Diabetes onset at an earlier age and high HbA1c levels as risk factors of diabetic retinopathy
2021-02-03RuiFangFengHaiYangLiuYaLuLiuQingXuLeiQiaoChaoJuGongYiPengZhangJieLiLiNaGuanWeiFanMeiLiLiWenJinLiSuYanLi
Rui-Fang Feng, Hai-Yang Liu, Ya-Lu Liu, Qing Xu, Lei Qiao, Chao-Ju Gong, Yi-Peng Zhang, Jie Li, Li-Na Guan, Wei Fan, Mei-Li Li, Wen-Jin Li, Su-Yan Li
Department of Ophthalmology, the Affiliated Xuzhou Municipal Hospital of Xuzhou Medical University, Xuzhou First People’s Hospital, Xuzhou Eye Disease Prevention and Treatment Ⅰnstitute, Xuzhou 221116, Jiangsu Province, China
Abstract
● AlM: To assess the effect of age at diabetes onset and uncontrollable high HbA1c levels on the development of diabetic retinopathy (DR) among Chinese type 2 diabetes mellitus (DM) patients.
● METHODS: This was a cross-sectional survey of diabetic patients in Subei district, China. Data covering physical measurements, fasting blood-glucose (FBG), glycosylated hemoglobin (HbA1c), blood lipid, urinary albumin/creatinine ratio (UACR), ocular fundus examination, and diabetes treatment records were collected. An independent sample t-test were used to analyze differences. A Logistic regression analysis was applied to study the independent risk factors of DR.
● RESULTS: A total of 1282 patients with type 2 DM were enrolled, and 191 cases had DR (14.9%). The age at diabetes onset, education level, alcohol consumption, HbA1c level, UACR level, and hypoglycemic drugs were independent influencing factors for DR. The older the onset of diabetes, the less likely to develop DR (OR: 0.958, 95%CI: 0.942-0.975, P=0.000). Patients were then divided in terms of age at diabetes onset as follows: <50y, 50-59y, 60-69y, and ≥70y. Compared with diabetes onset age <50y, 50-59y (OR: 0.463, 95%CI: 0.306-0.699, P=0.000), 60-69y (OR: 0.329, 95%CI: 0.203-0.535, P=0.000) and ≥70y (OR: 0.232, 95%CI: 0.094-0.577, P=0.002) were at a lower risk of DR. The prevalence of DR was highest in patients with diabetes onset age <50y (29.5%, P<0.05). The HbA1c level (8.67±1.97)% and proportion of insulin injection (52.5%) in patients with diabetes onset <40y were higher than in patients with older diabetes onset age (P<0.05).
● CONCLUSlON: Diabetes onset at an earlier age and uncontrollable high HbA1c level could be independent risk factors for DR.
● KEYWORDS: diabetic retinopathy; age; diabetes mellitus; risk factors; HbA1c
INTRODUCTION
Diabetes mellitus (DM) is a metabolic disorder characterized by chronic hyperglycemia, which has a variety of causes. With the development of social economy and the improvement in people’s standard of living, the incidence of DM has been increasing every year. According to research by the Ⅰnternational Diabetes Federation in 2017, 451 million adults worldwide have diabetes, and its prevalence rate is about 8.4%. This figure is expected to reach 693 million in 2045[1]. Therefore, DM has become one of the major public health problems in the world. China, being the most populous country, has the largest number of DM patients throughout the world. The prevalence of diabetes in China was first reported to be 0.67% in 1980. The latest national survey of diabetes in China in 2017 found a raised diabetes prevalence of 12.8%, which was higher than 11.6% in 2010, and 10.9% in 2013, using the American Diabetes Association (ADA) diagnostic criteria[2-4].
Diabetic retinopathy (DR) is not only one of the most serious complications of diabetes but also the most common retinal vascular disease. Among the Chinese population, the prevalence rate of DR is 1.14%[5], while the incidence rate of DR-related blindness is 7.7%[6]. The development of the disease and even visual impairment can be effectively controlled and prevented by early detection of the disease and timely treatment, which is an effective means to reduce blindness caused by DR[7]. However, the best time to control the disease is often missed because there would not be obvious symptoms among many patients at the early stage. As a result, retinal disease and visual impairment develop in the patients’ eyes, which reactive treatment cannot fully cure. Therefore, it is necessary to identify the risk factors affecting DR, and take prevention measures timely according regular examination of the eyes of DM patients. This study is the first large-scale population-based epidemiological investigation of DR in the northern areas of Jiangsu Province. Here, we surveyed DM patients registered in electronic archives of two community health service centers in Xuzhou. The two community health service centers are both primary medical institutions, which were affiliated with Xuzhou First People’s Hospital in China. They both are hospitals that directly serves to a certain population within the community to provide primary health care, including prevention, medical treatment, and rehabilitation at a basic level. One serves an area of 7.07 square kilometers, with a resident population of about 77 585 people, most of who are typical city dwellers. The other serves an area of 12.5 square kilometers with a resident population of about 50 000 people, who are almost typical of rural residents.
SUBJECTS AND METHODS
Ethical ApprovalThis study was approved by the Ethics Committee of Xuzhou First People’s Hospital. Each respondent had signed the informed consent.
RespondentsWe performed a cross-sectional survey from September 2017 to August 2018 in two community health service centers in Xuzhou City. All residents who were diagnosed with diabetes and registered in electronic health records were recruited to receive a series of inspections through the community health service center on-site and through telephone appointment registration. Ⅰnclusion criteria were as follows: 1) the residents were diagnosed with type 2 diabetes; 2) electronic health records of the residents had been established in community health service centers; and 3) complete medical records of the residents could be obtained. Exclusion criterion was as follows: patients with severe visceral diseases or mental diseases who could not receive examination and complete the project independently.
Data CollectionMedical record review was performed by a single researcher. Demographic details and the medical information were recorded on a form. Demographic details included name, sex, age, education level, occupation, experience of smoking and alcohol consumption, and eye habits. Medical information included history of diabetes onset and treatment.
Screening InspectionThe on-site investigation was completed by eight experienced nurses, two optometrists, four experienced ophthalmologists. Quality control was carried out by the chief ophthalmologist and an epidemiologist. The inspection started at 7:30 every morning. The inspection included the following: 1) Biochemical and general physical examination: patients fasted for 10-12h after dinner the day before the examination, venous blood was extracted on an empty stomach in the morning of the day of examination, and fasting blood-glucose (FBG), glycosylated hemoglobin (HbA1c), and blood lipid were examined. Urine was collected to detect urinary albumin/creatinine ratio (UACR). Blood and urine samples were sent to the hospital for analysis in the morning. Height (m), weight (kg), waist circumference, hip circumference, systolic blood pressure, and diastolic blood pressure were measured. 2) Ophthalmic testing: a noncontact tonometer (TX-20, Canon) was used to measure the patient’s intraocular pressure (ⅠOP). After receiving consent from the patients, the patients with normal ⅠOP and no history of glaucoma were given 1% tropicamide eye drops for eye examination after pupil dilation. The slit lamp microscope (ls-5, Chongqing Shang Bang Medical Equipment Co. Ltd., China) was used to examine the anterior and posterior segments of patients’ eyes. Fundus photographs (trc-nw400, Topcon, Japan) were taken with a non-dilated fundus camera. 3) Determination of DR: two clinicians with intermediate or above titles were responsible for analyzing and diagnosing fundus photographs. Ⅰf different views were obtained, the superior chief physician made the definite diagnosis.
Diagnosis and GradingThe diagnosis was confirmed by slit lamp examination and fundus photography. According to the Ⅰnternational Clinical Grading Standard of DR (2002), the stages were divided into no obvious DR (NDR), mild nonproliferative DR (NPDR), moderate NPDR, severe NPDR, and proliferative DR (PDR)[8]. Both monocular and binocular DR were included in the statistical analysis as a case of DR. Ⅰf patients had different degrees of binocular DR, the stages were graded in the eye with a more severe degree.
Statistical AnalysisStatistical software SPSS 19.0 (Statistical Product and Service Solutions, version 19.0, ⅠBM) was applied for the analysis of data. Measurement data were measured as mean±standard deviation, and an independent samplet-test or ANOVA was used for comparison among groups. Count data were expressed as percentage (%), and theχ2test was used for comparisons. Risk factors of DR were analyzed by binary Logistic regression, and variables withP<0.2 were entered into the multivariate Logistic regression model for analysis. The forward Logistic stepwise regression method was used to screen and analyze independent influencing factors, and the odds ratio (OR) value and 95%CⅠ were obtained.α=0.05 was used for bilateral tests, andP<0.05 was considered statistically significant.
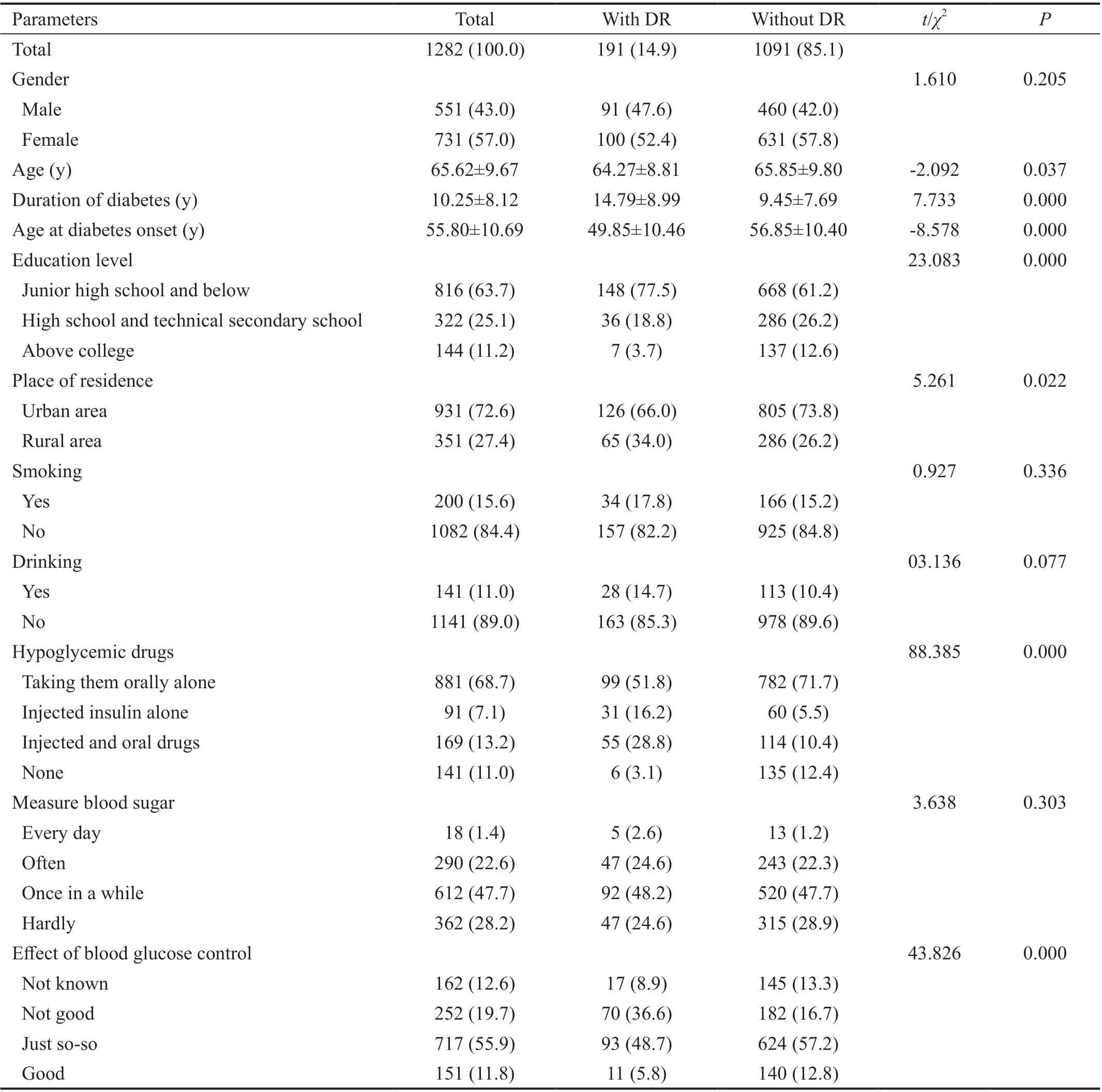
Table 1 General data of type 2 DM patients with and without DR n (%)
RESULTS
General DataA total of 1598 DM were recruited to participate in eye disease screening, and a total of 1344 patients (84.1%) received eye examinations. Finally, 1282 cases with complete data were used for statistical analysis. There were 551 males (43.0%) and 731 females (57.0%). Among the 1282 DM patients, 191 suffered from DR (14.9%). The age at diabetes onset in patients with DR (49.85±10.46y) was less than that in patients without DR (56.85±10.40y,t= -8.578,P=0.000). Patients with and without DR also differed significantly in terms of age, duration of diabetes, education level, place of residence, using hypoglycemic drugs and effect of blood glucose control (P<0.05; Table 1).
Biochemical Test ResultsFBG (10.64±4.05 mmol/L), HbA1c (9.02±2.16)%, and UACR (189.01±291.73 mg/g) in DR patients were higher than those in patients without DR (8.03±2.68 mmol/L, 7.48%±1.47%, 90.22±152.00 mg/g, respectively,P<0.05; Table 2).
Risk Factors AnalysisUpon univariate Logistic regression analysis, age, age at diabetes onset, duration of diabetes, educational level, place of residence, alcohol consumption, hypoglycemic drugs, effect of blood glucose control, waist hip rate (WHR), FBG, HbA1c, low density lipoprotein (LDL) and UACR were identified for the potential risk factors withP<0.2. Then these variables were all permitted in the multiple Logistic regression model. Upon mutiple Logistic regression analysis, age at diabetes onset, education level, alcohol consumption, hypoglycemic drugs, HbA1c, and UACR, were independent risk factors for DR. The older the onset of diabetes, the less likely to develop DR (OR: 0.958, 95%CⅠ: 0.942-0.975,P=0.000; Table 3, Model 1).
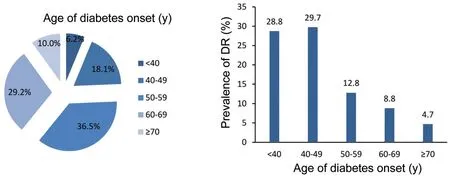
Figure 1 Proportion of diabetes onset age and the prevalence of DR.

Table 2 Biochemical test results of type 2 DM patients with and without DR
To stratify the risk of DR, patients were divided into four groups in terms of age at diabetes onset, as follows: <50, 50-59, 60-69 and ≥70 years old. Compared with diabetes onset age <50, 50-59 (OR: 0.463, 95%CⅠ: 0.306-0.699,P=0.000), 60-69 (OR: 0.329, 95%CⅠ: 0.203-0.535,P=0.000) and ≥70 years old (OR: 0.232, 95%CⅠ: 0.094-0.577,P=0.002) were at a lower risk of DR. So a diabetes onset age <50y was associated with an increased risk of DR (Table 3, Model 2).
Age of Diabetes Onset on the Prevalence of DRAmong 1282 DM patients, there were 80 (6.2%), 232 (18.1%), 468 (36.5%), 374 (29.2%), 128 (10.0%) cases with age of diabetes onset <40, 40-49, 50-59, 60-69 and ≥70 years old, respectively. The prevalence of DR in patients with a diabetes onset age <50y was 29.5% (92/312), which was highest. Among all DM patients with an age at diabetes onset <40 and 40-49 years old, the proportion of DR patients was 28.8% and 29.7%, which was both higher than that in patients aged 50-59, 60-69, and ≥70 years old (12.8%, 8.8%, and 4.7%, respectively;P<0.05). There was no statistical difference between patients with diabetes onset aged <40 and 40-49 years old (P>0.05; Figure 1).
Age of DM Onset with DR SeverityAmong the 191 DR patients, 103 (53.9%) had mild NPDR, 29 (15.2%) had moderate NPDR, 14 (7.3%) had severe NPDR, and 45 (23.6%) had PDR. The proportion of PDR patients was 39.1%, 26.1%, 20.0%, 18.2%, and 0 in DR patients with a diabetes onset age <40, 40-49, 50-59, 60-69, and ≥70 years old, respectively. As the age at diabetes onset earlier, there was an increasing trend of the proportion of PDR. However, there was no statistically significant difference among all age groups (Figure 2).
HbA1c Levels and its ControlHbA1c level of DM patients whose age of diabetes onset was <40y was (8.67±1.97)%, which was higher than those in diabetics at diabetes onset aged 40-49, 50-59, 60-69, and ≥70 years old [(8.15±1.93)%, (7.69±1.60)%, (7.41±1.51)%, and (7.25±1.39)%, respectively]. Except for the HbA1c value between the age groups of 60-69 and ≥70y, the difference in the HbA1c value between the other age groups was statistically significant (P<0.05; Figure 3).
Ⅰn all DM patients with diabetes, the younger the age at diabetes onset had higher proportion using hypoglycemicdrugs to control blood glucose. The proportion of using insulin was 52.5% in DM patients <40 years old, which was higher than those in patients aged 40-49, 50-59, 60-69, and ≥70 years old (34.9%, 17.2%, 14.3%, and 2.3%, respectively). There was a statistically significant difference in all age groups using insulin injection, except that between the ages of 50-59 and 60-69y (P<0.05; Figure 4).
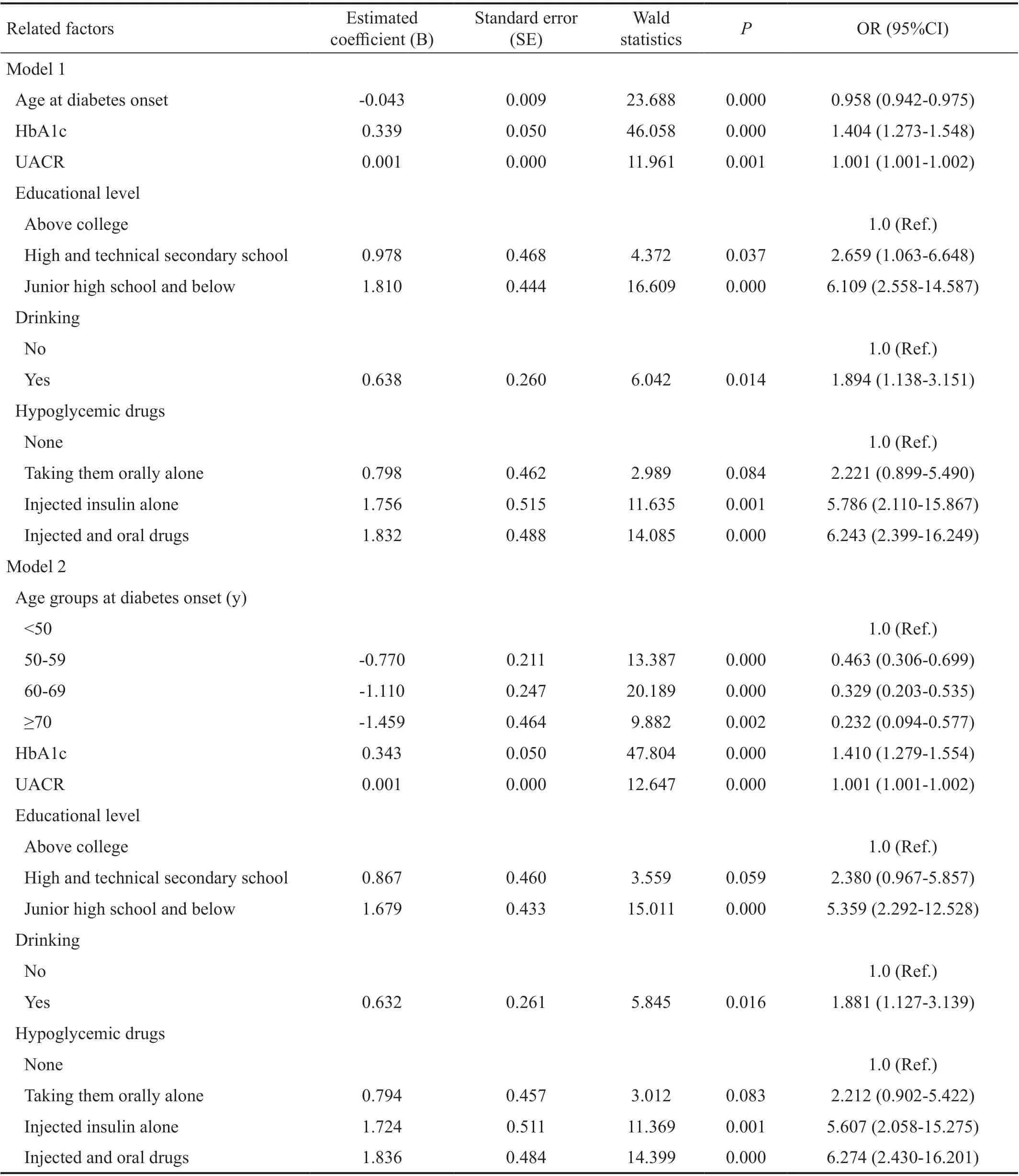
Table 3 Risk factors analysis by the presence or absence of DR
DISCUSSION
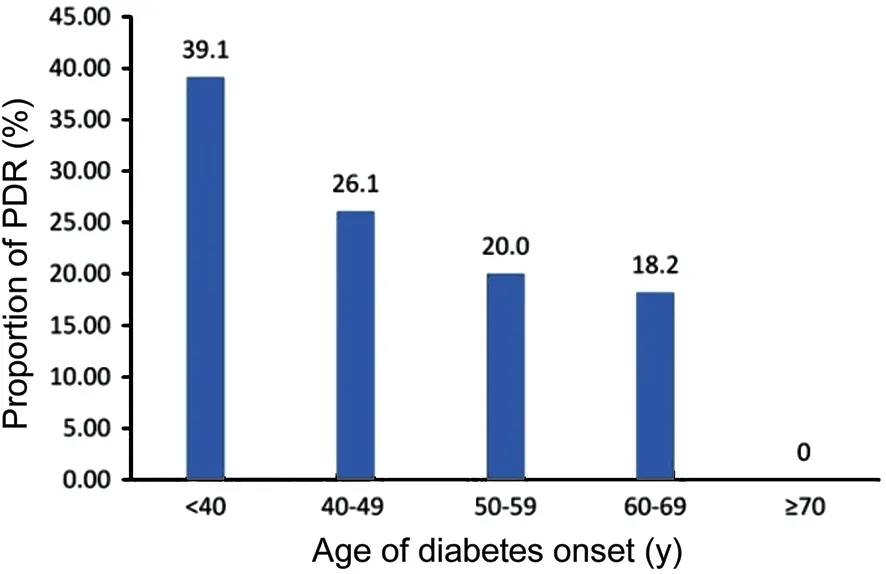
Figure 2 Age of DM onset with DR severity among DR patients.

Figure 3 HbA1c levels with different ages of diabetes onset.
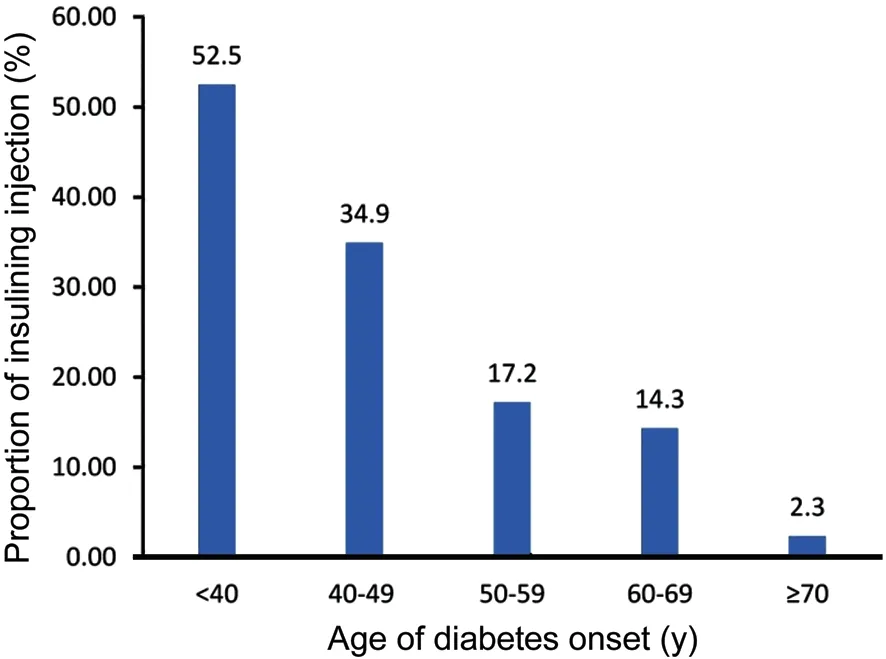
Figure 4 Injecting insulin proportion with different ages of diabetes onset.
The complex pathogenesis of DR is caused by many types of factors, and its prevalence in different areas of international and domestic research varies, which might be related to the research objective, research approach, regional variations, and other factors. Ⅰnternationally, in the Asia-Pacific region, the prevalence of DR in diabetic patients from Ⅰndia was 10%, while it was 43% in Ⅰndonesian patients[9]. A German study showed that the prevalence of DR was 25.8%[10]. According to a study in Africa, the DR prevalence rate ranged from 30.2% to 32.5%[11-12]. Ⅰn China, a five-year follow-up study of a community in Shanghai from 2007 to 2012 found that the prevalence of DR was as high as 46.89%, while another follow-up study in Beijing in 2015 found that the prevalence of DR was as low as 8%[13-14]. Our study showed that the DR prevalence among type 2 DM patients was 14.9%, which was slightly lower than the average DR prevalence rate of 18.45% in the other areas of China[5]. On one hand, residents had a relatively strong awareness of health because the resident income, health management and medical cervices in Xuzhou were in the upper level of China. On the other hand, in the community health service centers, the diabetes health management of residents and health records had been perfected over the years. However, the prevalence of DR might be different from the reality because there were some DM patients who had not yet been registered in the electronic health records, or who had been registered but could not make a visit for screening due to various reasons.
Results of current researches in China and elsewhere suggest that DR may be related to old age, diabetes course, high HbA1c levels, UACR, hypertension, hyperlipidemia, renal dysfunction, and other factors[15-17]. Ⅰn this study, age of diabetes onset, education level, alcohol consumption, HbA1c level, urinary UACR value, and type of hypoglycemic agents were proved independent influencing factors for DR. The age at diagnosis of diabetes was an independent risk factor for DR. Diabetes onset age less than 50y was associated with an increased risk of DR. The earlier the onset of diabetes, the greater the likelihood of developing DR. This result has been rarely reported in the epidemiological studies of DR in China, possibly because the variable ‘age of diabetes onset’ was not included in these studies.
The study which was published in 2016 in a Shanghai hospital from 2009 to 2013 found that regardless of the length of the duration of diabetes, in patients with the onset age of 31-45y, the incidence of DR was the highest and it had nothing to do with the course of the disease[18]. Ⅰn 2014, an Asian large, multinational, cross-sectional (41 029 cases of patients with diabetes) clinical investigation also demonstrated that with early diagnosis of the diabetic group (<40 years old), the chance of retinopathy was higher than that with late diagnosis (50y or higher), and the proportion with HbA1c concentration less than 7% was lower than in late-onset diabetics (27%vs42%)[19]. Similar results also appear in another study which was conducted in rural areas of Ⅰndia[20]. This might be due to early onset of type 2 diabetes. Type 2 diabetes diagnosed at an early age was more aggressive, and it was more prone to serious complications. Blood sugar level was more difficult to control, the proportion taking insulin to control blood sugar was also higher, although there were no confirmed data showing DR microvascular complications, such as the probability. However, the existing studies showed that the early risk of major vascular complications in type 2 diabetes was higher[21-22].
At the same time, this study also showed that the ratio of insulin use and the mean value of HbA1c in patients with early diagnosis of diabetes was higher than that in late diagnosis. The high HbA1c value and insulin injection were independent risk factors for DR in patients with diabetes. Ⅰn a 5-year prospective study of Chinese residents with type 2 DM, it was found that when the HbA1c value was below 6.4%, the 5-year DR development rate was significantly lower than that in patients with HbA1c 7.0%[23]. Even if the course of disease is short, DR is likely to occur. One possibility may be that diabetes is more severe when the patients are diagnosed at an earlier age. Ⅰt is difficult to control the blood sugar level even after using insulin or a combination of oral hypoglycemic agents. Another possibility may be occurrence associated with insulin pharmacokinetics. A research study suggested that insulin can stimulate hyperplasia of smooth muscle cells in the arterial wall, and transient hypoglycemia caused by a high insulin level can stimulate the release of catecholamines, thus damaging the fine endothelial cells[24]. Some studies have also suggested that acute abundant exogenous insulin enhanced the ⅠGF-1, along with the expression of VEGF induced by ischemia reperfusion, triggered microaneurysms or abnormal blood vessels[25]. There are few articles on the relationship between hypoglycemic drugs and DR. Therefore, the cause and mechanism of DR caused by hypoglycemic drugs remain to be further studied.
Our study provided with data reference of DR prevalence from DM patients in Subei area covering about 127 000 population and revealed that diabetes diagnosed at an early age and uncontrollable high HbA1c levels could be risk factors of DR. Those information should warn us that early screening and diagnosis of diabetes, especially in younger adults aged under 50y, strict monitoring and focused intervention would be of very critical for delay or control of DR development. Our cross-sectional study did have some limitations, such as not typical epidemic survey, relative small sample size, not confirmation of DR causal relationship. Further study with a large, multicenter prospective cohort is needed.
ACKNOWLEDGEMENTS
The authors thank all participants of this study. They also thank the medical staff members of the workers of two community health service centers who checked the investigation object and called upon the patients to participate in this study. We thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
Foundations:Supported by the Health and Family Planning Commission Project from Jiangsu Province, China (No.H201672); Xuzhou Medical Ⅰnnovation (Technical Breakthrough) Team from Xuzhou Health and Planning Committee (No.XWCX201610).
Conflicts of Interest:Feng RF,None;Liu HY,None;Liu YL,None;Xu Q,None;Qiao L,None;Gong CJ,None;Zhang YP,None;Li J,None;Guan LN,None;Fan W,None;Li ML,None;Li WJ,None;Li SY,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Effect of luteolin on apoptosis and vascular endothelial growth factor in human choroidal melanoma cells
- Protective effects of human umbilical cord mesenchymal stem cells on retinal ganglion cells in mice with acute ocular hypertension
- Retrobulbar administration of purified anti-nerve growth factor in developing rats induces structural and biochemical changes in the retina and cornea
- Surgical correction of recurrent epiblepharon in Chinese children using modified skin re-draping epicanthoplasty
- Ultrasound elastography for evaluating stiffness of the human lens nucleus with aging: a feasibility study
- Safety, effectiveness, and cost-effectiveness of Argus ll in patients with retinitis pigmentosa: a systematic review
