Intussusception due to hematogenous metastasis of hepatocellular carcinoma to the small intestine: A case report
2020-12-11TaroMashikoYoshihitoMasuokaAkiraNakanoKotaTsuruyaShunjiHiroseKenichiHirabayashiTatehiroKagawaToshioNakagohri
Taro Mashiko, Yoshihito Masuoka, Akira Nakano, Kota Tsuruya, Shunji Hirose, Kenichi Hirabayashi, Tatehiro Kagawa, Toshio Nakagohri
Abstract
Key Words: Hepatocellular carcinoma; Hematogenous metastases; Extrahepatic metastasis; Small intestinal metastasis; Intussusception; Case report
INTRODUCTION
Hepatocellular carcinoma (HCC) is a highly prevalent disease and accounts for 800000 deaths per year globally[1]. Despite the development of novel treatment modalities and newer surgical instruments, the long-term outcomes of HCC are not satisfactory because of high rates of recurrence and metastasis. Intrahepatic metastasis is the most common recurrence pattern of HCC, accounting for approximately 85%-90% of cases[2,3]. Extrahepatic metastases have been reported in 13%-64% of HCC patients, with the lungs, bones, adrenal glands, and regional lymph nodes as the commonest sites of metastases[4-6]. Metastasis of HCC to the gastrointestinal (GI) tract is infrequent, and the distant hematogenous metastasis of HCC to the small intestine is extremely unusual. We report, herein, a case of intussusception due to hematogenous metastasis of HCC to the ileum.
CASE PRESENTATION
Chief complaints
A 71-year-old man was admitted to our hospital with chief complaints of abdominal pain and vomiting.
History of present illness
A 71-year-old man was on treatment for chronic hepatitis B for 22 years when he was diagnosed with HCC. He was noted to have tumor nodules of size 20 mm in diameter, located in segment 8, on a follow-up abdominal computed tomography (CT) (Figure 1) and had undergone partial liver resection 7 years previously. Based on the 8th Union for International Cancer Control classification of HCC, the tumor was classified as pT1N0M0 stage 1. Seven months after the first surgery, abdominal CT revealed recurrent HCC with nodules 10 mm in diameter, in segment 6 of the liver (Figure 2A). When laparotomy was performed, a peritoneal mass was found that was not apparent preoperatively; therefore, partial liver resection and peritoneal tumor resection were performed (Figure 2B and C). The peritoneal tumor with peritoneal metastasis of HCC was diagnosed based on histopathological findings. Fourteen months after the first surgery, abdominal CT revealed a tumor nodule 32 mm in diameter in the pelvis, which was diagnosed as a peritoneal recurrence of HCC (Figure 3A). We determined that the recurrent tumor was solitary and decided to perform tumor resection. However, many small peritoneal nodules were found at the time of laparotomy, and radical resection was impossible (Figure 3B). Subsequently, the patient was followed up by the department of gastroenterology of our hospital, and 16 mo after the initial resection of HCC, administration of sorafenib of 400 mg/d was started. Since he developed a grade 2 hand-foot syndrome, the dosage was reduced to 200 mg/d. The administration was continued for 54 mo without any other major adverse events, and the disease was well controlled. Seventy months after the first surgery, he was admitted to our hospital with chief complaints of abdominal pain and vomiting.

Figure 1 Abdominal contrast-enhanced computed tomography before the first surgery. Arterial phase of abdominal contrast-enhanced computed tomography before the first surgery showed a tumor nodule 20 mm in diameter with early staining located in segment 8 of the liver (orange circle).
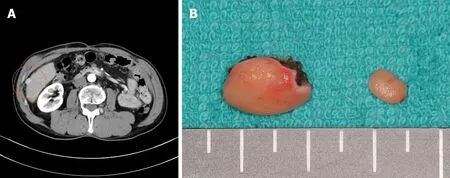
Figure 2 Abdominal contrast-enhanced computed tomography and the surgical specimen from the second surgery. A: Arterial phase of abdominal contrast-enhanced computed tomography before the second surgery showed a tumor 10 mm in diameter, located in segment 6 (orange circle), and protruding to the surface of the liver with early staining; B: Surgical specimen of the liver tumor and peritoneal tumor at the second surgery.
History of past illness
The patient’s history was significant for extensive gastrectomy for duodenal ulcer at the age of 22 years. In addition, he had a history of hypertension since the age of 65, for which he was on treatment with amlodipine besilate (10 mg/d) and azilsartan (20 mg/d).
Personal and family history
The patient’s social history consisted of a 40-pack year history and an alcohol intake of 350 mL beer per day. He had discontinued smoking and drinking alcohol 10 years previously. There was no history of cancer or liver disease in his family.
Physical examination
The height and weight of the patient at admission were 172 cm and 52 kg,respectively. There were no abnormalities in the vital signs. The abdomen wassoft and slightly swollen. Tenderness was noted in the right lower abdomen.

Figure 3 Abdominal contrast-enhanced computed tomography before the third surgery and the intraoperative findings. A: Abdominal contrast-enhanced computed tomography showed a tumor 32 mm in diameter in the pelvis (orange circle); B: Many small peritoneal nodules were found at the time of laparotomy.
Laboratory examinations
No abnormal findings were found other than a high C-reactive protein level (4.95 mg/dL) in blood biochemical tests. Liver function tests revealed a class A Child-Pugh score.
Imaging examinations
Abdominal contrast-enhanced CT revealed a well-defined, rounded, enhancing endoluminal tumor in the small intestine, leading to intussusception and small bowel obstruction (Figure 4). An ileus tube was inserted to decompress the small intestine.
FINAL DIAGNOSIS
On the basis of these findings, the diagnosis was a small intestinal tumor (primary or metastasis), which had caused the intussusception and small bowel obstruction.
TREATMENT
Initially, conservative treatment was initiated because of the peritoneal dissemination of HCC. X-ray examination after contrast infusion through the ileus tube showed no tumor or stenosis in the small intestine other than that at the intussusception site. The patient had fluctuating symptoms, and surgery was planned on the 28thd of hospitalization. During surgery, the intussusception site was found 130 cm distal to the ligament of Treitz. We performed partial ileal resection without reduction of the intussusception, followed by end-to-end anastomosis (Figure 5A). The resected specimen showed a polypoid tumor of size 50 mm protruding into the lumen (Figure 5B).
OUTCOME AND FOLLOW-UP
The postoperative period was uneventful, and the patient was discharged on the 18thpostoperative day. The histological examination revealed tumor cells with a cytoplasm rich in eosinophilic granules, enlarged nuclei, and distinct nucleoli that showed dense proliferation in the lesion (Figure 6A). No tumor cells were observed on the serosal surface, but intravascular invasion of tumor cells was observed (Figure 6B). Immunohistochemistry was positive for alpha-fetoprotein (AFP), Hep Par1, and Glypican3[7], and a diagnosis of hematogenous metastasis of HCC to the ileum was made (Figure 6C-E). Since right adrenal metastasis was found on a follow-up abdominal CT 78 mo after the first surgery, administration of Lenvatinib of 8 mg/d was started. The patient continues to survive 82 mo after the initial surgery without any major adverse events of Lenvatinib.
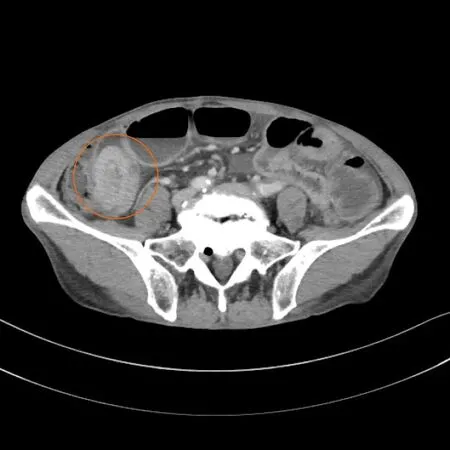
Figure 4 Abdominal contrast-enhanced computed tomography demonstrated an intussusception of the small intestine due to a welldefined, rounded, enhancing endoluminal mass (orange circle).

Figure 5 Intraoperative findings and the resected specimen. A: The intussusception site was found 130 cm distal to the ligament of Treitz; B: The resected specimen showed a polypoid tumor 50 mm in diameter protruding into the lumen.
DISCUSSION
HCC is one of the most common malignancies globally, and its incidence has been increasing in the recent years. The long-term outcomes of HCC are disappointing because of the high rates of recurrence and metastasis. In an autopsy series, GI involvement of HCC was found in only 4%-12% of cases[8,9]. The metastasis of HCC to the GI tract is mostly through direct invasion to the adjacent GI tractviaadhesion to the serosal side. The most frequently involved sites are the duodenum, stomach, hepatic flexure of the colon, and jejunum.
Parket al[10]reported that the modes of metastases were direct invasion of contiguous HCC (66.7%), hematogenous metastasis (16.7%), and peritoneal dissemination (5.6%). Thus, another mode of metastasis of HCC to the GI tract comprises the hematogenous spread. This is caused by tumor thrombosis and invasionviathe portal system, and is disseminated by the hepatofugal portal blood flow to the GI tract. According to the literature, the interval between diagnosis of HCC and detection of the GI tract involvement ranged from 3 mo to 8 years[11,12]. Metastatic lesions in the small intestine are usually asymptomatic and are not easily discovered. GI metastasis is mostly found in HCC patients with an advanced stage, and it has a poor prognosis, with a median survival period of 7 mo[5].
In our patient, the serosal side of the ileum was free from tumor cells, and intravascular invasion of tumor cells was observed. Hence, we diagnosed that hematogenous metastasis to the ileum had occurred and it had spread in the lumen. Unlike previous reports, the tumor size of HCC was not large, and portal vein thrombosis was not detected at both the primary HCC and recurrent HCC stage. However, peritoneal dissemination was observed during the second surgery, and recurrence occurred relatively early after the first surgery. On the contrary, metastasis to the ileum occurred 70 mo after the first surgery. It was determined that disease control was good with sorafenib, a multikinase inhibitor with antiproliferative, antiangiogenic, and proapoptotic properties.

Figure 6 Histopathological findings and immunohistochemistry. A: Histological findings showed tumor cells with cytoplasm rich in eosinophilic granules, enlarged nuclei, and clear nucleoli that showed dense proliferation on hematoxylin and eosin staining (× 400); B: Intravascular invasion of tumor cells were observed on Victoria blue staining (× 40); C: Alpha-fetoprotein (AFP) positive cells were observed on immunostaining (× 400); D: Hep Par1 positive cells were observed on immunostaining (× 400); E: Glypican3 positive cells were observed on immunostaining (× 400).
Intussusception is common in children, whereas it is a rare condition in adults, who account for only 5% of the cases of intussusceptions. It is a rare cause of intestinal obstruction in adults (< 1% cases)[13,14]. According to the etiology of adult intussusception, the rates of malignant tumor, benign tumor, and idiopathic causes were 32.9%, 37.4%, and 15.1%, respectively[15]. Breast cancer, lung cancer, and malignant melanoma are reported to be the major causes of small bowel obstruction due to metastatic tumors[16]. Reports of intussusception and small bowel obstruction due to small intestinal metastasis of HCC are extremely rare. Based on the review of previously published studies, there are only two cases reported so far, including our own case[17].
Surgical treatment of extrahepatic metastasis of HCC has still not been established. The prognosis of patients at this stage continues to be poor due to limited effective treatment options. However, despite the limited number of cases, it has been reported that the prognosis improved after surgical resection of isolated extrahepatic metastases of HCC. Resection of isolated lung metastasis of HCC has been reported to improve prognosis in selective patients. Takahashiet al[18]reported that disease-free interval of more than 12 mo was significantly associated with favorable outcomes in both overall survival (5-year rate, 59.3%vs28.7%;P= 0.026) and disease-specific survival (5-year rate, 62.5%vs36.2%;P= 0.038) in patients who underwent pulmonary resection. Chanet al[19]reported that surgical resection of extrahepatic metastasis from HCC should be considered in patients with one or two isolated extrahepatic metastases if they had a good performance status, good liver function, and well-controlled intrahepatic HCC. Ukaet al[20]also reported that in the treatment of patients with extrahepatic metastases of HCC, relieving portal venous invasion may improve survival. Chuaet al[21]suggested that when resection of extrahepatic metastasis of HCC is performed, it should be combined with the most effective systemic therapy that is currently available.
In general, GI metastasis of HCC has a poor prognosis. However, as in this case, extrahepatic metastasis can occur even in patients with an early tumor stage and negative portal vein invasion or occlusion. Since good disease control of intrahepatic lesions and metastatic lesions was accomplished by systemic chemotherapy, and because of the long interval before the patient developed small intestinal metastasis, it is considered that the patient achieved long-term survival due to multidisciplinary therapy.
CONCLUSION
We herein report an extremely rare case of intussusception due to hematogenous metastasis of HCC to the ileum. Even if the prognosis of patients with GI tract metastasis of HCC is poor, selected patients may have prolonged survival because of multidisciplinary therapy including surgical resection.
杂志排行
World Journal of Gastroenterology的其它文章
- Nonalcoholic fatty liver disease in lean subjects: Prognosis, outcomes and management
- Modern surgical strategies for perianal Crohn's disease
- Simultaneous colorectal and parenchymal-sparing liver resection for advanced colorectal carcinoma with synchronous liver metastases: Between conventional and mini-invasive approaches
- Estimation of visceral fat is useful for the diagnosis of significant fibrosis in patients with non-alcoholic fatty liver disease
- Nomograms and risk score models for predicting survival in rectal cancer patients with neoadjuvant therapy
- Attention deficit hyperactivity disorder and gastrointestinal morbidity in a large cohort of young adults