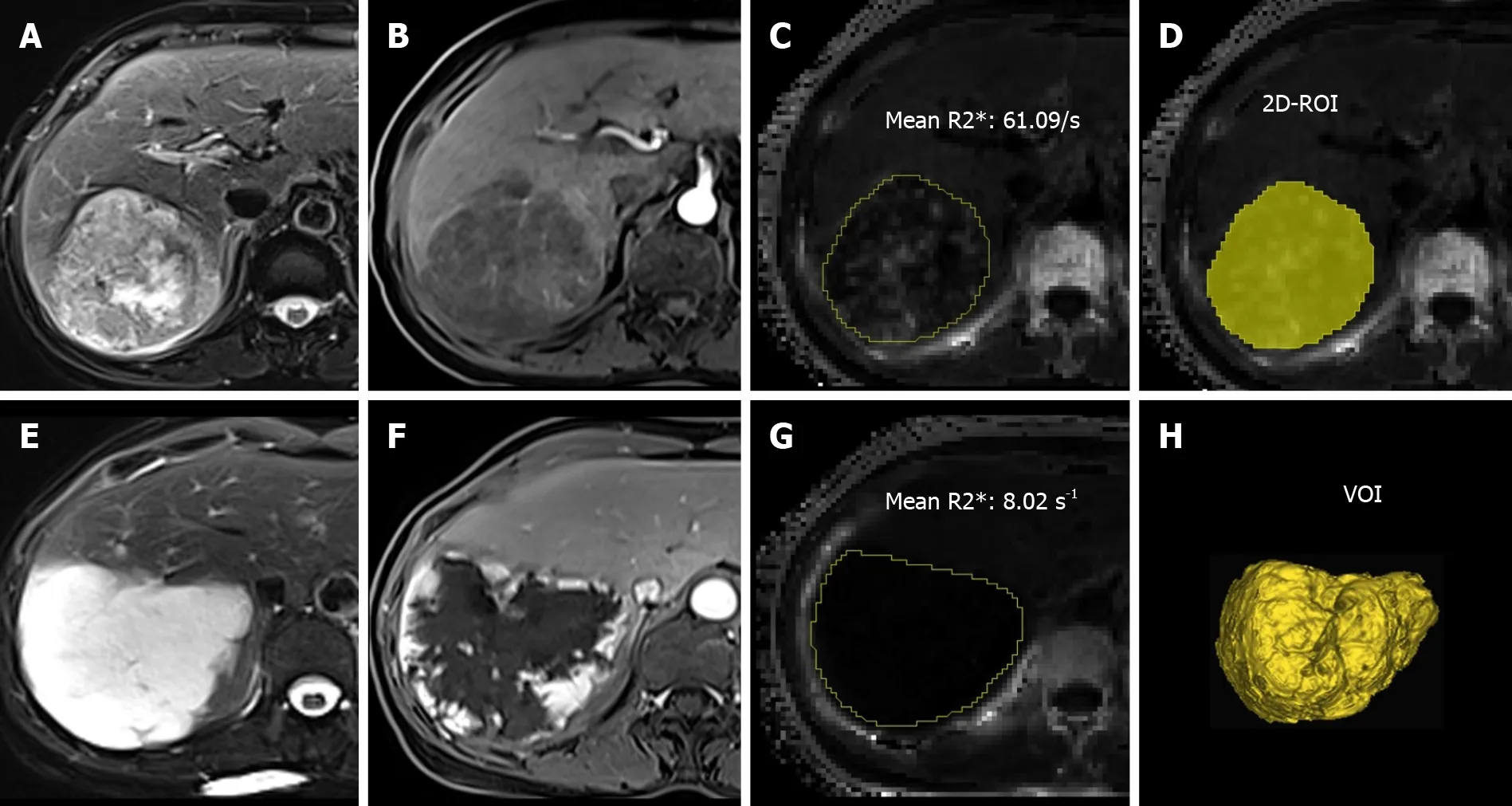
Figure 1 Two-dimensional region of interest and volume of interest. A-C: T2 -weighted imaging (T2 WI) (A), arterial phase contrast-enhanced T1 -weighted imaging (T1 WI) (B), and R2 * map showed liver metastasis (yellow line) (C) confirmed by histology in a 59 -year-old woman with lung cancer; D: Twodimensional region of interest was drawn on the section showing the maximal tumor dimension; E-G: T2 WI (E), arterial phase contrast-enhanced T1 WI (F), and R2 *map showed a live hemangioma (yellow line) (G) in a 59 -year-old woman; H: Volume of interest was placed covering the entire tumor volume on R2 * map. 2 D-ROI:Two-dimensional region of interest; VOI: Volume of interest.
Diagnosis of FLLs
All analyzed lesions were diagnosed by contrast-enhanced MRI, follow-up contrastenhanced CT/MRI examination within at least 6 mo, fluorine 18 (18 F) fluorodeoxyglucose (FDG) PET-CT, or histopathological findings (hepatectomy or biopsy)[5,22 -25]. Diagnostic reference standard was established based on histopathological confirmation in 29 /32 hepatocellular carcinomas (HCCs), 6 /9 intrahepatic cholangiocarcinomas (IHCCs), 7 /37 metastases, 5 /25 hemangiomas, and 2 /3 focal nodular hyperplasias (FNHs). In the remaining 69 FLLs without histopathological results, diagnoses were established by well-accepted imaging findings in all acquired MRI sequences (e.g., T1 WI, T2 WI, T2 -SPAIR, DWI, and contrast-enhanced T1 WI).Criteria were determined by consensus reading of two experienced radiologists (R1 ,Shi GZ; and R2 , Gao M) by consideration of all acquired images. Further reference standards were required: (1 ) FFLs were diagnosed as primary malignant FFLs if they showed (a) characteristic imaging appearance during a 6 -mo imaging follow-up combined with (b) clinical symptoms and serological results; (2 ) FFLs were diagnosed as liver metastasis in patients with primary malignancies (pathologically confirmed)when at least one of the following criteria was satisfied: (a) Newly developed lesion or an increase in size with typical imaging appearance during a 6 -mo imaging follow-up;and (b) abnormal18 F FDG uptake at PET-CT examination; and (3 ) FFLs were diagnosed as benign lesions if (a) they were stable at 6 -mo imaging follow-up with characteristic imaging appearance in subjects at low risk; and (b) no malignant tumor was found in patients with benign FLLs during imaging examination.
Three HCCs, three IHCCs, and 19 metastases were diagnosed according to 6 -mo imaging follow-up. Eleven metastases were confirmed by PET-CT. In liver metastasis patients, the primary tumors were bladder cancer (n = 9 ), lung cancer (n = 2 ),colorectal cancer (n = 7 ), cervical cancer (n = 4 ), gastric cancer (n = 3 ), gallbladder cancer (n = 1 ), breast cancer (n = 1 ), and HCC (n = 10 ). For benign FLLs, 20 hemangiomas and one FNH were confirmed by 6 -mo imaging follow-up. Two liver abscesses had typical imaging findings in all the MRI sequences and typical imaging findings in a 6 -mo follow-up MRI examination after clinical treatment.
Statistical analysis
Numerical data are expressed as the mean ± SD. The Bland–Altman plot was performed to determine the interobserver agreement on R2 * measurements. Intraclass correlation coefficient (ICC) was used to determine the reliability between the two radiologists in R2 * measurements using 2 D-ROI and VOI methods (0 -0 .20 poor; 0 .21 -0 .40 fair; 0 .41 -0 .60 moderate; 0 .61 -0 .80 good; and 0 .81 -1 .0 excellent correlation). Mean R2 * values from the two readers were used for the final analysis. Nonparametric Mann–Whitney test was used to compare the difference in R2 * values between the malignant and benign groups. The receiver operating characteristic (ROC) analysis was used to evaluate the diagnostic performances of R2 *. The area under the ROC curve (AUC), optimal cut-off values, sensitivity, and specificity were determined as the maximum Youden index. Differences in the diagnostic performance of the two different ROI positioning methods were analyzed by comparing ROC curves according to the method developed by DeLong et al[26 ]. P < 0 .05 (two-tail) indicated a statistically significant difference.
RESULTS
Clinicopathological characteristics
A total of 108 FLLs were found in 73 patients, including 78 malignant FLLs (mean maximum diameter, 48 .2 ± 37 .7 mm; range, 11 -163 mm) and 30 benign FLLs (mean maximum diameter, 32 .3 ± 22 .5 mm; range, 14 -94 mm). Forty-nine patients had malignant FFLs (30 men and 19 women; mean age, 56 .3 ± 10 .3 years; range, 40 -81 years), and 24 patients (11 men and 13 women; mean age, 52 .1 ± 12 .9 years; range, 31 -73 years) had benign FLLs. The malignant FFLs included 32 HCCs, nine IHCCs, and 37 liver metastases. Benign FFLs included 25 hemangiomas, three FNHs, and two liver abscesses. The mean maximum diameter of liver metastases, HCCs, and IHCCs was 29 .1 ± 24 .1 mm (range, 11 -122 mm), 66 .3 ± 43 .0 mm (range, 15 –163 mm), and 61 .9 ± 25 .9 mm (range, 32 -111 mm), respectively. In benign FFLs, the mean maximum diameter of hemangiomas, FNHs, and liver abscesses was 29 .4 ± 21 .8 mm (range, 14 -94 mm), 32 .0 ±8 .5 mm (range, 23 -40 mm), and 69 .5 ± 12 .0 mm (range, 61 -78 mm), respectively.Clinicopathological characteristics and laboratory evaluations of FFLs are shown in Tables 1 and 2 .
R2 * analysis
Figure 2 shows the Bland–Altman plot measurement of R2 * of FLLs for the two readers. For 2 D-ROI analysis, the 95 % limits of agreement of R2 * for the two readers were from -5 .68 to 5 .04 /s, and the mean difference for the two readers was -0 .32 /s. For VOI analysis, the 95 % limits of agreement of R2 * for the two readers were from -3 .65 to 3 .28 /s, and the mean difference for the two readers was -0 .18 /s. The differences between the two readers using two different methods were relatively small. ICC for the 2 D-ROI method was 0 .994 and ICC for the VOI method was 0 .998 . The interobserver agreement was excellent.
The mean R2 * values measured by 2 D-ROI and VOI methods were significantly higher in the malignant group than in the benign group (2 D-ROI: 37 .99 ± 17 .71 vs 18 .6 ± 8 .43 /s, P < 0 .001 ; VOI: 41 .11 ± 19 .01 vs 20 .61 ± 9 .01 /s, P < 0 .001 ). For 2 D-ROI measurement, the mean R2 * value of liver metastases was 44 .17 ± 21 .90 /s, and the mean R2 * values of HCCs and IHCCs were 33 .45 ± 10 .15 and 28 .72 ± 10 .21 /s,respectively. The mean R2 * values of hemangiomas, FNHs, and abscesses were 16 .66 ±8 .18 , 26 .21 ± 5 .61 , and 23 .29 ± 9 .31 /s, respectively. For VOI measurement, FFLs had a mean R2 * value of 48 .42 ± 23 .61 /s for liver metastases, 35 .41 ± 10 .04 /s for HCCs, 31 .34 ± 9 .65 /s for IHCCs, 19 .36 ± 8 .93 /s for hemangiomas, 27 .87 ± 7 .46 /s for FNHs, and 25 .29 ± 10 .46 /s for abscesses. Malignant FFLs had higher R2 * values than benign FLLs regardless of ROI placement methods (Table 3 ).
ROC analysis
The AUC of 2 D-ROI was 0 .884 (95 %CI, 0 .819 to 0 .950 ) at a cut-off of 25 .2 /s, with a sensitivity of 84 .6 % and specificity of 80 .0 % for differentiating benign from malignant FFLs. The VOI method yielded an AUC of 0 .875 (95 %CI: 0 .806 to 0 .945 ) at a cut-off of 26 .7 /s in distinguishing benign from malignant FFLs, with a sensitivity of 85 .9 % and specificity of 76 .7 %. There was no significant difference between the AUCs for 2 D-ROI and VOI positioning methods for discriminating benign from malignant FFLs (Z =1 .069 , P = 0 .285 ) (Figure 3 ).
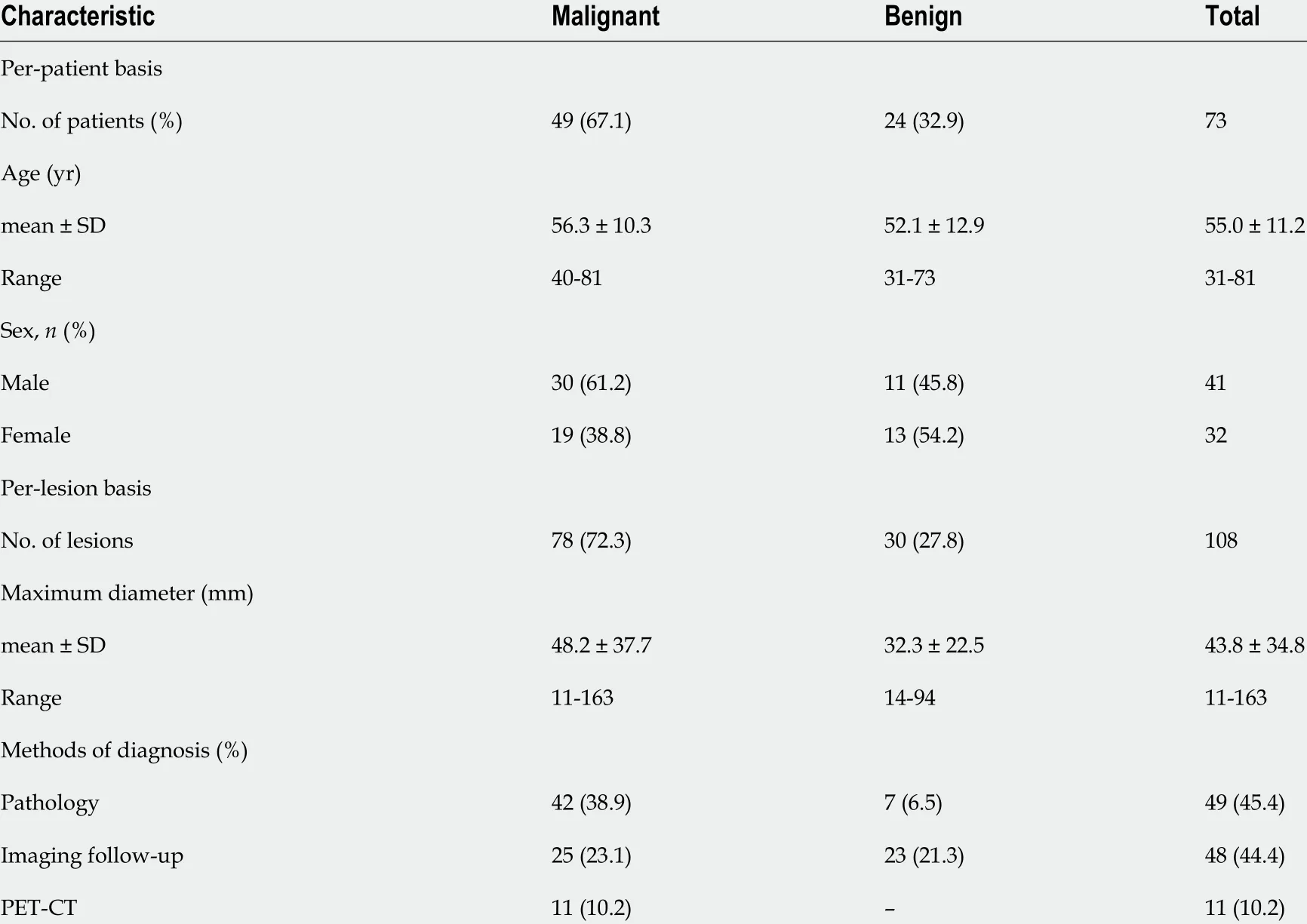
Table 1 Baseline characteristics of malignant and benign focal liver lesions of 73 patients
DISCUSSION
Our study showed that the mean R2 * value of malignant FLLs was significantly higher than that of the benign FLLs. R2 * derived from multi-echo Dixon imaging is a potential biomarker to differentiate malignant from benign FFLs.
The combined use of MRI, CT, and ultrasound has a high diagnostic performance for the identification of FLLs, but requires the administration of gadolinium or iodine contrast agents[7]. Gadolinium contrast is contraindicated in patients with severe renal impairment, because it may induce nephrogenic systemic fibrosis, and may even be a greater risk in patients with liver dysfunction[27 ,28]. Iodinated contrast administration for CT may aggravate renal failure[8]. Currently, no alternative imaging methods have been widely advocated for these patients. Hypoxia is an important factor in cancer progression, affecting the autonomous functions of tumor cells and nonautonomous processes such as angiogenesis, lymphangiogenesis, and inflammation[29]. Hypoxia causes an increase in the concentration of deoxygenated hemoglobin in the tumor.Deoxyhemoglobin can be used as an endogenous hypoxia tracer that may produce local magnetic field inhomogeneities to reduce T2 * relaxation time[30]. Furthermore,higher local deoxyhemoglobin may result in a decrease in proton T2 * relaxation time and a corresponding increase in R2 *, which indicates a link between R2 * and the oxygen concentration of local tissues[15]. Recently, susceptibility-weighted imaging,which was originally called blood-oxygen-level-dependent (BOLD) venographic imaging, has demonstrated advantages in the detection of hemorrhagic events due to its sensitivity to paramagnetic substances[31]. Also, BOLD MRI has shown ability in assessing tumor oxygenation and indirectly hypoxia, by detecting signal changes secondary to changes in blood flow and oxygenation[32]. These two sequences were commonly used in the central nervous system[33 ,34 ]. Currently, T2 * has been used in assessing tissue oxygenation status in vivo based on the paramagnetic properties of deoxyhemoglobin[35]. Besides, this technique has been shown to be feasible and accurate in the detection of HCC[27 ,32]
Previously, R2 * values have been used to distinguish cancerous from normal prostatic regions, with higher mean R2 * values being related to a higher tumor Gleason score[36 ]. In addition, higher R2 * values were found in high-grade bladder cancer[15 ] and clear cell renal cell carcinoma[37]than those of low-grade malignancies. Inour study, the mean R2 * value of malignant FLLs was significantly higher than that of the benign FLLs. This may be attributed to the rapid growth of liver malignancies,resulting in a relatively hypoxic state and an increase in deoxyhemoglobin[15].Consequently, the corresponding increase in R2 * value may correlate with the degree of malignancy of FFL. R2 * may be used as a quantitative imaging biomarker to provide additional information for tumor differential diagnosis.

Table 2 Clinicopathological characteristics of 108 focal liver lesions
In our study, mean R2 * values, whether derived from 2 D-ROI or VOI segmentation positioning methods, were highly reproducible. Moreover, the AUC of R2 * measured by 2 D-ROI was 0 .884 with a sensitivity of 84 .6 % and specificity of 80 .0 %, while AUC of R2 * measured by VOI yielded an AUC of 0 .875 with a sensitivity of 85 .9 % and specificity of 76 .7 %, in distinguishing benign from malignant FFLs, respectively.Campo et al[38]demonstrated that a large ROI that refers to as large an area of the liver as possible can improve the reproducibility and repeatability of R2 * measurements inpatients with low and high liver iron content. McCarville et al[39]reported excellent interobserver agreements in liver R2 * for both small (≥ 1 cm diameter) and whole liver ROI methods for iron overloaded patients who underwent biopsy. Sofue et al[40]found that R2 * measurements of whole liver volume and colocalized ROIs in three different hepatic segments were repeatable between examinations. However, these studies investigated ROI location of R2 * measurements in diffusive liver lesions rather than FLLs. To the best of our knowledge, our study was the first to investigate R2 *measurements in FFLs.

Table 3 Mean R2 * values for different focal liver lesions
We found similar results in differentiating between benign and malignant FLLs by using 2 D-ROI and VOI methods for R2 * measurement. ROC curve analysis demonstrated no significant difference between the AUCs for 2 D-ROI and VOI positioning methods for discriminating benign from malignant FFLs. R2 * measured by VOI analysis showed an AUC of 0 .875 , while 2 D-ROI analysis showed an AUC of 0 .884 in differentiating between benign and malignant FLLs. These results indicate that the impact of the different ROI positioning methods could be ignored for the differential diagnosis of benign and malignant FFLs. Thust et al[41]obtained the same results in volumetric and 2 D measurements of apparent diffusion coefficient in distinguishing glioma subtypes. Compared with VOI, 2 D-ROI is easier to delineate and easily incorporated into clinical practice. The easy implementation of R2 *measurements using 2 D-ROI will facilitate its clinical application.
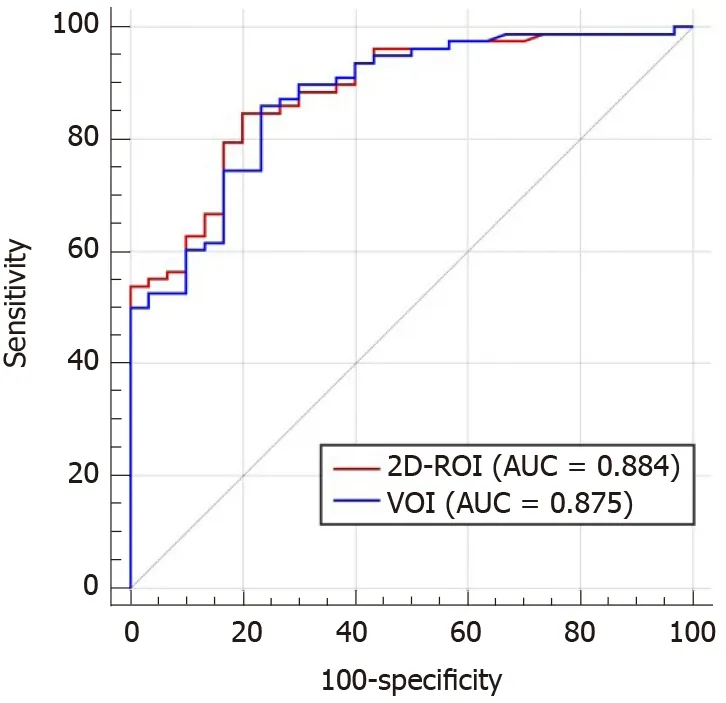
Figure 3 Receiver operating characteristic curve analysis of the two positioning methods in differentiating between malignant group and benign group. Two-dimensional region of interest and volume of interest methods yielded similar results. 2 D-ROI: Two-dimensional region of interest; VOI: Volume of interest; AUC: Area under the curve.
There were several limitations to this study. First, this was a single-center study,and the number of patients in the cohort was relatively small. A larger patient cohort in a multicenter setting is needed to validate our findings. Second, R2 * is an indirect method for monitoring tumor PO2[42 ]. In addition to the oxygenation state, R2 * can also be affected by other factors, such as hemoglobin levels, blood volume, and vasculature[15 ]. Nevertheless, various studies have found that T2 WI is a highly sensitive technique for reliably assessing paramagnetic deoxyhemoglobin, methemoglobin, or hemosiderin in lesions and tissues in body imaging[30 ,35 ,37 ]. R2 * quantification can yield hypoxia information about malignancies in a noninvasive manner[19 ,42]. In addition, the sequence used in our study is easy to perform and requires only a single breath-hold of 16 s to image the entire liver, and no image postprocessing is required.
CONCLUSION
In conclusion, R2 * values derived from multi-echo Dixon imaging can aid in discrimination between benign and malignant FLLs. 2 D-ROI and VOI methods do not affect the diagnostic performance of R2 *. R2 * measured by 2 D-ROI can be adopted to improve diagnostic accuracy of FFLs, particularly in patients with a contraindication to contrast agents.
ARTICLE HIGHLIGHTS

Research results
The study included 30 benign and 78 malignant FLLs. Mean R2 * was significantly higher for malignant than benign FFLs as measured by 2 D-ROI (P < 0 .001 ) and VOI (P< 0 .001 ). The area under the curve (AUC) of R2 * measured by 2 D-ROI was 0 .884 at a cut-off of 25 .2 /s, with a sensitivity of 84 .6 % and specificity of 80 .0 % for differentiating benign from malignant FFLs. R2 * measured by VOI yielded a AUC of 0 .875 at a cut-off of 26 .7 /s in distinguishing benign from malignant FFLs, with a sensitivity of 85 .9 %and specificity of 76 .7 %. The AUCs of R2 * were not significantly different between the 2 D-ROI and VOI methods. However, due to the relatively small sample size, a large population from multiple centers is needed for further validation of our findings.
Research conclusions
R2 * derived from multi-echo Dixon imaging can aid in differentiation between benign and malignant FLLs. 2 D-ROI and VOI methods do not affect the diagnostic performance of R2 *.
Research perspectives
This study describes that R2 * value derived from multi-echo Dixon imaging can aid in differentiation between benign and malignant FLLs. The multi-echo Dixon sequence is easy to perform and requires only a single breath-hold of 16 s to image the entire liver,which holds a good potential for clinical application.
杂志排行
World Journal of Gastroenterology的其它文章
- Cascade of care for children and adolescents with chronic hepatitis C
- Risk perception and knowledge of COVID-19 in patients with celiac disease
- Risk stratification and geographical mapping of Brazilian inflammatory bowel disease patients during the COVID-19 outbreak: Results from a nationwide survey
- Hepatitis E in solid organ transplant recipients: A systematic review and meta-analysis
- Primary localized gastric amyloidosis: A scoping review of the literature from clinical presentations to prognosis
- Emerging wearable technology applications in gastroenterology: A review of the literature
