Medical therapy vs early revascularization in diabetics with chronic total occlusions:A meta-analysis and systematic review
2020-12-17MuhammadShayanKhanFarhadSamiHemindermeetSinghWaqasUllahMaenAlDabbasKhalidHamidChangalTanveerMirZainAliAmeerKabour
Muhammad Shayan Khan,Farhad Sami,Hemindermeet Singh,Waqas Ullah,Ma'en Al-Dabbas,Khalid Hamid Changal,Tanveer Mir,Zain Ali,Ameer Kabour
Abstract
Key Words:Coronary angiography;Diabetes mellitus;Percutaneous coronary Intervention;Coronary bypass grafts;Chronic total occlusions;Mortality
INTRODUCTION
Chronic total occlusion (CTO) of a coronary artery is defined as a 100% stenosis with thrombolysis in myocardial infarction 0/I flow for greater than 3 mo[1,2].The prevalence of CTOs ranges from 18%-26% in all patients with coronary artery disease(CAD) and almost 50% in patients with previous coronary artery bypass grafting(CABG)[3].Around 10% of patients with acute myocardial infarction (MI) are also found to have CTOs[3].Presence of CTO is associated with lifestyle impairment,reduced cardiac performance and poor long-term outcomes[3,4].Given the complex nature and uncertainty regarding mortality benefit from revascularization,these lesions were traditionally treated with optimal medical therapy (OMT).However,with recent advancement in percutaneous techniques and greater operator experience along with better patient selection,there has been an increase in the trend of CTO interventions in contemporary practice.
In this complex subset of CAD population,diabetic patients are particularly at higher risk of poor outcomes as compared to their non-diabetic counter-parts[5-7].Despite lack of sufficient studies,recent evidence suggest that successful CTO revascularization is associated with improved outcomes of quality of life,left ventricular systolic function and potentially survival in general population[8,9].However,limited data exists regarding long-term outcomes in diabetic patients with CTO treated with revascularization.We,therefore,conducted this meta-analysis of randomized clinical and observational studies to compare clinical outcomes with revascularizationvsoptimal medical therapy in diabetic patients with CTO.
MATERIALS AND METHODS
We followed the preferred reporting items for systematic reviews and meta-analyses guidelines,a checklist of which is available as supplementary material[10].
Search strategy
A predefined inclusion criterion was established in advance.Potentially relevant published clinical trials were identified in Medline,Embase,chemical abstracts and Biosis (from start of the databases till date).The following search items were used to search titles and abstracts:(Optimal medical therapy? or OMT? Or intensive medical therapy or IMT or revascularization? Or prompt revascularization or early revascularization? And diabetic or type 2 diabetes or DM and chronic total occlusion or CTO and clinical trials.Due to scarcity of data,both observational and interventional studies were included.Studies were limited to involving humans only.
Selection criteria
Two researchers independently performed an electronic search of pub med and web of science databases.No language restrictions were made.Studies were included if they met the following criteria;intervention with OMT and early revascularization (PCI or CABG) in diabetics as variables and primary outcome of interest as all cause death.Secondary outcomes included cardiac death,prompt revascularization (ER) or repeat MI.Studies were included if successful revascularization (CABG or PCI) was performed within six weeks of randomization or start of study.Both short and long term follow ups were included in literature review.48 articles were identified after the search.The second selection step involved proof-reading of those articles to ensure the first step was performed correctly.Articles were excluded if data on OMT or prompt revascularization (ER) was missing,trials did not include diabetic subjects or primary and secondary outcomes of interest were not available.In case of un-clarity,inclusion of the studies was discussed amongst the authors to arrive at a final decision.
Data extraction and statistical analysis
Data was extracted from each study using a standardized spread sheet which involved study identification (Author,year of publication and country),study type,percent males,subject baseline characteristics with history of coronary artery disease,number of cases in OMT and ER arms,time of follow up,type of stent used (Drug elutingvsbare-metal),exclusion criteria and quality scoring.
To calculate the overall effect outcome,generic inverse variance tool under the random effects model to calculate pooled hazard ratios (HR) was performed using Cochrane's review manager.The “test for overall effect” was reported as z value corroborating inference from the 95% confidence interval (CI),and the probability value ofP<0.05 was considered statistically significant.Higgins I-squared (I2) statistic model was used to assess variations in outcomes of included studies.I2 values of 50%or less corresponded to low to moderate,and 75% or higher indicated large amounts of heterogeneity.Publication bias was illustrated graphically using a funnel plot asymmetry.The methodological quality of included articles was performed using the Cochrane guidelines for systematic review and meta-analysis.
We also assessed quality using a scoring system based on the Delphi consensus for meta-analysis[11].The following criteria were used for scoring:Proper randomization(Score:1 point),similarity of treatment groups in relevant variables at baseline (1 point),blinding of subjects and investigators (1 point for each),specified eligibility criteria (1 point),valid point estimates and measures of variability (1 point) and data on degree of compliance (1 point).Thus,a combined score was calculated for each study which could range from 0 to 7 points.For the observational studies,a score of 0 was given for randomization.Quality scores for each study have been illustrated in Table 1.
RESULTS
The search through Pub med and Med of science databases yielded 48 potentially relevant articles.Based on predefined exclusion criteria,44 papers were excluded for various reasons.1 Randomized control trial[12]and 3 observational studies[13-15]involving a total of 2448 subjects were included in the meta-analysis.The number of subjects ranged from 236 in Yanet al[15]to 972 in Damlujiet al[12].Mean age ranged from 59.2 years in Yanet al[15]to 68.5 years in Flores-Umanzoret al[13]Reported compliance was 100%.Follow up time ranged from 45 mo in Yanet al[15]To 60 mo in Damlujiet al[12]as above,studies were included if successful revascularization (CABG or PCI) was performed within six weeks of randomization or start of study.OMT included pharmacological therapy as well as lifestyle modification.Pharmacologic therapy across the studies included antiplatelet therapy (as needed),maximum tolerated dose of anti-anginals (B-Blocker plus a long acting nitrate and/or a calcium channel blocker) and statins.Baseline characteristics of all studies have been illustrated in Table 1, with the major co-morbidities across all studies in Table 2.Among studies with reported data,right coronary artery was the vessel most commonly diseased(Table 3).
Primary effect outcome
Three out of four studies reported long term all-cause mortality.There was a 70%increase in risk of pooled all-cause mortality in the OMT group,although the confidence interval did cross 1, (HR:1.70,95%CI:0.80-3.26,P= 0.11,see Figure 1A).Significant heterogeneity was observed,(I2= 88%,P= 0.0003).After removing the study by Flores-Umanzoret al[13],no significant heterogeneity was seen,(I2= 28%,P=0.24) however,pooled results were similar, (HR:1.21,95%CI:0.79-4.19,P= 0.38,Figure 1B).In order to assess for publication bias,a funnel plot for each study was constructed against their respective precisions.Absence of publication bias is reflected in an intercept close to zero with the slope of regression line close to overall effect size.Although the small number of studies limited its interpretation however,a subjective impression of funnel plot demonstrated no publication bias.
Secondary effect outcomes
All four studies reported long term cardiac mortality.The long-term HR for cardiac mortality was 1.68 with 95%CI:0.96-2.96 andP= 0.07 in the OMT group with an overall 68% increased risk as compared to the ER group,results were close to significance (Figure 1C).Significant heterogeneity was again observed, (I2= 76%,P=0.006).After removing Flores-Umanzoret al[13]from the analysis,mortality was higher in the OMT group,however the CI crossed 1, (HR:1.24,95%CI:0.85-1.81,P= 0.27).
Data for repeat MI was available for all four studies.No significant differences in the hazard ratio were observed between the two groups.(HR:0.97,95%CI:0.61-1.54,P= 0.90,Figure 2A).No significant heterogeneity was observed, (I2= 41%,P= 0.16).
All four studies reported data on repeat revascularization (PCI and CABG).There was a 62% increase in risk of repeat revascularization in patients assigned to medical therapy,and results were statistically significant, (HR:1.62,95%CI:1.36-1.94,P<0.00001,Figure 2B).No publication bias or study heterogeneity was observed,I2= 0%.
Subgroup analysis
Sub-group analysis stratified by mode of revascularizationi.e.CABG or PCI was also performed for both primary and secondary effect outcomes.Only Flores-Umanzoret al[13]provided data on both PCI and CABG where as two studies provided data on PCI only.Thus,subgroup analysis was done only for PCI.
For all-cause mortality,sub group analysis of OMTvsPCI revealed a 98% increased risk in the OMT group, (HR:1.98,95%CI:1.36-2.87,P= 0.0003,Figure 3A).This was statistically significant with no significant heterogeneity, (I2= 0,P= 0.83).
Similarly,sub-group analysis for cardiac mortality was also done comparing PCIvsOMT.Three out of four studiesi.e.,Flores-Umanzoret al[13]and Yanet al[15]provided data on PCI.There was an 87% increased risk of cardiac mortality in the OMTvsPCI group, (HR:1.87,95%CI:0.96-3.62,P= 0.06,Figure 3B).Results were not statistically significant with moderate heterogeneity, (I2= 60%,P= 0.08).

Table 1 Baseline characteristics of all studies
Three out of four studiesi.e.Flores-Umanzoret al[13],Choiet al[14]and Yanet al[15]provided data on risk of repeat MI.OMT was relatively safer in regards to occurrence of repeat MI as compared with PCI with a decreased HR, (HR:0.53,95%CI:0.31-0.91,P= 0.02,Figure 3C).No heterogeneity was observed,I2= 0%,P= 0.87.
For repeat revascularization,sub group analysis of OMTvsPCI revealed no difference in HR between the two groups.(HR:1.00,95%CI:0.52-1.93,P= 1.00, Figure 3D).
DISCUSSION
In this meta-analysis of randomized controlled and observational studies comparing diabetic patients with CTOs,patients in the OMT group were found to have a higher risk of all-cause and cardiac death as compared to ER.We included 4 studies for a total of 2448 patients.1252 patients were treated with OMT while 1196 patients underwent early revascularization.Damlujiet al[12]which is a post hoc analysis of the bypass angioplasty revascularization investigation 2 diabetes trial,evaluated the influence of CTO on long term clinical outcomes of patients with coronary artery disease and diabetes mellitus.We extracted the data for CTO only from Damlujiet al[12]to calculate mortality and morbidity outcomes in diabetics,however,our results were nonsignificant as shown in Figures 1A-1C further 3 observational studies were added to our meta-analysis to achieve the above results.We found that there was a trend of improved survival with ER either with CABG or PCI in terms of cardiac and all cause death.To our knowledge,this is the first ever meta-analysis of clinical trials comparing morbidity and mortality outcomes in diabetic patients with a CTO.Our subgroup analysis also revealed poor performance of PCIs vs OMT in terms of incidence of combined fatal and non-fatal MI.Further stratification could not be performed due to paucity of data.

Table 2 Percentage prevalence of co-morbidities across studies (actual prevalence in brackets)

Table 3 Chronic total occlusions location with number of chronic total occlusions lesions among studies in percentages (actual prevalence in brackets)
Given the complex nature and uncertainty regarding mortality or morbidity benefits from percutaneous or surgical revascularization,CTO lesions have been traditionally treated with OMT.Historically,the standard of care for revascularization of CTO lesions has been CABG with little evidence of superiority over OMT.However,with recent advancement in percutaneous techniques and greater operator experience along with better patient selection,there has been an increase in trend of CTO interventions in contemporary practice[16,17].Although observational data has shown a reduction in Major Adverse Cardiac Events,global left ventricular ejection fraction and quality of life after revascularization of CTO,results from these trials are inconsistent[18,19].Currently the global expert consensus statement recommends PCI revascularization for ischemic symptom improvement for which data is more unanimous[20].
Diabetes mellitus is a major risk factor of CTO.Around 34%-40% of patients with CTO have a history of diabetes[13]and there is a well-known association with worse outcomes from CTO in diabetics[5-7,13].Diabetes leads to endothelial cell dysfunction and changes in microcirculation,a prothrombotic/proinflammatory state along with impaired formation of coronary collaterals[7,8,21].This causes aggressive progression of atherosclerosis within the arterial bed including the coronary arteries leading to poorer outcomes in patients with CAD[22].PCI in diabetic patients also has a higher risk of instent restenosis,repeat revascularization,MI,stent thrombosis and death when compared to non-diabetics[23-25].
By performing a post hoc analysis of the bypass angioplasty revascularization investigation 2 diabetes trial,Damlujiet al[12]was the first to compare clinical outcomes in patients with both diabetes and coronary artery disease.They found that a lot of diabetic patients with CAD had a high prevalence of CTOs,approximately 41%.Although the primary outcome studied was the effect of CTOs on mortality in diabetics with a strongly positive correlation,we extracted the data for the CTO subgroup only for our analysis and found that OMT was associated with a higher risk of all cause and cardiac mortality in diabetics.Patients undergoing early revascularization were also noted to have a lower risk of repeat MI and repeat revascularization at long term follow up.Damlujiet al[12]and Choiet al[14]however did not perform a subgroup analysis on the revascularization modality choseni.e.,CABGvsPCI.
Our subgroup analysis (OMTvsPCI) revealed inferiority of PCI as a revascularization strategy in terms of repeat MI and repeat revascularization to the combined PCI and CABG group.This discrepancy in results is an interesting observation from the PCI subset as compared to the combined revascularization pool.This could imply superiority of CABG over PCI in these patients but these results might be confounded by disease anatomy and various comorbidities.Studies designed to compare CABG and PCI for this purpose can be helpful in the future.Also,the current success rates of CTO-PCI in the general population are from 80%-85%,however the majority of our trials demonstrated a lower success rate[26].One possible explanation for this discrepancy could be recent advancements in percutaneous techniques and equipment,however it is well known that diabetic patients have a higher burden of CAD with more complex disease anatomy which might be difficult to completely re-vascularize[27].In a meta-analysis of 35 studies including 89883 patients,Garciaet al[28]demonstrated that CABG was twice as likely as PCI to achieve complete revascularization in patients with CTOs.The study by Flores-Umanzoret al[13]included in our meta-analysis also noted higher rates of anatomic and functional complete revascularization in CABGvsPCI patients (63% and 62%vs36%and 32%,P<0.01).Subsequently,they also reported statistically significant lower allcause and cardiac mortality with CABG when compared to MT group but not with PCI.
Another important factor to consider in these patients is the presence or absence of chronic kidney disease (CKD).Studies have shown that renal dysfunction is an independent risk factor for cardiovascular disease,with higher mortality rates for both myocardial infarction and sudden cardiac death[29,30].Our patients in Choiet al[14]and Yanet al[15]were case-control matched according to the presence or absence of CKD,however,further data on this sub-group was not available for us to perform analysis.Similarly,the study referenced by Damlujiet al[12]excluded patients with a creatinine of 2.0 mg/dL or higher.Flores-Umanzoret al[13]did not comment on CKD.Hopefully,further studies in the future shall enable us to look at the effect of CKD on clinical outcomes in diabetics with CTO.
It is also not clear why revascularization in CTO is beneficial and associated with improved survival rates in diabetics.CTOs are usually associated with a larger scar and most of all with a bigger border zone which causes arrhythmias and sudden cardiac death in most patients[31].Thus,it might be the beneficial effects of early revascularization in preventing the formation of scar myocardium which may lead to improvement in mortality and morbidity.It also might be worthwhile to attempt CABG instead of PCI in patients with a difficult anatomy particularly in the diabetic sub group as these patients have a lower success rate as compared to the general population and might save unnecessary side effects from an unsuccessful procedure in itself.

Figure 1 Random effects meta-analysis and forest plot of hazard ratios for all cause long term and cardiac mortality.

Figure 2 Random effects meta-analysis and forest plot of hazard ratios for repeat myocardial infarction and repeat revascularization.
Limitations
Our studies have various limitations.Because of the observational design of three out of four studies (Figures 1 and 2),there was an inherent risk of selection bias which may have affected the results through confounding factors.One of the potential explanations for the mortality benefits with ER may be potential confounders as highrisk patients are less likely to undergo ER.This was reinstated across all studies as patients assigned to OMT were older and with more co-morbidities.A major concern for selection bias in Flores-Umanzoret al[13]was the inclusion of failed PCI group into the medical therapy group as a failed PCI might itself be a risk factor for adverse events in the future.Yan and colleagues also only studied one vessel CTO but the other three studies also included more than one vessel CTO.Although this might not be significant as Flores-Umanzoret al[13]demonstrated that in majority of patients,only one vessel was diseased with the most common culprit being the right coronary artery.The selection of only PCI as revascularization modality by Choiet al[14]and Yanet al[15]also introduced bias as patients treated with CABG were not studied.Significant heterogeneity was observed in some effect outcomes,however we used sensitivity analysis to analyze which study was causing the effect and recalculated data after dropping the study.Also,as with all met-analysis,the quality of the study is as good as the quality of the trials itself.
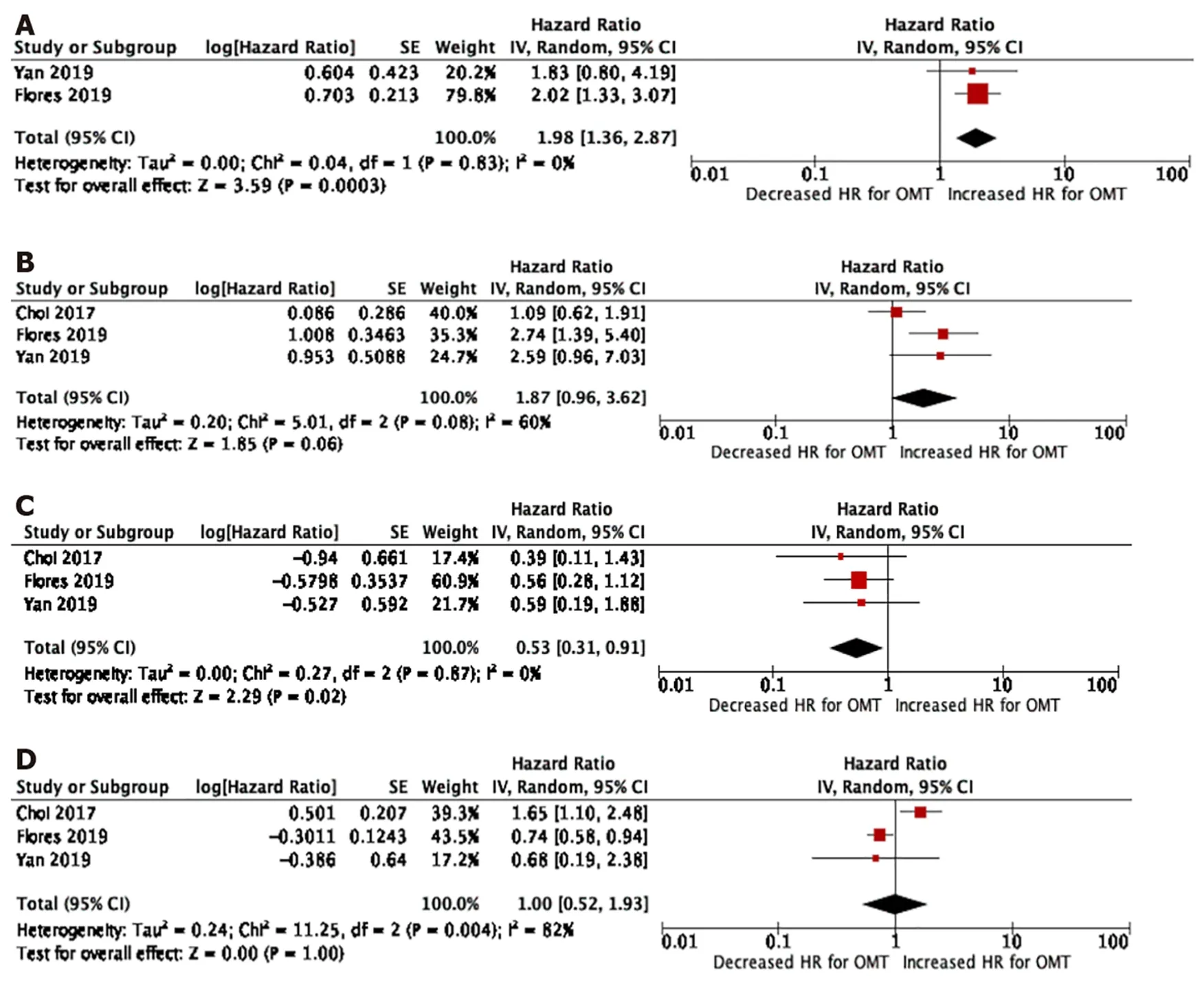
Figure 3 Sub-group analysis and forest plot of hazard ratios for all-cause and cardiac mortality,repeat mi and repeat revascularization.
CONCLUSION
Despite our limitations,we report the results of the first meta-analysis specifically done on diabetic patients with CTO lesions treated with OMTvsER.The results reveal a trend towards superiority of the ER group (PCI and CABG) to OMT in terms of all cause and cardiac death although we could not achieve statistical significance.These findings were reinforced on subgroup analysis of OMTvsPCI,specifically regards to all-cause death where the results were statistically significant.However,patients undergoing PCI had a higher risk of repeat fatal and non-fatal MI as compared to OMT and the risk for repeat revascularization was similar in both groups.Overall patients in the OMT only group had a higher risk of repeat revascularization as compared to ER group (PCI and CABG).In patients with extensive CAD and CTO,CABG may be attempted as PCI in diabetics has a higher risk of failure as compared to non-diabetics.Further data including larger patient population from future studies is needed to clarify outcome benefits from revascularization or medical therapy in these patients.
ARTICLE HIGHLIGHTS
Research background
The thought process behind this manuscript was our motivation upon literature review of a scarcity of data involving clinical outcomes of diabetics with chronic total occlusion (CTO) of coronary vessels.
Research motivation
Our motivation came from the scarcity of data in this sub group of population.There exists a lot of literature comparing the mortality and morbidity outcomes of medical therapy (OMT) vs early re-vascularization [ER:Percutaneous coronary intervention(PCI) + Coronary artery bypass grafting] in patients with chronic total occlusions but none in the diabetic subset.
Research objectives
To compare the mortality and morbidity outcomes in diabetic population with CTO treated with OMT vs ER.
Research methods
Multiple electronic data-bases including Pubmed,Embase were searched involving human studies comparing OMT vs ER in patients having CTO of coronary vessels.Data was analyzed using Cochrane review manager with hazard ratios using the random effects model.Primary effect estimate was all cause mortality with secondary effect estimates as cardiac mortality,repeat myocardial infarction (MI) and repeat revascularization.
Research results
Statistical analysis revealed a higher risk for all-cause mortality,cardiac mortality and repeat re-vascularization in the OMT group.For repeat MI,data analysis revealed no significant differences in between the two groups.Sub-group analysis was also done for OMT vs PCI.This revealed a higher risk for all-cause mortality but not for cardiac mortality or repeat re-vascularization in the OMT group.Interestingly,patients in the OMT group were found to have a lower incidence of repeat MI vs PCI group.
Research conclusions
There is a trend towards superiority of the ER group as compared to OMT group in diabetic patients with a CTO.These findings were reinforced on sub-group analysis of OMT vs PCI.
Research perspectives
Despite our limitations,we present the first ever meta-analysis specifically involving diabetic patients only with CTO treated with OMT or ER.Although we were able to demonstrate a trend towards superiority of the ER group,this was not statistically significant for some sub-groups including all-cause and cardiac mortality.Although this manuscript provides a relatively new insight into management of such patients,further studies may be needed before a consensus is developed.
杂志排行
World Journal of Cardiology的其它文章
- Effectiveness and safety of antithrombotic strategies in elderly patients with acute myocardial infarction
- Endothelial progenitor cells mobilization after maximal exercise according to heart failure severity
- Rapid right ventricular pacing for balloon valvuloplasty in congenital aortic stenosis:A systematic review
- Effects of left ventricular assist device on pulmonary functions and pulmonary hemodynamics:A meta-analysis
- Transradial vs transfemoral secondary access outcomes in transcatheter aortic valve implantation:A systematic review and meta-analysis
- Cardiac adverse events of immune checkpoint inhibitors in oncology patients:A systematic review and meta-analysis
