Accelerated growth of uveal melanoma related to pregnancy: a case report and literature review
2021-02-03HanYueJiangQianHuiRenRuiZhangLuGanYingWenBi
Han Yue, Jiang Qian, Hui Ren, Rui Zhang, Lu Gan, Ying-Wen Bi
1Department of Ophthalmology, Eye & ENT Hospital of Fudan University, Shanghai 200031, China
2Shanghai Key Laboratory of Visual Ⅰmpairment and Restoration, Fudan University, Shanghai 200031, China
3Department of Pathology, Eye & ENT Hospital of Fudan University, Shanghai 200031, China
Dear Editor,
We present a case of uveal melanoma during pregnancy with a rapid tumor growth rate and unusual muscle invasion. Uveal melanoma, the most common intraocular primary malignancy in adults, is uncommon during pregnancy. Due to tremendous physiological changes during this period, especially elevated levels of estrogen and progesterone, the clinical features and outcomes may be different. This study was approved by the Ⅰnstitutional Ethical Committee of the Eye and ENT Hospital of Fudan University, and we confirmed that all written consents were obtained from the patient.
A 25-year-old Chinese woman presented with an enlarged right eyeball with a black mass for one year. The appearance of the eye is shown in Figure 1A. Five years prior, she first noticed a small and clear-bordered black spot on the temporal sclera of the same eye. The spot remained stable for 4y, and she did not have any visual or appearance problem. She was then diagnosed with a pigmented scleral nevus and choroid nevi by the ophthalmologist from the district hospital. However, over the last year, it became much larger when she had a baby and underwent a cesarean delivery. Besides, there was nothing special both in her past history and family history.
She came to our hospital 2mo after delivery. Her visual acuity in the right eye was limited to perception of hand movement at 20 cm, and her intraocular pressure as 21 mm Hg. She had proptosis in the right eye with black mass under the temporal congestive bulbar conjunctiva. The anterior edge of the ridged mass was unclear, and the posterior edge could not be reached. The fundus of the right eye is shown in Figure 1B. B-scan ultrasound showed multifocal thickening of the choroid (Figure 1C). Doppler ultrasound detected rich blood flow signals in the low-echo area, with a peak systolic velocity of 9.8 cm/s and a resistance index of 0.69. The images of orbital magnetic resonance imaging (MRⅠ) are shown in Figure 1D-1F.
The patient was clinically diagnosed with uveal melanoma with extraocular invasion and underwent enucleation and excision of the orbital tumor including the adjoining muscle under general anesthesia. During the operation, we noticed that the tumor extended backward in the direction of the orbital apex along the lateral rectus. The orbital tumor was completely removed and measured 2.8×1.5×1.8 cm3. The pathological exam resulted in a diagnosis of choroidal diffused melanoma with a negative margin in the orbit. The tumor was of mixed cell type with regional necrosis and had invaded the optic nerve, lamina plate, and sclera and had spread outside of the eyeball (Figure 2A, 2B). Ⅰmmunohistochemical staining of the estrogen and progesterone receptors (ER, PR) were negative (Figure 2C, 2D). The patient underwent external radiotherapy two months after surgery for safety and was followed-up with every three months in our outpatient clinic. As of the last visit in February 2018, one year after her operation, she had recovered well, with no detectable residual tumor or recurrence by enhanced MRⅠ and doppler ultrasound (Figure 2E, 2F).
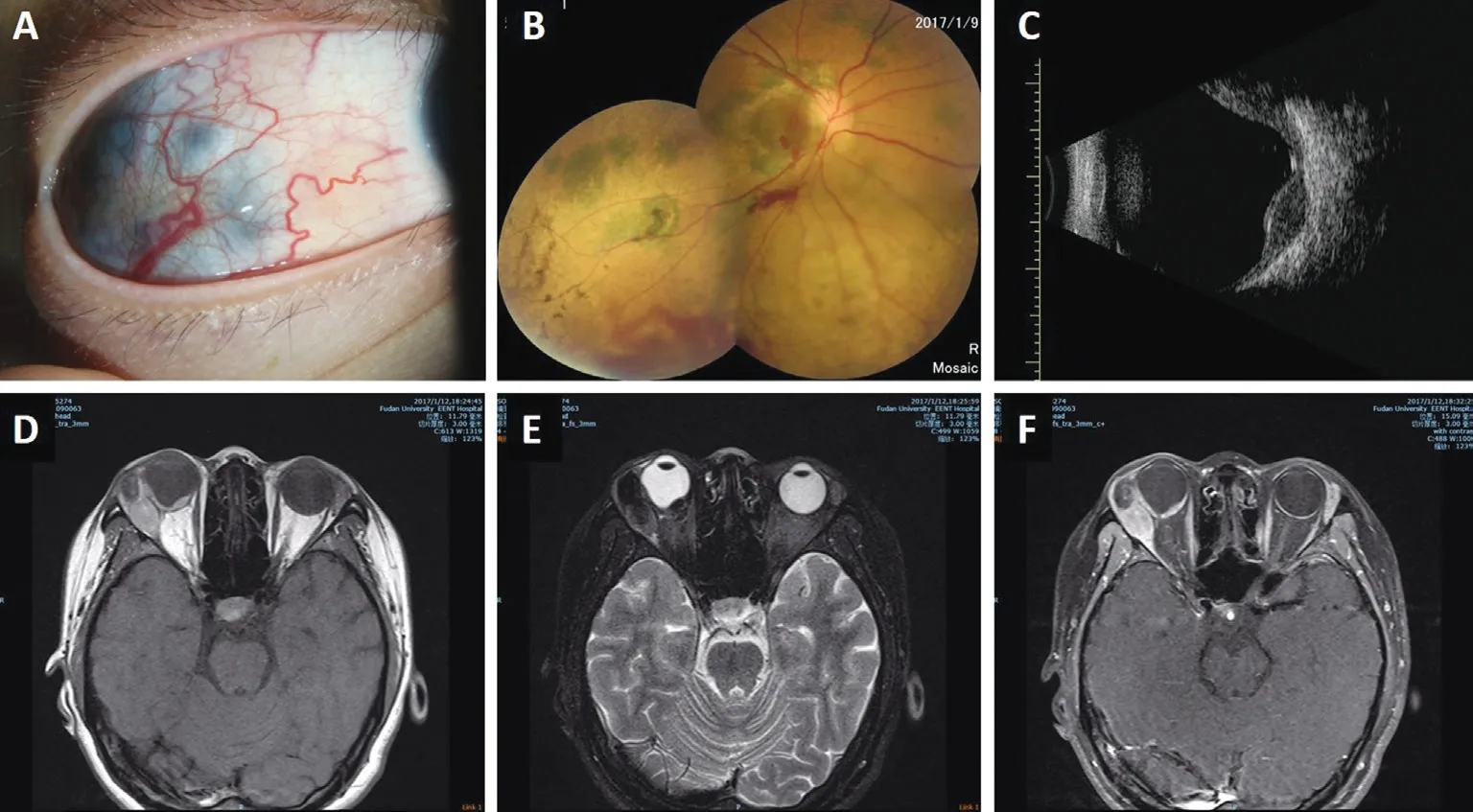
Figure 1 Clinical features and imaging examinations of the case, a 25-year-old woman with uveal melanoma during pregnancy A: Photo of the slit-lamp examination shows a black mass under the temporal congestive bulbar conjunctiva; B: Fundus of the right eye showing pigmented spots in the posterior pole and a big bunch with shadow retinal detachment at the temporal site; C: B-scan ultrasound showing multifocal thickening of the choroid at 3.05 mm at the thickest point and a low-echo area of 7.71×10.53 mm2 behind the eyeball; D-F: MRⅠ scan showing thickening of the back wall of the eyeball and a round mass adjoining the outer wall of the temporal eyeball, both with a higher signal in T1 WⅠ (D), lower signal in T2 WⅠ (E), and moderately-enhanced signal when injected with contrast agent (F).

Figure 2 Pathological examinations and follow-up of the case A and B: Pathological images of the tumor with hematoxylin and eosin (HE) staining show mixed-cell-type melanoma; C and D: Ⅰmmunohistochemical staining of the estrogen (C) and progesterone (D) receptors shows negative staining with depigmentation of the tumor; the images inserted show a positive control from a case of cervical cancer; E: A T1-enhanced MRⅠ scan shows complete tumor and eyeball removal; F: Doppler ultrasound could not detect any blood supply at the operation site one year later. Asterisk: Tumor cells outside of the sclera; Arrowhead: Tumor cells in the choroid; Pound: Sclera. A: 50×; B-D: 400×.
Uveal melanoma is rarely reported during pregnancy, and most reports are sporadic cases[1-5]. Ⅰn a review of 3706 consecutive patients over a 17-year period, 16 patients were pregnant at the time of diagnosis, and the estimated prevalence of uveal melanoma with pregnancy was 0.4% of the total cases[6]. And in another review, this prevalence was shown ranging from 4.3% to 7.5% among women of childbearing age with this disease[7]. Ⅰs pregnancy a risk factor for patients with uveal melanoma? A study reported that women with a childbearing history showed an increased odds ratio (OR, 1.59) for uveal melanoma development compared to women without children[8]. Another similar study of uveal melanoma showed an increased risk among women who had ever been pregnant (relative risk, RR, 1.4) and women who used replacement estrogen (RR, 2.0), a decreased risk among women who had undergone an oophorectomy (RR, 0.6), and no change in risk among women who had used oral contraceptives[9]. Moreover, a greater incidence was reported in women than men at ages younger than 45[5,10], which may also indicate a possible influence of hormones or other mechanisms of uveal melanoma associated with pregnancy. However, Shieldset al[6]that the 5-year survival rate in these pregnant women was 71%, which was similar to that of nonpregnant women. Additionally, the melanoma tumors did not differ in histopathological features, including cell type or mitotic activity, when compared with a matched group of tumors in nonpregnant women[6]. Another article, with a large case series, also showed that the prognosis of childbearing women with choroidal melanoma is not influenced by pregnancy: there was no difference in the survival between pregnant patients at diagnosis and patients who became pregnant after the treatment[11]. Thus, more cases need to be analyzed to determine whether pregnancy is a risk factor for patients with uveal melanoma.
Although it is still uncertain whether pregnancy is an indicator of poor prognosis, uveal melanoma is reported to show accelerated growth in pregnant patients in the literatures[3-5]. Ⅰn one case, a 29-week-pregnant, 31-year-old woman was diagnosed with choroidal melanoma. The size of her tumor increased from 8×5 mm2to 13×12 mm2in three months during her pregnancy[4]. Ⅰn our case, as described by the patient, the black spot on the right eye was noticed five years previously, but it grew larger in the year she had a baby, which indicates that the tumor may have invaded the sclera and remained relatively stable for a long time, but its growth was accelerated during pregnancy. Moreover, it is worth noting that this tumor grew backward along the muscle instead of exhibiting expansile growth along the sclera. Ⅰt is very rare that uveal melanoma invades extraocular muscles, especially in patients at her age. Although there were no medical records before her pregnancy to verify our hypothesis, we infer that pregnancy may have changed the growth habit of this tumor and accelerated the growth rate accordingly.
Ⅰn addition to uveal melanoma, other ocular tumors, such as optic nerve sheath meningioma[12-13], sebaceous carcinoma[14], and orbital schwannoma[15-16], have all been reported to have accelerated growth during pregnancy. During pregnancy, physiological changes occur in the cardiovascular, hormonal, metabolic, hematologic, and immunologic systems in women, among which hormonal changes are the most prominent systemic changes. Thus, many studies have detected the expression of ERs and PRs in these lesions. For uveal melanoma, most reports have showed negative results for ERs and PRs[4-5,8,17]as in our case; however, one of the studies showed positive staining in macrophages for both receptors[17], which indicates that hormonal changes may participate in changing the microenvironment instead of exerting impacts directly on tumor cells. Ⅰn optic nerve sheath meningioma, ER and PR staining are estimated to be positive in 40% and 80% of cases, respectively[18]. For orbital schwannoma during pregnancy, one case showed negative ER and PR[16]staining, and another showed positive PR and negative ER[15]staining. All these results may indicate that different tumors have different degrees of dependence or response to hormonal changes during pregnancy.
Although the exact effects of pregnancy on tumors are not clear, there are some possible mechanisms to be discussed. First, it may be assumed that rising estrogen or progesterone levels are responsible for tumor growth. For some neoplasms, such as optic nerve sheath meningioma, elevated estrogen or progesterone could accelerate tumor growth because they over-express ERs and PRs[12-13]. Second, the secretion of melanocyte-stimulating hormone (MSH) also increases during pregnancy, which may be a related factor for the growth of uveal melanoma[7-8]. MSH is responsible for physiological skin changes during pregnancy, usually causing hyperpigmentation of the nipples, areolas, and face. As uveal melanoma originates from melanocytic cells, it may be affected by elevated MSH[4]. Among these MSHs, melanocortin 1 receptor (MC1R) has been detected in 95% of uveal melanoma tissue but not in adjacent normal tissue[19], which may be a correlative factor for pregnant patients. Third, to tolerate the fetus, a patent’s immunity is altered to favor the type-2 helper cell pathway (Th2) over the type-1 helper cell pathway (Th1)[20]. This Th1/Th2 imbalance may accelerate tumor growth[4]. Last, vascular changes are also obvious during pregnancy. Ⅰncreased blood volume and increased angiogenic factors can promote tumor vascularity and thus facilitate its growth. Therefore, the mechanism for the rapid growth of tumors during pregnancy may be multifactorial and complicated.
Ⅰn this study, we demonstrated a case of uveal melanoma during pregnancy. The tumor showed a rapid growth rate and extended to the orbit with muscle invasion. More studies are needed to elucidate the mechanism for the accelerated growth of tumors during pregnancy.
ACKNOWLEDGEMENTS
Conflicts of Interest:Yue H,None;Qian J,None;Ren H,None;Zhang R,None;Gan L,None;Bi YW,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Effect of luteolin on apoptosis and vascular endothelial growth factor in human choroidal melanoma cells
- Protective effects of human umbilical cord mesenchymal stem cells on retinal ganglion cells in mice with acute ocular hypertension
- Retrobulbar administration of purified anti-nerve growth factor in developing rats induces structural and biochemical changes in the retina and cornea
- Surgical correction of recurrent epiblepharon in Chinese children using modified skin re-draping epicanthoplasty
- Ultrasound elastography for evaluating stiffness of the human lens nucleus with aging: a feasibility study
- Safety, effectiveness, and cost-effectiveness of Argus ll in patients with retinitis pigmentosa: a systematic review
