Transradial vs transfemoral secondary access outcomes in transcatheter aortic valve implantation:A systematic review and meta-analysis
2020-12-17ShreeLataRadhakrishnanKalonKLHo
Shree Lata Radhakrishnan,Kalon KL Ho
Abstract
Key Words:Transcatheter aortic valve implantation;Meta-analysis;Femoral access;Radial access;Secondary access;Transcatheter aortic valve replacement
INTRODUCTION
The transcatheter aortic valve implantation (TAVI) procedure is a promising alternative to surgical aortic valve replacement in patients with aortic stenosis.As with any procedure,TAVI is not without complications.Bleeding,vascular complications,and strokes are some of the most common adverse events associated with TAVI.These complications are often associated with the type of access used in the procedure.
TAVI utilizes two vascular access sites—primary and secondary.The valve itself is delivered through the primary access site,while the secondary access site is used for the introduction of catheters for angiography,aiding in device placement,and obtaining invasive hemodynamic data[1].Options for primary access include transfemoral,transaortic,transapical,and subclavian,among others,out of which transfemoral has been the most popular.The two main sites used for secondary access are the contralateral femoral artery and either radial artery.Historically,the transfemoral site was chosen as the preferred secondary access site.However,during recent years,the transradial site has shown promising results with lower complication rates.There are a handful of studies,mostly with relatively small sample sizes,directly comparing outcomes in transfemoral (TF) and transradial (TR) access sites[1-6].These studies have suggested that the transradial site for secondary access has better outcomes than the transfemoral site for bleeding and vascular complications.The aim of this review is to pool data from available relevant studies to compare outcomes between TR and TF secondary accesses.
MATERIALS AND METHODS
Search strategy
This study was registered on PROSPERO on May 7,2020,and the meta-analysis was conducted using PRISMA guidelines.A comprehensive literature search was conducted through June 10,2020 using PubMed,EMBASE,Google Scholar,and Cochrane databases.Search words included “transfemoralvstransradial secondary access in transcatheter aortic valve replacement” and “radialvsfemoral secondary access in TAVI.” Literature search was conducted independently by two investigators(Radhakrishnan SL and Darmoch F—see acknowledgement) using the above search strategy.There was uniform agreement between both investigators on what studies to include and exclude,resulting in a kappa correlation of 1.
Inclusion criteria
All observational or experimental trials which aimed at comparing data related to secondary access in patients who underwent TAVI were considered in this review,irrespective of primary access.We included studies if they reported data comparing outcomes between transradial and transfemoral secondary access.Studies considered had to include tables comparing demographics and other baseline characteristics and outcomes.The outcomes considered for the purpose of this review were 30-d all-cause mortality,30-d stroke,30-d bleeding complications,and 30-d vascular complications.Studies were included if they reported at least one of the four outcomes in the format desired (comparing TRvsTF).
Exclusion criteria
Studies that did not meet inclusion criteria based on title were excluded.Studies that did not report data specifically related to secondary access in TAVI procedures in the format desired were also excluded.Letters to the editor,abstracts,and posters were excluded.
Statistical analysis
Statistical analysis was performed using Review Manager 5.3.Subgroup analysis was only done if data were reported in at least four studies to increase confidence in the findings.The test statistic calculated in this meta-analysis was the odds ratio.A random-effect model was chosen over a fixed-effect model since the underlying population in each study was thought to be different.Heterogeneity was determined by theI2value to describe the percentage of variability due to heterogeneity rather than due to sampling bias.The higher theI2value,the higher the heterogeneity.That is,anI2of <50% indicates more similarity between studies.APvalue of 0.05 or less was considered to be significant for all test statistics.Funnel plots were created to assess for evidence of bias and to determine heterogeneity.Results are expressed as mean ± standard deviation,with 95% confidence intervals for odds ratio denoted by square brackets.
RESULTS
Identification of eligible studies
Using the search strategy described above resulted in 2701 articles (2690 from Google scholar,5 from PubMed,5 from Embase,and 1 from Cochrane Central).Of these,2690 articles were excluded after title and/or abstract review,and 1 trial was still in process and unpublished.Each of the remaining 10 articles was reviewed in full.Of these,2 letters,1 poster,and 1 duplication were excluded.Although a study by Wynneet al[1]was an observational study which focused on the topic of interest,results reported were not dichotomized based on the type of secondary access and hence excluded from the meta-analysis.Five remaining studies were included in the meta-analysis[2-6].Detailed results of the search strategy are outlined in Figure 1.
Study characteristics
All 5 studies included were observational cohort studies.Definitions of bleeding and vascular events were based on Valve Academic Research Consortium-2 (VARC-2)criteria in 4 studies and the original VARC criteria in 1 study (Curranet al[3]).All studies provided outcomes comparing transradial secondary access (TRSA) with transfemoral secondary access (TFSA).The primary access was solely femoral in 2 studies (Fernandez-Lopezet al[6]and Curranet al[3]).Allendeet al[4]and Jacksonet al[5]reported data on all primary accesses (APA,i.e.,femoral and non-femoral primary accesses) with distinction in comparative outcomes based on transfemoral primary access (TFPA)vsnon-TFPA.In Junqueraet al[2],the study included APA subjects.However,it did not separately provide comparative data on TFPA subjects.Due to the lack of uniformity in the type of primary access,most of the analyses in the study mainly focused on APA.The 2 studies that reported only TFPA outcomes were considered as APA for practical purposes.A separate analysis was also done for TFPA alone,thus excluding Junqueraet al[2].Relevant study characteristics are outlined in Table 1.
Of the 5 studies,risk adjustment in some manner was reported in 3 of 5 studies.When available,matched/adjusted scores were used;however,if no adjustment or matching was reported,the study was still included in this review.Allendeet al[4]adjusted data for differences in gender and peripheral disease.Fernandez-Lopezet al[6]reported that results were adjusted for age,Euroscore,body mass index,New York Heart Association (NYHA) functional class,type and size of valve.Junqueraet al[2]reported both overall unadjusted data and propensity score-matched data.Jacksonet al[5]and Curranet al[3]did not report having performed specific risk adjustment or matching.
In Junqueraet al[2],both unadjusted as well as propensity score-matched data were reported.For the purpose of this study,only propensity score-matched data was included.

Figure 1 Flowchart outlining search strategy and article-selection process.
Study results
A total of 5065 patients underwent TAVI inclusive of APA,with 1453 patients (28.7%)having TRSA and 3612 patients (71.3%) having TFSA.A secondary analysis was conducted in patients that underwent TAVI with TFPA.Four out of 5 studies qualified for the TFPA sub-group analysis.The total population of this cohort was 898 patients,out of which 496 patients (55.2%) underwent TRSA and 402 (44.8%) patients underwent TFSA.
Baseline demographics in each study are compared in Table 2.The mean age of the study population was 81.1 ± 7.2 in the TFSA group and 81.3 ± 7.1 in the TRSA group.Forty six percent (46%) were males in the TFSA group and 53% in the TRSA group.Atrial fibrillation was present in 26% of subjects in the TFSA group and 28% in the TRSA group.The mean STS-PROM score was 6.4 in the TFSA group and 6.0 in the TRSA group.
Results of APA procedures
All-cause mortality:When APA-TAVI procedures were considered,the 30-d all-cause mortality rate was 2.6% in the TRSA group and 4.4% in the TFSA group,odds ratio(OR) 0.59 [0.41,0.86] (P= 0.006,Figure 2A).
Stroke:The 30-d stroke rate was 1.5% in the TRSA group and 3.2% in the TFSA group,OR 0.45 [0.29,0.74] (P = 0.001,Figure 2B).
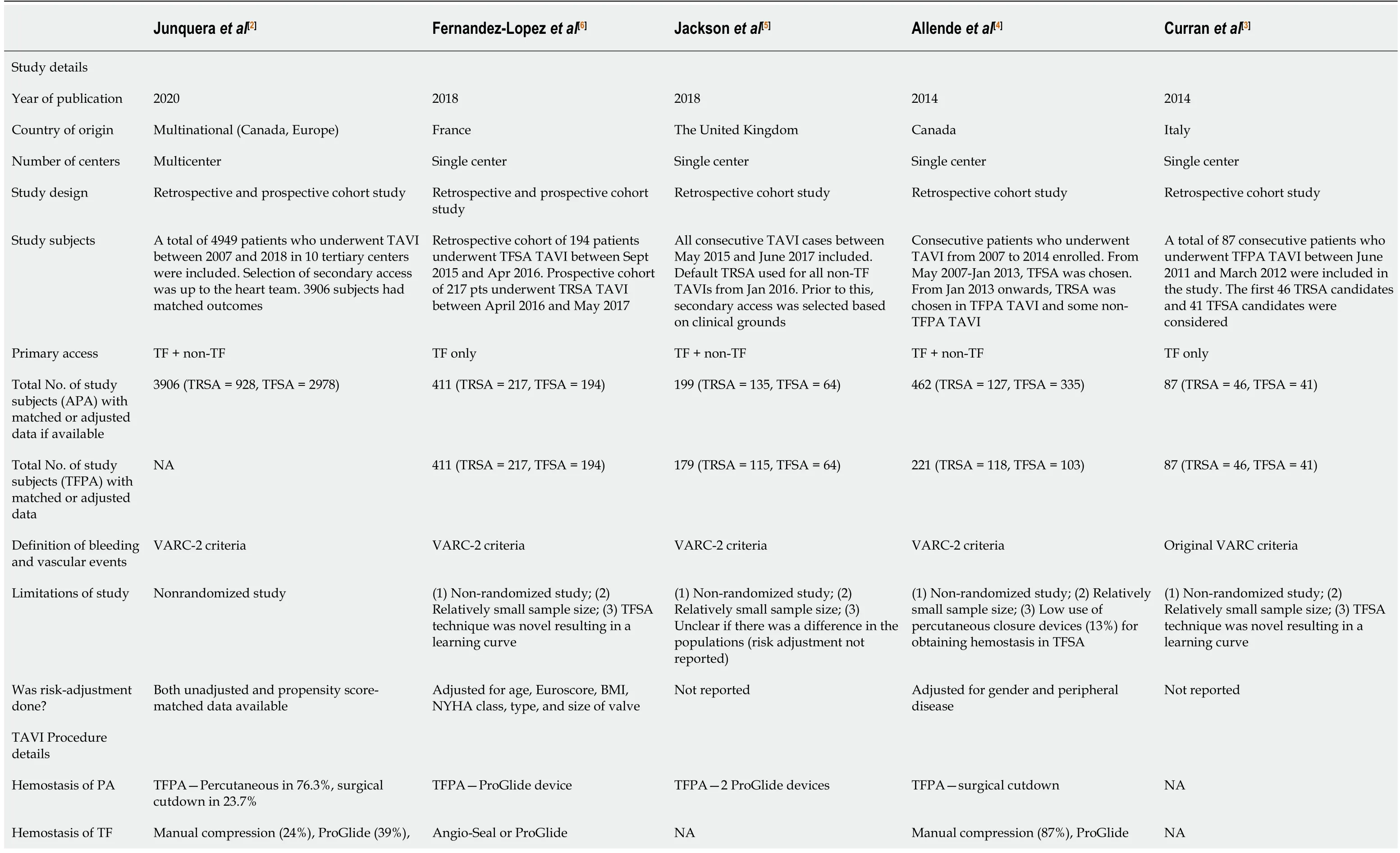
Table 1 Characteristics and procedure details of included studies

TF:Transfemoral;TR:Transradial;APA:All primary access;TFPA:Transfemoral primary access;TFSA:Transfemoral secondary access;TRSA:Transradial secondary access;TAVI:Transcatheter aortic valve implantation;NYHA:New York Heart Association;BMI:Body mass index;VARC:Valve Academic Research Consortium;NA:Not available.
Bleeding complications:The incidence of major and life-threatening bleeding complications by 30 d post-TAVI was 3.4% in TRSA patients and 6.3% in TFSA,OR 0.40 [0.28,0.56] (P<0.00001,Figure 2C).
Vascular complications:Major vascular complications by 30 d post-TAVI were seen in 2.8% of TRSA patients and 5.9% in TFSA,OR 0.48 [0.33,0.69] (P<0.0001,Figure 2D).The incidence of 30-d minor vascular complications was 11.7% in TRSA patients and 12.4% in TFSA,OR 0.92 [0.75,1.12] (P= 0.41,Figure 2E).
Figure 3 shows funnel plots for the main outcomes.The plots were symmetric,and all studies lie within the triangular region,close to the mean,without outliers.This indicates minimal heterogeneity in this review.Figure 4 shows traffic light plots of the domain-level judgements for each individual result to assess risk of bias.
Results of TFPA procedures
All-cause mortality:The 30-d all-cause mortality rate was 2.8% in the TRSA group and 4.7% in the TFSA group,OR 0.62 [0.31,1.26] (P= 0.19,Figure 5A).
Stroke:The 30-d stroke rate was 1.2% in the TRSA group and 4.2% in the TFSA group,OR 0.31 [0.12,0.77] (P= 0.01,Figure 5B).
Bleeding complications:In patients who had TFPA during their TAVI,major/Lifethreatening bleeding complications were seen by 30 d in 6.3% of TRSA patients and 11.2% in TFSA,OR 0.52 [0.32,0.85] (P= 0.008,Figure 5C).
Vascular complications:This was not analyzed for the TFPA group,as only 3 out of 5 studies reported on this outcome in the TFPA group.
DISCUSSION
Main findings
In this meta-analysis,we found that patients who underwent TRSA had significantly lower odds than those with TFSA of developing 30-d mortality,stroke,bleeding,and major vascular complications.When APA site procedures were considered,the odds of mortality up to 30 d after the procedure were found to be 41% lower,and the odds of 30-d stroke 54% lower in the TRSA group than the TFSA group.Similarly,the odds of having major or life-threatening bleeding were 60% lower in the TRSA group than the TFSA group.The odds of having major vascular complications were 52% lower in the TRSA group.Our findings are consistent with previously published data[1-10],which have also reported that TRSA has lower odds of complications.

Table 2 Demographic comparison based on secondary access of matched/adjusted data (if available)
When TFPA alone was considered,there was no significant difference in 30-d mortality between the TRSA and TFSA groups as opposed to the APA group which showed a significant decrease in mortality in the TRSA group.The absolute mortality rates and odds ratio in the APA and TFPA cohorts were,however,comparable.This discrepancy in statistical significance can be attributed to the smaller sample size in the TFPA group.There were significantly lower odds of having a stroke or major/lifethreatening bleeding in the TRSA group compared with the TFSA group in the TFPA cohort.

Figure 2 Forest plots for all primary access outcomes.
The transradial access has some advantages over transfemoral access.For one,the transradial site is more easily compressible in case of bleeding complications[11-13].It also avoids the need to puncture both femoral arteries[3].These advantages could lead to improved rates of vascular complications when compared with femoral secondary access.The disadvantage of radial access is that it does not allow the use of other interventional devices[11,13].Some other challenges include difficulty navigating in case of anatomical variations and the possibility of developing radial artery occlusion with larger catheter diameters.
This review has several limitations.One major limitation of this meta-analysis is that all studies included were non-randomized.No randomized studies on this topic have been published yet.Hence there is high risk for selection bias.Risk adjustment or propensity score-matching was done in some studies.Two studies did not report on risk adjustment or matching in their study,hence there is a possibility of differences in their study populations.Moreover,unmeasured confounders cannot be accounted for.To improve confidence in the results,subgroup analysis was done only if data were reported in at least four studies.On another note,there was no uniformity in the type of primary access among studies.Few studies reported outcomes in the TFPA subgroup.This was a small fraction of the overall study population and results were mostly similar to APA results.Lastly,the presence of a learning curve should be considered,with the assumption that complication rates improve with experience.Due to the novelty of the procedure when initially adapted in some of these studies,one could assume that complications were more likely to occur in the early phase of implementing this procedure.In experienced operators,complication rates would likely be lower.This could skew the study results accordingly,especially if radial secondary access was adopted later in institutional experience.
CONCLUSION
In patients undergoing transcatheter aortic valve implantation (TAVI),irrespective of primary access,those who underwent TRSA had lower complication rates than those who underwent TFSA.In the absence of contraindications,a transradial approach for secondary access seems preferable in TAVI procedures.Confirmation by randomized controlled studies of TAVI procedures stratified by primary access site would be useful to adjust for primary access while comparing secondary access-related outcomes.

Figure 3 Funnel plot for all primary access outcomes.

Figure 4 Traffic light plots of the domain-level judgements for each individual result to assess risk of bias.

Figure 5 Forest plots for trans femoral primary access outcomes.
ARTICLE HIGHLIGHTS
Research background
Complications of transcatheter aortic valve implantation (TAVI) procedures include bleeding,vascular complications,and strokes.These complications are often associated with the type of access used.Access can be primary or secondary.Few studies have been published on the effect of secondary access on outcomes.
Research motivation
The objective of this meta-analysis is to investigate if transradial secondary access(TRSA) has fewer complications than transfemoral or vice versa,with the hope of reducing complications in TAVI procedures related to access.
Research objectives
This systematic review aims to compare outcomes between transradial vs transfemoral secondary access (TFSA).
Research methods
A systematic search was conducted using major databases (EMBASE,PubMed,Cochrane Central,Google Scholar),which resulted in 5 studies that met criteria for study selection.Outcomes of interest were 30-d rates each of major/life-threatening bleeding,vascular complications,strokes,and mortality.All 5 studies were observational.Adjusted or matched data were used if reported.
Research results
A total of 5065 patients underwent TAVI,with 1453 patients (28.7%) having undergone TRSA and 3612 patients (71.3%) TFSA.Irrespective of the site of primary access,the odds of having major or life-threatening bleeding were 60% lower in the TRSA group than the TFSA group (P<0.00001).The odds of having major vascular complications were 52% lower in the TRSA group (P<0.0001) with no difference in minor vascular complications between the 2 groups.Similarly,the odds of mortality in 30d after the procedure were 41% lower (P= 0.006) and the odds of stroke were 54%lower (P= 0.001) in the TRSA group than the TFSA group.
Research conclusions
TRSA appears to be a safer alternative to the TFSA in TAVI procedures.
Research perspectives
Our findings need to be confirmed in randomized clinical trials,which should minimize selection bias and both measured and unmeasured confounding.
ACKNOWLEDGEMENTS
The authors are grateful for the assistance of Darmoch F,MD,in conducting the literature search.
杂志排行
World Journal of Cardiology的其它文章
- Effectiveness and safety of antithrombotic strategies in elderly patients with acute myocardial infarction
- Endothelial progenitor cells mobilization after maximal exercise according to heart failure severity
- Rapid right ventricular pacing for balloon valvuloplasty in congenital aortic stenosis:A systematic review
- Effects of left ventricular assist device on pulmonary functions and pulmonary hemodynamics:A meta-analysis
- Medical therapy vs early revascularization in diabetics with chronic total occlusions:A meta-analysis and systematic review
- Cardiac adverse events of immune checkpoint inhibitors in oncology patients:A systematic review and meta-analysis
