Burkholderia pseudomallei infection manifests as mediastinal/hilar lymphadenopathy:A case report
2021-03-09QiLiQianFengXiaQiongFangSunXiangDongZhou
Qi Li, Qian-Feng Xia, Qiong-Fang Sun, Xiang-Dong Zhou✉
1Respiratory Medicine, the First Affiliated Hospital of Hainan Medical University, Haikou, China
2Key Laboratory of Emergency and Trauma of Ministry of Education, Hainan Medical University, Haikou, China
3Key Laboratory of Tropical Translational Medicine of Ministry of Education, School of Tropical Medicine and Laboratory Medicine, Hainan Medical University, Haikou, China
4Radiology Department, the First Affiliated Hospital of Hainan Medical University, Haikou, China
ABSTRACT
KEYWORDS: Endobronchial ultrasound-transbronchial needle aspiration; Lymphnode; Mediastinum; Melioidosis
1. Introduction
Melioidosis is a zoonotic disease that mainly occurs in Southeast Asia and northern Australia[1]. Hainan Province, a tropical island of China, has high incidence rates of Burkholderia (B.) pseudomallei infection. B. pseudomallei is widespread in the soil around Hainan Province, especially in coastal areas. Cases are reported every month, with the peak incidence occurring in August and September during monsoon season[2]. The population is generally susceptible,while fishermen and farmers have a higher incidence rate[3]. Most patients with melioidosis have underlying chronic diseases, such as diabetes, chronic liver disease, chronic lung disease or kidney dysfunction. Clinical symptoms of melioidosis include high fever,cough, hemoptysis and septic shock. Septicemia and pneumonia are two major clinical manifestations. The overall fatality rate of septicemia caused by melioidosis remains significantly high.Chronic pulmonary melioidosis can manifest as nodules, cavitation or fibrosis, and sometimes may present as enlarged lymph nodes.Hilar and/or mediastinal lymphadenopathy may be associated with sarcoidosis, carcinomatous lymphangitis, lymphoma,tuberculosis or other infectious diseases[4]; therefore, etiological diagnoses are difficult in some cases. Endobronchial ultrasound(EBUS)-transbronchial needle aspiration (TBNA) is a reliable first-line diagnostic investigation for isolated hilar or mediastinal lymphadenopathy[5].
2. Case presentation
This case report was approved by the Ethics Committee of Hainan Medical University (Hainan, China). The authors obtained consent from the patient.
A 49-year-old male patient presented with a 2-week history of sudden fever between 39.0 ℃ and 39.5 ℃, which was accompanied by chills, a cough with little sputum and shortness of breath that became worse at night and on exertion. The patient denied having chest pain, hemoptysis, nausea or vomiting. He was admitted to the local hospital and the treatment was unknown. The fever was alleviated after 8 days and he was discharged. Two days later, high fever recurred and a computerized tomography (CT) scan of his chest and abdomen showed multiple lymph node enlargement in the mediastinum and right hilar region. No abnormality was found in the abdomen. The patient had a gastric perforation repair surgery 8 years prior and did not have any history of diabetes, liver or kidney diseases. There was no clear history of exposure to tuberculosis.The patient was a farmer working on an Areca catechu plantation,residing in Wanning city, Hainan Province, China. He previously smoked 10 cigarettes/day for 10 years, and had given up one year prior to admission. There was no history of alcohol abuse.
On physical examination, his vital signs were normal (temperature,36.5 ℃; heart rate, 76/min; respiratory rate, 20/min; blood pressure, 97/62 mmHg). He showed no signs of supraclavicular or axillary lymphadenopathy. No crackles, rhonchi or pleural rubs were detected during the chest auscultation. Results of the cardiovascular and abdominal examinations were also normal. His electrocardiogram results showed normal sinus rhythm. Routine blood tests showed the following results: White blood cells,6.84×10/L; neutrophils, 3.98×10/L; red blood cells, 3.71×10/L; hemoglobin, 105 g/L and procalcitonin, 0.01 ng/mL. Liver function tests showed the following: Alanine transaminase, 63 U/L and alkaline phosphatase, 115 U/L. Renal function was normal. A CT scan of his chest and abdomen showed multiple enlarged lymph nodes in the mediastinum and right hilum (diameter, 18 mm×27 mm). The lymph nodes were partially fused, and unevenly enhanced by enhanced scanning (Figure 1A and 1B). No obvious in filtration,consolidation, cavity or nodules were found in the lungs and no abnormality was found in the abdomen.
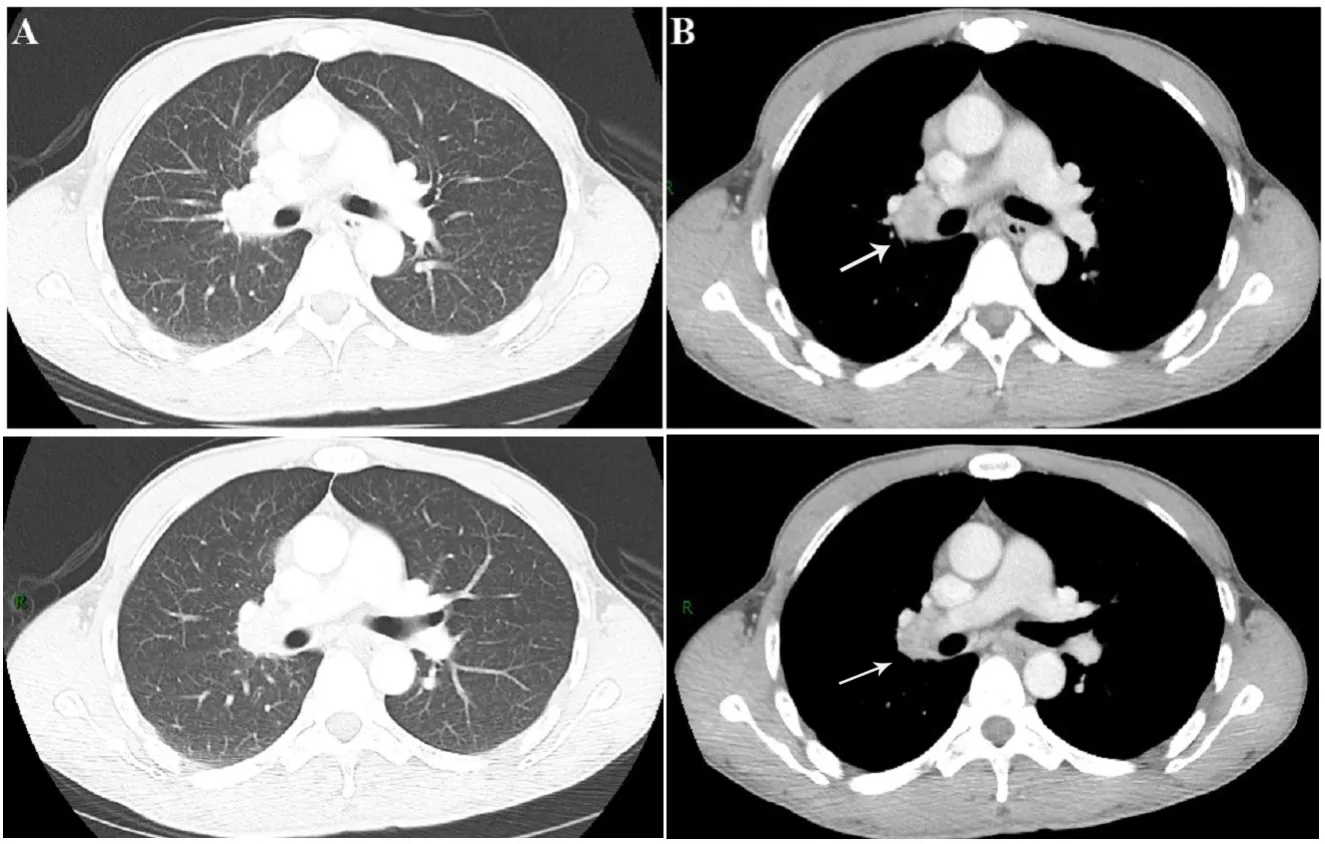
Figure 1. CT chest images at admission were taken for a 49-year-old male presenting with a 2-week history of sudden fever accompanied by chills, coughing and shortness of breath, which showed enlarged lymph nodes in the right hilum (arrow). (A) Lung window of the enhanced CT. (B) Mediastinal window of the enhanced CT. CT: computerized tomography.
As there was an initial suspicion of lymphoma or sarcoidosis,EBUS was performed. Ordinary bronchoscopy did not show any endobronchial lesions, but EBUS demonstrated enlargement of the right interlobar lymph nodes (R11). EBUS-guided TBNA was used to obtain tissues and aspirate for histology and bacterial culture. The aspirate culture on blood agar yielded growth of presumptive colonies of B. pseudomallei (Figure 2A and 2B), thus confirming the diagnosis of melioidosis. A drug sensitivity test showed that the organism was susceptible to ceftazidime, imipenem and trimethoprim/sulfamethoxazole. The patient was treated with intravenous ceftazidime and oral trimethoprim/sulfamethoxazole for 1 week, and once discharged he began a 12-week course of trimethoprim/sulfamethoxazole. At the 2-month follow-up, a pulmonary CT scan showed that the lesion in the mediastinum and right hilum had decreased in size (Figure 3A and 3B), and a further scan (6 months later) showed no signs of mediastinal lymphadenopathy (Figure 4A and 4B).
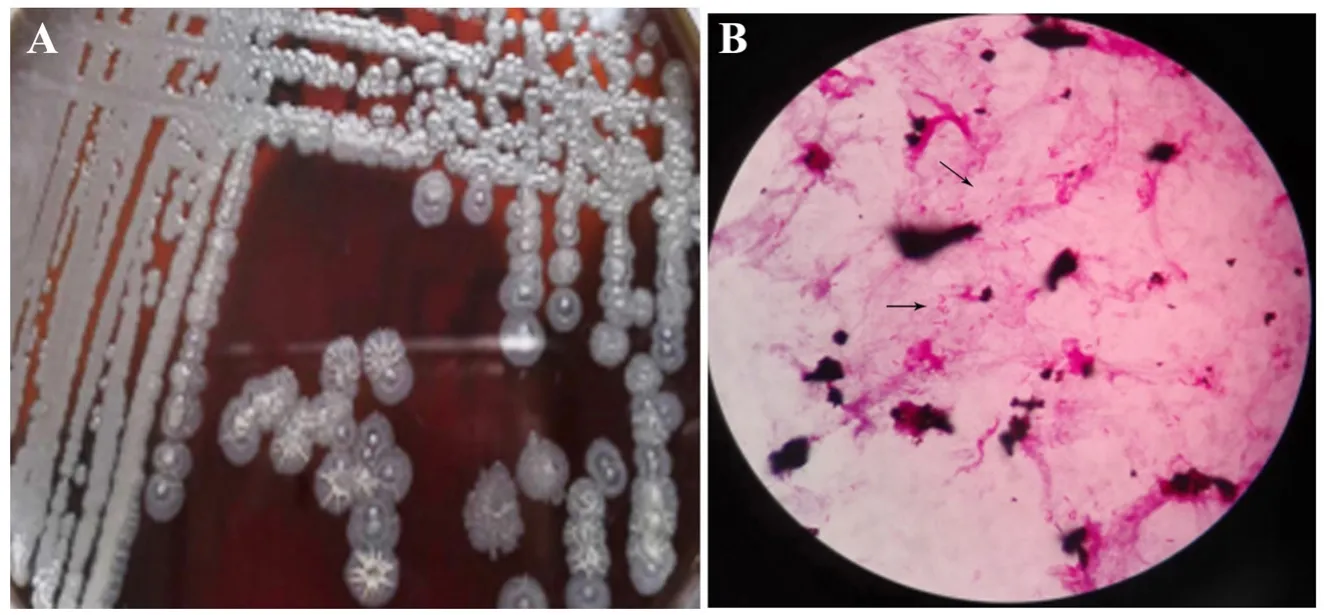
Figure 2. (A) Growth of Burkholderia pseudomallei on the blood agar plate. (B) Burkholderia pseudomallei was detected under the optical microscope (magnification,×200).
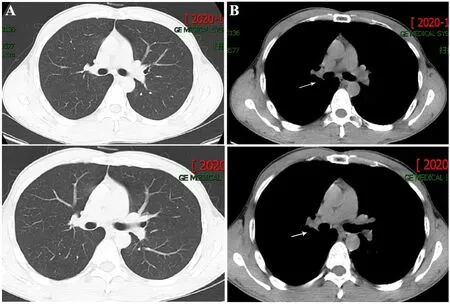
Figure 3. Chest CT scan images showed decreased enlargement of the lymph nodes in the right hilum 2 months after discharge. (A) Lung window of chest image. (B) Mediastinal window of chest image.Obviously decreased size of enlarged lymph nodes in the right hilum (arrow).
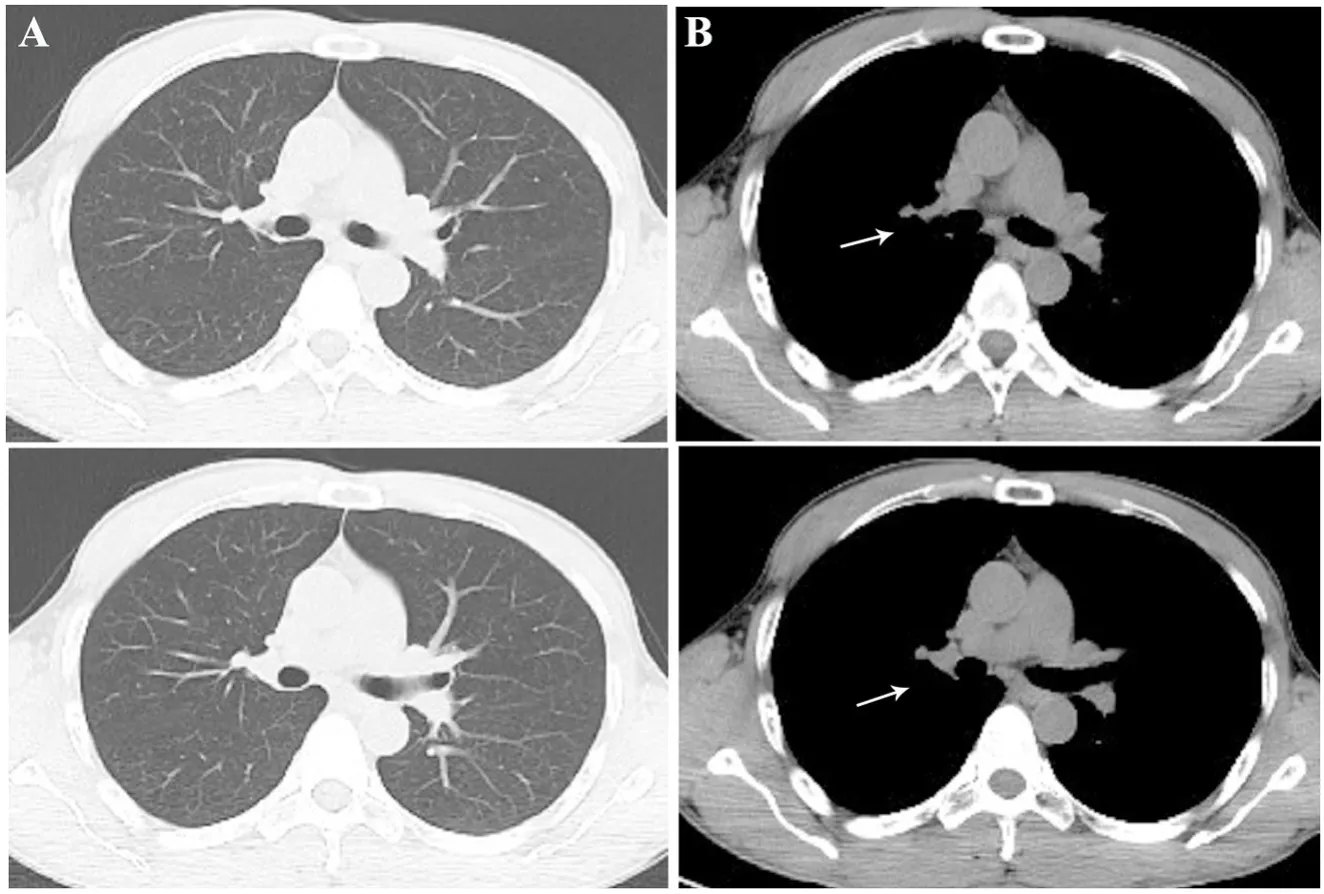
Figure 4. Chest CT scan images showed no enlargement of the lymph nodes in the right hilum 6 months after discharge. (A) Lung window of chest image. (B) Mediastinal window of chest image. No lymphadenopathy was found (arrow).
3. Discussion
B. pseudomallei is an environmental bacterium, which is unevenly distributed geographically and is particularly found in tropical Southeast Asia and Australia[6]. Hainan Province, a tropical island in China, has a high incidence of B. pseudomallei infection(melioidosis). We have found that B. pseudomallei is widespread in the soil around Hainan Province, especially in coastal areas[7]. The patient in the present case report lived in Wanning, a coastal city in eastern Hainan Province, and was a farmer working on an Areca plantation, where he was presumably exposed to the infection. He did not have underlying chronic diseases or was exposed to severe weather events, which may help to explain why he presented with localized lymphadenopathy in the hilum/mediastinum rather than severe acute manifestations, such as sepsis or pneumonia.
Most patients with melioidosis have underlying chronic diseases,such as diabetes mellitus, liver or kidney diseases, or malignancies.The lung is the most common place of localized infection,manifesting radiologically as pulmonary in filtrates, nodules, pleural effusion or cavitation. The clinical manifestations include high fever,cough (with or without sputum production), hemoptysis and even septic shock. In acute infections, culture of blood or pulmonary secretions are usually positive. Chronic pulmonary melioidosis can manifest as nodules, cavitation or fibrosis, which must be differentiated from tuberculosis and tumors; some may manifest as enlargement of hilar or mediastinal lymph nodes. Chan et al. reported a case in Singapore with a cavitary lung lesion and mediastinal lymphadenopathy that was initially suspected to be tuberculosis,but later confirmed as melioidosis via culture of the lymph node aspirate[8]. Solverson reported a 65-year-old male patient in Canada with mediastinal lymphadenopathy and fever after travelling to Mexico, and he was diagnosed with B. pseudomallei infection[9].Hainan is an endemic area of B. pseudomallei, and this is the first reported case with hilum and mediastinum lymphadenopathy in this area. Hilar or/and mediastinal lymphadenopathy may be associated with sarcoidosis, carcinomatous lymphangitis, tuberculosis and fungal infections. The mediastinal lymphadenopathy of this patient was initially suspected to be lymphoma by the radiologists, hence enhanced CT of the abdomen was performed to exclude any lesions or enlarged lymph nodes in the abdomen, however it turned out to be normal. When the patient was first admitted, our differential diagnoses included malignancy, tuberculosis, fungal infection and other infectious diseases, particularly given the history of fever. In this case, EBUS-TBNA proved to be a successful and minimally invasive diagnostic technique. The identification of this organism was carried by blood agar culture using the VITEK 2 compact system. Diagnosis is not easy because currently available biochemical identification systems may misidentify some strains of B. pseudomallei[10]. In this case, we made a presumptive diagnosis based on clinical history and basic microbiology test results, and the prognosis is favorable, but genotypic identification by sequencing of gene targets such as 16S ribosomal RNA or GroEL is still recommended to confirm the identified B. pseudomallei strains.
This case should act as a reminder that hilar/mediastinal lymphadenopathy can be caused by any infectious disease, not just tuberculosis or fungal infection, and melioidosis should be considered, especially in endemic areas. EBUS-TBNA is useful to diagnose patients with hilar/mediastinal lymphadenopathy, but histological examination and bacterial culture are also necessary.
Conflict of interest statement
The authors declare that there is no conflict of interest.
Funding
This work was supported by the National Natural Science Foundation of China (grant No.: 31660329, 81660010 and 81860001).
Authors’ contributions
Q.L. performed clinical collection, data analysis and drafted the article. Q.F.S. was responsible for the image taking. Q.F.X.and X.D.Z. contributed to the final version of the manuscript. We particularly thank Professor David A. B. Dance for proof reading the manuscript.
杂志排行
Asian Pacific Journal of Tropical Medicine的其它文章
- Prevalence of cryptosporidiosis in animals in Iran: A systematic review and metaanalysis
- Prevalence and intensity of soil-transmitted helminth infections among school-age children in the Cagayan Valley, the Philippines
- How knowledge of hepatitis B disease and vaccine influences vaccination practices among parents in Ho Chi Minh City, Vietnam
- In vitro anti-plasmodial activity of new synthetic derivatives of 1-(heteroaryl)-2-((5-nitroheteroaryl)methylene) hydrazine
- SARS-CoV-2 may impair pancreatic function via basigin: A single-cell transcriptomic study of the pancreas
