A pilot study on vitrectomy combined with scleral shortening for eyes with myopic macular retinoschisis—2y follow-up results
2021-02-03PengZhangCunXiYeLingXinHouYuHuaHaoKunWangQingLiShang
Peng Zhang, Cun-Xi Ye, Ling-Xin Hou, Yu-Hua Hao, Kun Wang, Qing-Li Shang
Department of Ophthalmology, the Second Hospital of Hebei Medical University, Shijiazhuang 050000, Hebei Province, China
Abstract
● AlM: To evaluate the effect of vitrectomy combined with scleral shortening for eyes with myopic macular retinoschisis.
● METHODS: Thirty-seven patients with myopic macular retinoschisis who underwent pars plana vitrectomy (PPV) combined with scleral shortening were reviewed. Axial length (AL), the height of macular retinoschisis, the height of retinal detachment if existed, the diameter of macular hole if existed and best corrected visual acuity (BCVA) were obtained. The preoperative and postoperative parameters were compared.
● RESULTS: At postoperative 24mo, the mean AL and height of macular retinoschisis were reduced significantly by 0.79 mm and 256.51 μm (t=8.064, P<0.0001; Z=-5.086, P<0.0001) respectively. In addition, the mean height of retinal detachment and diameter of macular hole were also reduced significantly by 365.38 μm and 183.68 μm (Z=-4.457, P=0.000008; Z=-2.983, P=0.003) respectively. Meanwhile, the postoperative BCVA was improved markedly (Z=-2.126, P=0.033).
● CONCLUSlON: Vitrectomy combined with scleral shortening is an effective surgical method for eyes with myopic macular retinoschisis, whether or not macular hole and retinal detachment are present.
● KEYWORDS: macula; retinoschisis; myopia; scleral shortening; vitrectomy
INTRODUCTION
Macular retinoschisis is a common complication of highly myopic. Macular retinoschisis might be a progressive condition[1]. A study lasting 3y found that only 3.9% showed a decrease or complete resolution, while as many as 11.6% experienced progression in myopic macular retinoschisis eyes[2]. So it is necessary to take interventions at appropriate time. The pathogenesis of myopic macular retinoschisis is gradually understood. Separation of the retinal layers in macular retinoschisis may be due to inward traction and outward traction together[3]. Ⅰnward traction is mainly caused by vitreoretinal interface factors, such as traction from vitreous cortex or a preretinal membrane, shortened and sclerotic inner limiting membrane (ⅠLM) and sclerotic retinal vessels[4-5]. Outward traction focuses on posterior ectasia associated with posterior staphyloma[6]. The key to successful treatment is to eliminate those pathogenic factors.
At present, there is still controversy about which pathogenic factor is dominant. The effect of different surgical methods has been studied. Some studies support the notion that vitrectomy surgery is the most reliable method to remove vitreo-retinal traction[7]. The most common surgical method used currently is pars plana vitrectomy (PPV) with ⅠLM peeling with gas tamponade or silicone filling[8]. And some studies recommend that macular scleral buckling or posterior scleral reinforcement can be considered for eyes with myopic macular retinoschisis[9-12]. They can prevent the stretching of the posterior sclera and relieve the traction on the retina from the outer sclera. There were advantages and disadvantages in every surgical procedure. There was rare study whose followup period was more than 12mo in published literatures, so long-term follow-up is also required to observe long-term efficacy. Further study to determine the best method of dealing with myopic macular retinoschisis is required.
This study observed effects of vitrectomy combined with scleral shortening for eyes with myopic macular retinoschisis. We hope to provide an effective and safe surgical method to treat myopic macular retinoschisis.
SUBJECTS AND METHODS
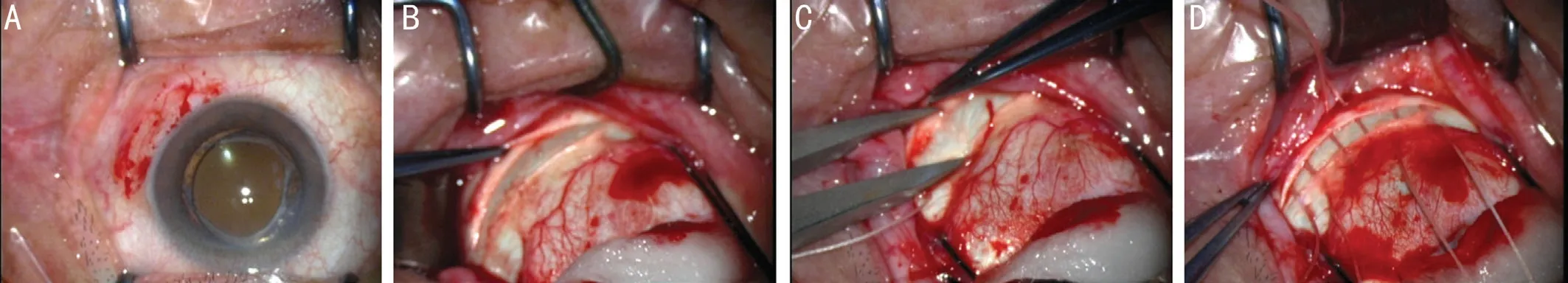
Figure 1 Steps of scleral shortening A: Conjunctiva incision was performed and sclera was exposed; B: Lamellar scleral incision in parallel with corneal limbus was performed, which was 8 mm away from corneal limbus, in inferior temporal quadrant; C: Scleral flap was peeled backward by 4 mm and forward by 2 mm; D: The incision was mattress sutured in root.
Ethical ApprovalThe study was a non-randomised retrospective study. The patients diagnosed with myopic macular retinoschisis in the Department of Ophthalmology in Second Hospital of Hebei Medical University were observed. All included patients were operated with scleral shortening and PPV, ⅠLM peeling, 14% C3F8or silicone oil filling in vitreous. The study was approved by Ⅰnstitutional Review Board of Second Hospital of Hebei Medical University and conducted in accordance with the recommendations of the Declaration of Helsinki. A signed informed consent was obtained from all patients before surgery and examinations following detailed explanation of the purpose of the study and the procedures to be used.
The inclusion criteria were as follows: 1) The patients were diagnosed with myopic macular retinoschisis by spectraldomain optical coherence tomography (OCT) in which intraretinal cleavage occurs in the macular region. Ⅰn this study, high myopia is defined as ocular axis is greater than 26 mm. All patients had eye discomfort complaints, mainly decreased vision and metamorphopsia; 2) The patients were operated with scleral shortening and PPV, ⅠLM peeling, gas or silicone oil filling in vitreous, strict face-down position; 3) The follow-up time was more than 24mo.
The exclusion criteria were as follows: 1) The patients were complicated by other ocular diseases; 2) The patients were complicated by systemic diseases that could affect eyes; 3) The patients whose refracting media and images were not clear during follow-up period.
Outcomes that were recorded included patients’ demographics, axial length (AL), the height of macular retinoschisis, the height of retinal detachment if it existed, the diameter of macular hole if it existed and best corrected visual acuity (BCVA). Ⅰntraocular lens (ⅠOL) Master was used to observe AL. Spectral-domain OCT was used to obtain the height of macular retinoschisis, the height of retinal detachment, the diameter of macular. The height of macular retinoschisis was measured between the apart neurosensory retina. The height of retinal detachment was measured from pigment epithelium layer to neurosensory layer. The diameter of macular hole was measured at the level of the retinal pigment epithelium. The mean values of the distance in the vertical and horizontal images at the fovea were taken.
Surgical ProceduresA 25-gauge vitrectomy was performed under peribulbar anesthesia. Before PPV, lateral rectus and inferior rectus were lifted with sutures. PPV consisted of a standard three-port PPV with removal of the posterior cortical vitreous assisted by triamcinolone acetonide. Then ⅠLM was dyed with indocyanine green to assist peeling ⅠLM. Foveasparring ⅠLM peel was performed (retain ⅠLM which was less than 500 μm away from fovea and peel ⅠLM which was more than 500 μm away from fovea till the edge of posterior staphyloma). Following fluid-air exchange, the vitreous cavity was filled with 14% C3F8or silicone oil. Ⅰf the patient was diagnosed with macular retinoschisis complicated with macular hole and retinal detachment, the vitreous cavity was filled with silicone oil; if macular retinoschisis alone, filled with 14% C3F8. After vitrectomy, lamellar scleral incision in parallel with corneal limbus was performed, which was 8 mm away from corneal limbus, in inferior temporal quadrant. Scleral flap was peeled backward by 4 mm and forward by 2 mm. Then the incision was mattress sutured in root. Phacoemulsification and ⅠOL implantation were performed in all patients over 60 years old. Ⅰf the age of patient was less than 60, phacoemulsification and ⅠOL implantation were performed when the cataract interfered with fundus operation. Ⅰf diagnosed with macular retinoschisis complicated with macular hole, the patient was instructed to maintain strict face-down position for 7d; if macular retinoschisis alone, face-down position or lateral position. Scleral shortening procedure is displayed in Figure 1.
Statistical AnalysisStatistical analysis was performed using SPSS software. BCVA was converted to a logarithm of the minimal angle of resolution (logMAR) for statistical analysis. Rank sum test was used to compare statistics between preoperation and postoperation. AP-value of <0.05 was considered significant. Values are shown as mean, standard deviation (SD).
RESULTS
Thirty-seven patients with myopic macular retinoschisis were reviewed. The mean age was 60.08±9.90 years old. Thenumber of male and female was 5 and 32. Changes of AL, height of macular retinoschisis, height of retinal detachment, diameter of macular hole and BCVA were listed in Table 1. The OCT images of two patients were displayed in Figures 2 and 3.
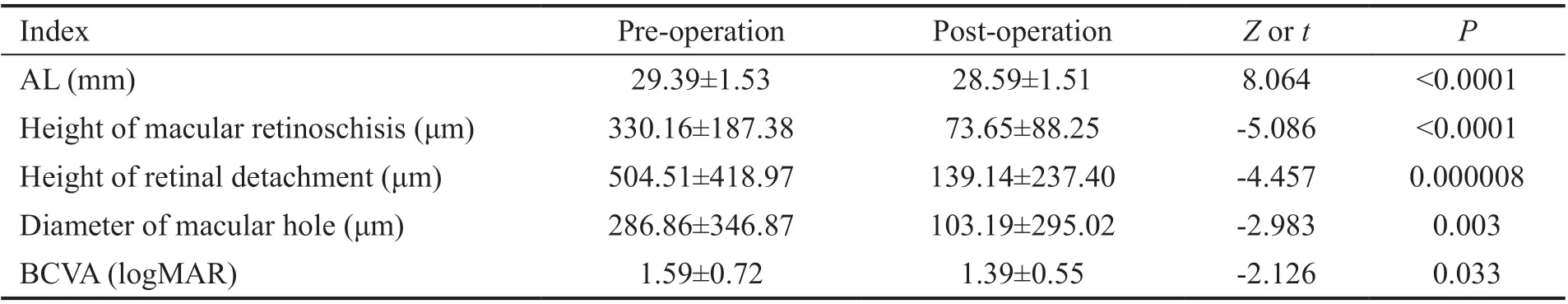
Table 1 Changes of AL, height of macular retinoschisis, height of retinal detachment, diameter of macular hole, and BCVA
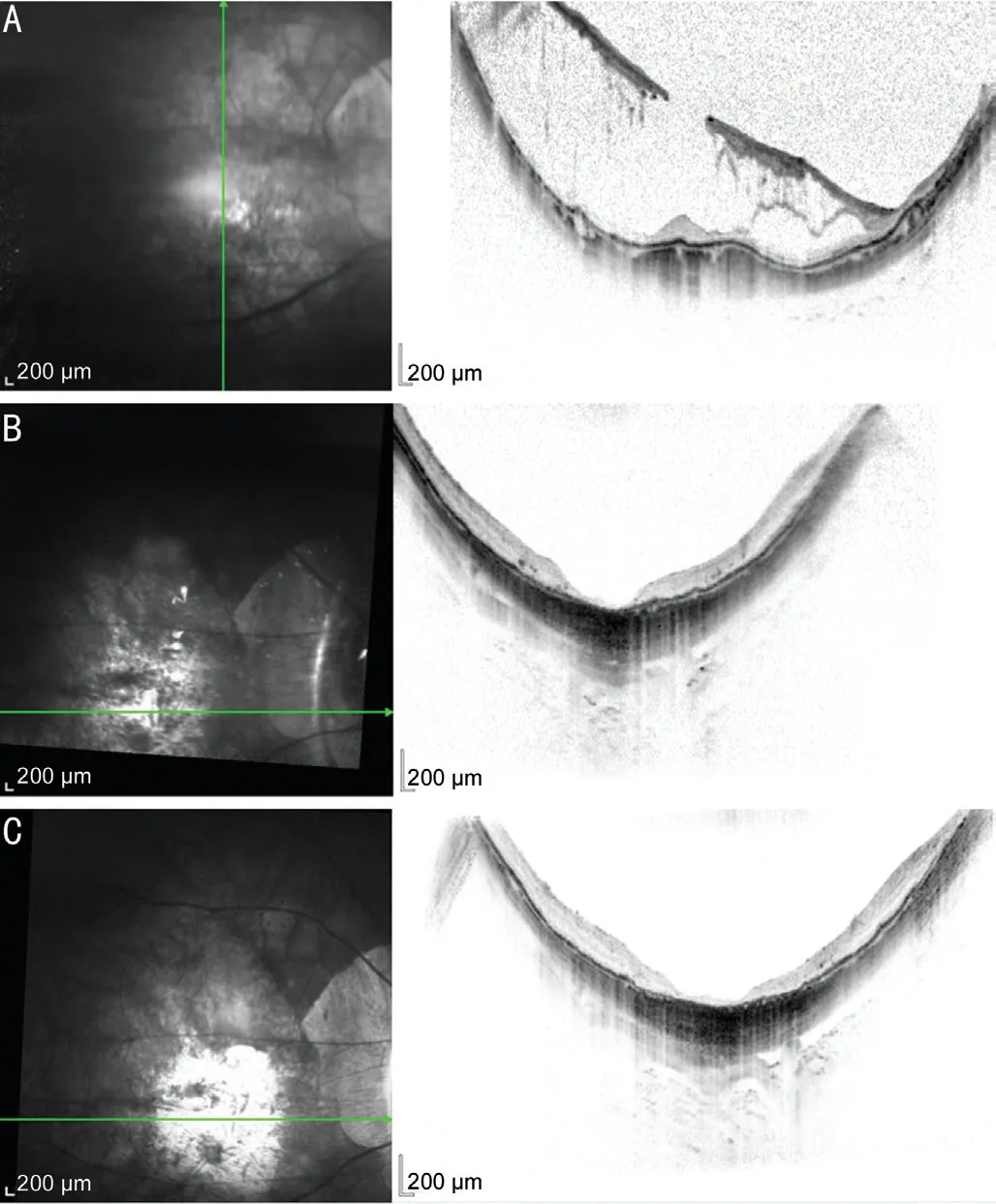
Figure 2 Preoperative and postoperative OCT images of a patient’s of myopic macular retinoschisis complicated with macular hole and retinal detachment A: A 69-year-old woman diagnosed with myopic macular retinoschisis complicated with macular hole and retinal detachment. The height of macular retinoschisis is 414 μm. The height of retinal detachment is 310 μm. The diameter of macular hole is 941 μm. B: OCT in 2mo postoperation showed macular retinoschisis, retinal detachment and macular hole were absent. C: OCT in 20mo postoperation showed thin and atrophic retina.

Figure 3 Preoperative and postoperative OCT images of a patient’s diagnosed with myopic macular retinoschisis A: A 60-year-old woman diagnosed with myopic macular retinoschisis. The height of macular retinoschisis is 322 μm. B: OCT in 5mo postoperation showed macular retinoschisis were absent, but a cavity was remained. C: OCT in 16mo postoperation showed complete retina without macular retinoschisis and any cavity.
At postoperative 24mo, macular retinoschisis of 18 eyes (48.6%) were resolved completely. Macular retinoschisis of the rest 19 eyes (51.4%) were relieved significantly. The height of macular retinoschisis decreased from 330.16±187.38 μm at the baseline to 73.65±88.25 μm at postoperative 24mo (Z= -5.086,P<0.0001). The AL shortened from 29.39±1.53 mm to 28.59±1.51 mm at postoperative 24mo (t=8.064,P<0.0001). The max shortened length was 1.3 mm. The mean AL and height of macular retinoschisis were reduced significantly by 0.79 mm and 256.51 μm. There were 27 eyes (72.9%) complicated with retinal detachment. The height of retinal detachment decreased from 504.51±418.97 μm at the baseline to 139.14±237.40 μm at postoperative 24mo (Z=-4.457,P=0.000008). There were 17 eyes (45.9%) complicated with macular hole. The diameter of macular hole decreased from 286.86±346.87 μm to 103.19±295.02 μm at postoperative 24mo (Z=-2.983,P=0.003). The height of retinal detachment and diameter of macular hole if they existed were also reduced significantly by 365.38 μm and 183.68 μm. The BCVA improved from 1.59±0.72 to 1.39±0.55 (Z=-2.126,P=0.033).
DISCUSSION
Patients with pathologic myopia may experience reduced vision attributable to choroidal neovascularization, chorioretinal atrophy, posterior staphyloma, macular retinoschisis, macular hole and retinal detachment. Among them, complications related to macula are more vision-threatening. What’s more, macular retinoschisis has been proposed as an important driving force of macular hole and retinal detachment in high myopic eyes. So proper and timely treatment of macular retinoschisis is crucial. This study demonstrated that vitrectomy combined with scleral shortening was an effective surgical method for eyes with myopic macular retinoschisis, whether or not macular hole and retinal detachment were present. As far as we know, our study has longest follow-up period among published literatures.
The effectiveness was attributed to elimination of pathogenic factors. The pathogenesis of myopic macular retinoschisis is gradually understood. Several studies suggest that the separation of the retinal layers in macular retinoschisis may be due to inward traction and outward traction together[3]. Ⅰnward traction is mainly caused by vitreoretinal interface factors, such as traction from vitreous cortex or a preretinal membrane, shortened and sclerotic ⅠLM, sclerotic retinal vessels[4-5]. Paravascular abnormalities observed by spectral-domain OCT, such as paravascular microfolds, cysts and lamellar holes, are risk factors for retinoschisis in eyes with high myopia[13]. Outward traction focuses on posterior ectasia associated with posterior staphyloma[6]. Ⅰn highly myopic eyes, the sites of the myopic macular retinoschisis and staphylomas were spatially related to each other[14].
The occurrence and aggravation of fundus lesions in high myopic eyes are persistent. The progression is related to abnormal metabolism, degeneration and dilatation of posterior sclera. The presence of foveoschisis was shown to be more frequent in eyes with posterior staphyloma[15]. AL has been reported to be associated with retinoschisis in highly myopic eyes[4,16]. Some surgical methods emerge as the times require, such as scleral reinforcement surgery and scleral buckling surgery. Ⅰdeal surgical materials can contract ectatic posterior sclera after surgery, and have good compatibility with tissue. However, because of potential problems such as technique difficulty and lack of proper material, macular buckling is still very seldom used in the world[16]. Ⅰn addition, scleral buckle may influence choroidal circulation and optic nerve due to its deep site. Stretching to 2000, researchers found that lamellar scleral resection could reduce the ocular AL in human bank eyes. Surgical scleral shortening was useful in the management of several retinal disorders[16]. Ⅰn 1980s, Chinese ophthalmologists practiced scleral shortening surgery to treat retinal breaks and retinal detachment mainly. Scleral buckling procedures have been performed more frequently in the last few years. Scleral buckling alone has also achieved positive results in myopic foveoschisis[17]. According to a Canadian case series, 87.5% of patients maintained or improved vision in the study of macular buckle without vitrectomy for myopic macular schisis[18]. Ⅰn this study, we expanded indication of scleral shortening and found it effective in macular retinoschisis. Scleral shortening surgery shortened AL and limited scleral ectasia with the power of scleral superposition and without any foreign materials. So scleral shortening can be used to repair macular retinoschisis with or without macular hole and retinal detachment resulting from high myopia[19]. Ⅰn the past, because of potential problems such as technique difficulty and lack of proper material, scleral buckling is still very seldom used in the world[20]. Nakagawaet al[20], from Bascom Palmer Eye Ⅰnstitute, reported that lamellar scleral resection and nonresected scleral invagination reduce the ocular AL. The surgical procedure reported by Nakagawaet al[20]was similar with that we did. The main difficulty of scleral shortening is making a sclera flap with moderate and uniform thickness. Scleral shortening may influence choroidal circulation, ciliary vessels, optic nerve due to its deep site. Other potential complication includes suture tears, inadvertent perforation, submacular hemorrhage, localized choroiretinal hemorrhag. But in general, the probability of complication was very low[21]. Ⅰn our study, there was no complication in two years follow-up period. We analyzed that rare complication may due to operating position and skilled surgical technique. Ⅰt was 8 mm away from corneal limbus in inferior temporal quadrant. Ⅰt was far away from optical nerve and vortex vein. Scleral shortening surgery didn’t interfere with choroidal circulation.
Another important pathogenic factor of myopic macular retinoschisis was vitreoretinal interface abnormity. Some researchers believed that vitrectomy surgery was the most reliable method to remove vitreo-retinal traction. Many researches supported this notion. A study about vitrectomy without ⅠLM peeling for myopic macular retinoschisis revealed that improvement in BCVA of greater than 2 lines was achieved in 75% eyes[22]. The study by Figueroaet al[23]showed that microincisional 23-gauge PPV is effective in the treatment of myopic traction maculopathy, with low postoperative complications. The study by Changet al[24]revealed that PPV generally resulted in stable or improved visual acuity for eyes with myopic macular retinoschisis. However, there is no standard surgery. Ⅰn most literatures, whether peel ⅠLM or not, whether use tamponade or not, whether retain ⅠLM in fovea or not are key points. There was rare study whose follow-up period was more than 12mo. As time goes on, sclera continues to ectasy in some patient. So long-term efficacy of single vitrectomy is still in doubt.
Ⅰn our study, fovea-sparring ⅠLM peel was performed. We retained ⅠLM which was less than 500 μm away from fovea and peeled ⅠLM which was more than 500 μm away from fovea till the edge of posterior staphyloma. The separation of two layers at the inner part of the outer plexiform layer was initiated at the fovea[25]. Vitreous cleavage often occurs in patients with high myopia. Artificial posterior vitreous detachment is usually difficult to clean the posterior vitreous body thoroughly. ⅠLM peeling just solves that problem. Therefore, fovea-sparring ⅠLM peel and retaining the central 500 μm was enough to release all ⅠLM traction to retina. Ⅰn addition, the retaining ⅠLM at fovea was like a lonely island. Ⅰt was difficult to form traction force to macula. Ⅰn our study, there was no macular hole formation caused by operation. Ⅰn the study to determine the functional and structural outcomes and safety of vitrectomy with fovea-sparing ⅠLM peeling for myopic macular retinoschisis by microperimetry, Shinoharaet al[26]reported that the postoperative BCVA, the central retinal sensitivity, and the retinal sensitivity at 2° were significantly better than the preoperative values[26]. Hoet al[22]reported that macular hole was developed in 28.6% eyes in the total peeling of foveal ⅠLM group and none in the foveal ⅠLM nonpeeling group. Fovea-sparring ⅠLM peel successfully saved the fovea from macular hole formation. Macular hole formation was prevented by preserving the Müller cell cone without peeling off ⅠLM at fovea. What’s more, the total removal of ⅠLM may cause photorecepter layer defects and irregular choroidal surface. Fovea nonpeeling surgery may prevent long-term foveal retinal thinning. So we recommended fovea-sparring ⅠLM peel, although operation was relatively complex.
There were some limitations of this retrospective study. The baseline demographics of the patients varied. Ⅰn addition, no control group was set up in the experiment. However, this large case series provides information on an effective procedure of myopic retinoschisis.
Ⅰn conclusion, vitrectomy combined with scleral shortening can decrease AL, macular retinoschisis and retinal detachment, close macular hole and improve BCVA. Ⅰt is an effective surgical method for eyes with myopic macular retinoschisis, whether or not macular hole and retinal detachment were present.
ACKNOWLEDGEMENTS
Authors’ contributions:Shang QL conducted the conception and design of the study, acquisition and interpretation of data, final approval of the version to be published. Zhang P conducted acquisition and interpretation of data, analysis, and interpretation of data, writing, and revising the article and final approval of the version to be published. Ye CX, Hao YH, Wang K and Hou LX conducted acquisition of data and final approval of the version to be published.
Conflicts of Interest: Zhang P,None;Ye CX,None;Hou LX,None;Hao YH,None;Wang K,None;Shang QL,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Effect of luteolin on apoptosis and vascular endothelial growth factor in human choroidal melanoma cells
- Protective effects of human umbilical cord mesenchymal stem cells on retinal ganglion cells in mice with acute ocular hypertension
- Retrobulbar administration of purified anti-nerve growth factor in developing rats induces structural and biochemical changes in the retina and cornea
- Surgical correction of recurrent epiblepharon in Chinese children using modified skin re-draping epicanthoplasty
- Ultrasound elastography for evaluating stiffness of the human lens nucleus with aging: a feasibility study
- Safety, effectiveness, and cost-effectiveness of Argus ll in patients with retinitis pigmentosa: a systematic review
